Abstract
Purpose
The number of arthroscopic knee surgeries performed annually has increased over the last decade. It remains unclear what proportion of individuals undergoing knee arthroscopy is at risk for subsequent ipsilateral procedures. Better knowledge of risk factors and the incidence of reoperative ipsilateral arthroscopy are important in setting expectations and counselling patients on treatment options. The aim of this study is to determine the incidence of repeat ipsilateral knee arthroscopy, and the risk factors associated with subsequent surgery over long-term follow-up.
Methods
The New York Statewide Planning and Research Cooperative Systems outpatient database was reviewed from 2003 to 2016 to identify patients who underwent elective, primary knee arthroscopy for one of the following diagnosis-related categories of procedures: Group 1: cartilage repair and transfer; Group 2: osteochondritis dissecans (OCD) lesions; Group 3: meniscal repair, debridement, chondroplasty, and synovectomy; Group 4: multiple different procedures. Subjects were followed for 10 years to determine the odds of subsequent ipsilateral knee arthroscopy. Risk factors including the group of arthroscopic surgery, age group, gender, race, insurance type, surgeon volume, and comorbidities were analysed to identify factors predicting subsequent surgery.
Results
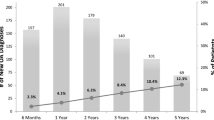
A total of 765,144 patients who underwent knee arthroscopy between 2003 and 2016, were identified. The majority (751,873) underwent meniscus-related arthroscopy. The proportion of patients undergoing subsequent ipsilateral knee arthroscopy was 2.1% at 1-year, 5.5% at 5 years, and 6.7% at 10 years of follow-up. Among patients who underwent subsequent arthroscopic surgery at 1-, 5-, and 10-year follow-up, there was a greater proportion of patients with worker’s compensation insurance (p < 0.001), index operations performed by very high volume surgeons (p < 0.001), and cartilage restoration index procedures (p < 0.001), compared with those who never underwent repeat ipsilateral surgery.
Conclusion
Understanding the incidence of subsequent knee arthroscopy after index procedure in different age groups and the patterns over 10 years of follow-up is important in counselling patients and setting future expectations. The majority of subsequent surgeries occur within the first 5 years after index surgery, and subjects tend to have higher odds of ipsilateral reoperation for up to 10 years if they have worker’s compensation insurance, or if their index surgery was performed by a very high volume surgeon, or was a cartilage restoration procedure.
Level of evidence
III.
Similar content being viewed by others
References
Boyd JA, Gradisar IM (2016) Total knee arthroplasty after knee arthroscopy in patients older than 50 years. Orthopedics 39:e1041–e1044
Bursac Z, Gauss CH, Williams DK, Hosmer DW (2008) Purposeful selection of variables in logistic regression. Source Code Biol Med 3:17
Cullen KA, Hall MJ, Golosinskiy A (2009) Ambulatory surgery in the United States, 2006. Natl Health Stat Rep (11):1–25
Doral MN, Bilge O, Huri G, Turhan E, Verdonk R (2018) Modern treatment of meniscal tears. EFORT Open Rev 3:260–268
Frank RM, Lee S, Levy D, Poland S, Smith M, Scalise N et al (2017) Osteochondral allograft transplantation of the knee: analysis of failures at 5 years. Am J Sports Med 45:864–874
Frank RM, McCormick F, Rosas S, Amoo-Achampong K, Erickson B, Bach BR Jr et al (2018) Reoperation rates after cartilage restoration procedures in the knee: analysis of a large US commercial database. Am J Orthop (Belle Mead NJ) 47:1–15
Gundle KR, McGlaston TJ, Ramappa AJ (2010) Effect of insurance status on the rate of surgery following a meniscal tear. J Bone Joint Surg Am 92:2452–2456
Hawker G, Guan J, Judge A, Dieppe P (2008) Knee arthroscopy in England and Ontario: patterns of use, changes over time, and relationship to total knee replacement. J Bone Joint Surg Am 90:2337–2345
Jameson SS, Dowen D, James P, Serrano-Pedraza I, Reed MR, Deehan DJ (2011) The burden of arthroscopy of the knee: a contemporary analysis of data from the English NHS. J Bone Joint Surg Br 93:1327–1333
Khan M, Evaniew N, Bedi A, Ayeni OR, Bhandari M (2014) Arthroscopic surgery for degenerative tears of the meniscus: a systematic review and meta-analysis. CMAJ 186:1057–1064
Lubowitz JH, Appleby D (2011) Cost-effectiveness analysis of the most common orthopaedic surgery procedures: knee arthroscopy and knee anterior cruciate ligament reconstruction. Arthroscopy 27:1317–1322
Mahure SA, Mollon B, Shamah SD, Zuckerman JD, Kwon YW, Rokito AS (2016) The incidence of subsequent surgery after outpatient arthroscopic rotator cuff repair. Arthroscopy 32:1531–1541
McCormick F, Harris JD, Abrams GD, Hussey KE, Wilson H, Frank R et al (2014) Survival and reoperation rates after meniscal allograft transplantation: analysis of failures for 172 consecutive transplants at a minimum 2-year follow-up. Am J Sports Med 42:892–897
Mickey RM, Greenland S (1989) The impact of confounder selection criteria on effect estimation. Am J Epidemiol 129:125–137
Montgomery SR, Foster BD, Ngo SS, Terrell RD, Wang JC, Petrigliano FA et al (2014) Trends in the surgical treatment of articular cartilage defects of the knee in the United States. Knee Surg Sports Traumatol Arthrosc 22:2070–2075
Patel AA, Singh K, Nunley RM, Minhas SV (2016) Administrative databases in orthopaedic research: pearls and pitfalls of big data. J Am Acad Orthop Surg 24:172–179
Salzler MJ, Lin A, Miller CD, Herold S, Irrgang JJ, Harner CD (2014) Complications after arthroscopic knee surgery. Am J Sports Med 42:292–296
Suchman KI, Behery OA, Mai DH, Anil U, Bosco JA (2018) The demographic and geographic trends of meniscal procedures in New York State: an analysis of 649,470 patients over 13 years. J Bone Joint Surg Am 100:1581–1588
Wylie JD, Hartley MK, Kapron AL, Aoki SK, Maak TG (2016) Failures and reoperations after matrix-assisted cartilage repair of the knee: a systematic review. Arthroscopy 32:386–392
Funding
No internal or external funding sources were used to conduct this study.
Author information
Authors and Affiliations
Contributions
OB reviewed the analysed data, all the relevant literature, statistical results, drafted the manuscript and made any necessary edits as part of the review process. KS assisted with gathering the literature review for the paper and formatting the references. AP was involved with SPARCS dataset management and statistical analysis for hypothesis testing. TL contributed to manuscript writing as well as editing process. KC reviewed the manuscript drafts and contributed to the editing and review process. JB senior author for this study, who developed the research question, hypotheses and guided the editing/review process.
Corresponding author
Ethics declarations
Conflict of interest
There are no relevant disclosures, relationships, conditions or circumstances to report that may represent potential conflict of interest in this study.
Ethical approval
This research represents an analysis of the large and public Statewide Planning and Research Cooperative System (SPARCS) database, which contains no patient identifiers and is exempt from the institutional review board (IRB) process.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Behery, O.A., Suchman, K.I., Paoli, A.R. et al. What are the prevalence and risk factors for repeat ipsilateral knee arthroscopy?. Knee Surg Sports Traumatol Arthrosc 27, 3345–3353 (2019). https://doi.org/10.1007/s00167-019-05348-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-019-05348-y