Abstract
Purpose
To determine the clinical and radiographic efficacy of chitosan-glycerol phosphate/blood implant versus hyaluronic acid-based cell-free scaffold in patients with focal osteochondral lesion of the knee joint.
Methods
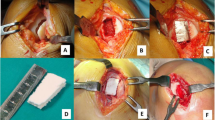
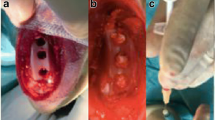
Clinical data of 46 patients surgically treated using either chitosan-glycerol phosphate/blood implant (25 patients, Group 1) or hyaluronic acid-based cell-free scaffold (21 patients, Group 2) in combination with microfracture were retrospectively evaluated. All lesions were Outerbridge grade III or IV with a mean lesion size of 3.3 ± 0.7 cm2. The mean follow-up time was 24.4 months. Visual analogue scale (VAS), Lysholm knee score, and Tegner activity scale were the instruments to evaluate the clinical status. Magnetic resonance observation of cartilage repair tissue (MOCART) system was used to analyze the characteristics of repair tissue.
Results
No significant differences were detected between the groups regarding VAS, Lysholm, and Tegner scores at any time interval during the whole follow-up. The mean post-operative VAS and Lysholm scores at the latest follow-up was significantly better in cases with the lesion size ≤ 3 cm2 in Group 1 (p = 0.001, p < 0.001, respectively). However, no significant differences according to the lesion size were detected in Group 2 (n.s.). Complete repair with the filling of the defect was achieved in 7 (28%) of the knees in Group 1 and it was 7 (33.3%) of the knees in Group 2 according to MOCART system at the latest follow-up.
Conclusion
Single-stage regenerative cartilage surgery using chitosan-glycerol phosphate/blood implant combined to microfracture for focal osteochondral lesions of the knee revealed similar clinical and radiographic outcomes with hyaluronic acid-based cell-free scaffold at short-term follow-up. However, clinical outcomes of hyaluronan scaffold were less sensitive to defect size than chitosan. With the advantages of no hypertrophic repair tissue formation as well as no need to arthrotomy during surgery, chitosan is an effective choice especially in patients with the lesion size ≤ 3 cm2.
Level of evidence
III.


Similar content being viewed by others
References
Angele P, Fritz J, Albrecht D, Koh J, Zellner J (2015) Defect type, localization and marker gene expression determines early adverse events of matrix-associated autologous chondrocyte implantation. Injury 46(Suppl 4):2–9
Bark S, Piontek T, Behrens P, Mkalaluh S, Varoga D, Gille J (2014) Enhanced microfracture techniques in cartilage knee surgery: fact or fiction? World J Orthop 5(4):444–449
Becher C, Ettinger M, Ezechieli M, Kaps C, Ewig M, Smith T (2015) Repair of retropatellar cartilage defects in the knee with microfracture and a cell-free polymer-based implant. Arch Orthop Trauma Surg 135(7):1003–1010
Benthien JP, Behrens P (2010) Autologous matrix-induced chondrogenesis (AMIC). A one-step procedure for retropatellar articular resurfacing. Acta Orthop Belg 76(2):260–263
Berta A, Duska Z, Toth F, Hangody L (2015) Clinical experiences with cartilage repair techniques: outcomes, indications, contraindications and rehabilitation. Eklem Hastalik Cerrahisi 26(2):84–96
Blisard BR (2013) Lesion size should not be a limitation for microfracture surgery. Orthopedics Today 33(10):p32
Delcogliano M, de Caro F, Scaravella E, Ziveri G, De Biase CF (2014) Use of innovative biomimetic scaffold in the treatment for large osteochondral lesions of the knee. Knee Surg Sports Traumatol Arthrosc 22(6):1260–1269
Filardo G, Kon E, Roffi A, Di Martino A, Marcacci M (2013) Scaffold-based repair for cartilage healing: a systematic review and technical note. Arthroscopy 29(1):174–186
Gobbi A, Karnatzikos G, Kumar A (2014) Long-term results after microfracture treatment for full-thickness knee chondral lesions in athletes. Knee Surg Sports Traumatol Arthrosc 22(9):1986–1996
Kusano T, Jakob RP, Gautier E, Magnussen RA, Hoogewoud H, Jacobi M (2012) Treatment of isolated chondral and osteochondral defects in the knee by autologous matrix-induced chondrogenesis (AMIC). Knee Surg Sports Traumatol Arthrosc 20(10):2109–2115
Kon E, Roffi A, Filardo G, Tesei G, Marcacci M (2015) Scaffold-based cartilage treatments: with or without cells? A systematic review of preclinical and clinical evidence. Arthroscopy 31(4):767–775
Lach M, Trzeciak T, Richter M, Pawlicz J, Suchorska WM (2014) Directed differentiation of induced pluripotent stem cells into chondrogenic lineages for articular cartilage treatment. J Tissue Eng 5:2041731414552701
Lee YH, Suzer F, Thermann H (2014) Autologous matrix-induced chondrogenesis in the knee: a review. Cartilage 5(3):145–153
Lynch TS, Patel RM, Benedick A, Amin NH, Jones MH, Miniaci A (2015) Systemic review of autogenous osteochondral transplant outcomes. Arthroscopy 31(4):746–754
Marlovits S, Singer P, Zeller P, Mandl I, Haller J, Trattnig S (2006) Magnetic resonance observation of cartilage repair tissue (MOCART) for the evaluation of autologous chondrocyte transplantation: determination of interobserver variability and correlation to clinical outcome after 2 years. Eur J Radiol 57:16–23
McNickle AG, Provencher MT, Cole BJ (2008) Overview of existing cartilage repair technology. Sports Med Arthrosc 16(4):196–201
Methot S, Changoor A, Tran-Khanh N, Hoemann CD, Stanish WD, Restrepo A, Shive MS, Buschmann MD (2016) Osteochondral biopsy analysis demonstrates that BST-CarGel treatment improves structural and cellular characteristics of cartilage repair tissue compared with microfracture. Cartilage 7(1):16–28
Nemec SF, Marlovits S, Trattnig S (2009) Persistent bone marrow edema after osteochondral autograft transplantation in the knee joint. Eur J Radiol 71(1):159–163
Oussedik S, Tsitskaris K, Parker D (2015) Treatment of articular cartilage lesions of the knee by microfracture or autologous chondrocyte implantation: a systematic review. Arthroscopy 31(4):732–744
Panseri S, Russo A, Cunha C, Bondi A, Di Martino A, Patella S, Kon E (2012) Osteochondral tissue engineering approaches for articular cartilage and subchondral bone regeneration. Knee Surg Sports Traumatol Arthrosc 20(6):1182–1191
Saw KY, Anz A, Merican S, Tay YG, Ragavanaidu K, Jee CS, McGuire DA (2011) Articular cartilage regeneration with autologous peripheral blood progenitor cells and hyaluronic acid after arthroscopic subchondral drilling: a report of 5 cases with histology. Arthroscopy 27(4):493–506
Stanish WD, McCormack R, Forriol F, Mohtadi N, Pelet S, Desnoyers J, Restrepo A, Shive MS (2013) Novel scaffold-based BST-CarGel treatment results in superior cartilage repair compared with microfracture in a randomized controlled trial. J Bone Joint Surg Am 95(18):1640–1650
Siclari A, Mascaro G, Gentili C, Cancedda R, Boux EA (2012) Cell-free scaffold-based cartilage repair provides improved function hyaline-like repair at one year. Clin Orthop Relat Res 470(3):910–919
Shive MS, Stanish WD, McCormack R, Forriol F, Mohtadi N, Pelet S, Desnoyers J, Methot S, Vehik K, Restrepo A (2015) BST-CarGel® treatment maintains cartilage repair superiority over microfracture at 5 years in a multicenter randomized controlled trial. Cartilage 6(2):62–72
Sofu H, Kockara N, Oner A, Camurcu Y, Issın A, Sahin V (2017) Results of hyaluronic acid-based cell-free scaffold application in combination with microfracture for the treatment of osteochondral lesions of the knee: 2-year comparative study. Arthroscopy 33(1):209–216
Vannini F, Battaglia M, Buda R, Cavallo M, Giannini S (2012) “One step” treatment of juvenile osteochondritis dessecans in the knee: clinical results and T2 mapping characterisation. Orthop Clin North Am 43(2):237–244
Verdonk P, Dhollander A, Almqvist KF, Verdonk R, Victor J (2015) Treatment of osteochondral lesions in the knee using a cell-free scaffold. Bone Jt J 97(3):318–323
Villa Y, Rico J, Dalmau A, Chaques FJ, Asuncion J (2014) Treatment of osteochondral lesions of the talus with bone marrow stimulation and chitosan glycerol phosphate/blood implants (BST-CarGel). Arthrosc Tech 6:e663–e667
Yanke AB, Cole BJ (2014) Microfracture: dead or the future? Orthopedics 37(12):798–800
Funding
The authors declare that there was no funding of this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was conducted in compliance with ethical standards after having IRB approval.
Rights and permissions
About this article
Cite this article
Sofu, H., Camurcu, Y., Ucpunar, H. et al. Clinical and radiographic outcomes of chitosan-glycerol phosphate/blood implant are similar with hyaluronic acid-based cell-free scaffold in the treatment of focal osteochondral lesions of the knee joint. Knee Surg Sports Traumatol Arthrosc 27, 773–781 (2019). https://doi.org/10.1007/s00167-018-5079-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-018-5079-z