Abstract
Purpose
This study aimed to investigate the results of arthroscopic treatment combined with ankle stabilization procedure for sinus tarsi syndrome (STS) in patients with chronic ankle instability (CAI).
Methods
A total of 57 patients (31 males and 26 females, average age 29.9 ± 8.4 years ranging from 15 to 52 years) with STS and CAI who accepted operation from 2013 to 2015 were included in this retrospective study. Surgical procedures included thorough tarsal sinus debridement and repair or reconstruction of lateral ankle ligaments according to the quality of ligaments. American Orthopedic Foot and Ankle Society (AOFAS) score, Karlsson score, and Tegner score were evaluated preoperatively and at final follow-up.
Results
All the patients accepted thorough debridement of tarsal sinus. Of these, 53 patients (93.0%) had an arch structure between the posterior subtalar joint and the middle subtalar joint. Further, 54 patients accepted lateral ankle ligament repair, and 3 patients accepted ligament reconstruction. A total of 40 patients were followed up with an average time of 30.7 months. The modified AOFAS score increased from 62.5 (27–90) to 93 (67–100), the Karlsson score increased from 57 (30–82) to 90 (55–100), and the Tegner score increased from 1 (1–3) to 5 (1–8).
Conclusions
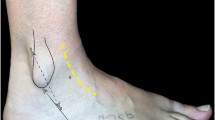
Arthroscopic treatment combined with the ankle stabilization procedure could get satisfactory results for STS in patients with CAI. The arch structure composed by medial calcaneal component of the medial root of the inferior extensor retinaculum (MCC) might contribute to the pathological mechanism of STS.
Level of evidence
IV.


Similar content being viewed by others
References
Ahn JH, Lee SK, Kim KJ, Kim YI, Choy WS (2009) Subtalar arthroscopic procedures for the treatment of subtalar pathologic conditions: 115 consecutive cases. Orthopedics 32:891
Aydıngöz Ü, Melih Topcuoğlu O, Görmez A, Cankurtaran T, Dilara Topcuoğlu E, Bilge Ergen F (2016) Accessory anterolateral talar facet in populations with and without symptoms: prevalence and relevant associated ankle MRI findings. AJR Am J Roentgenol 9:1–6
Barbaix E, Van Roy P, Clarys JP (2000) Variations of anatomical elements contributing to subtalar joint stability: intrinsic risk factors for post-traumatic lateral instability of the ankle? Ergonomics 43:1718–1725
Caputo AM, Lee JY, Spritzer CE, Easley ME, DeOrio JK, Nunley JA, DeFrate LE (2009) In vivo kinematics of the tibiotalar joint after lateral ankle instability. Am J Sports Med 37:2241–2248
Cho JH, Lee DH, Song HK, Bang JY, Lee KT, Park YU (2016) Value of stress ultrasound for the diagnosis of chronic ankle instability compared to manual anterior drawer test, stress radiography, magnetic resonance imaging, and arthroscopy. Knee Surg Sports Traumatol Arthrosc 24:1022–1028
Choisne J, Hoch MC, Alexander I, Ringleb SI (2017) Effect of direct ligament repair and tenodesis reconstruction on simulated subtalar joint instability. Foot Ankle Int 38:324–330
Frey C, Feder KS, DiGiovanni C (1999) Arthroscopic evaluation of the subtalar joint: does sinus tarsi syndrome exist? Foot Ankle Int 20:185–191
Helgeson K (2009) Examination and intervention for sinus tarsi syndrome. N Am J Sports Phys Ther 4:29–37
Hua YH, Chen SY (2010) Combination of modified Broström procedure with ankle arthroscopy for chronic ankle instability accompanied by intra-articular symptoms. Arthroscopy 26:524–528
Kamiya T, Kura H, Suzuki D, Uchiyama E, Fujimiya M, Yamashita T (2009) Mechanical stability of the subtalar joint after lateral ligament sectioning and ankle brace application: a biomechanical experimental study. Am J Sports Med 37:2451–2458
Keefe DT, Haddad SL (2002) Subtalar instability—etiology, diagnosis, and management. Foot Ankle Clin 7:577–609
Klein MA, Spreitzer AM (1993) MR imaging of the tarsal sinus and canal: normal anatomy, pathologic findings, and features of the sinus tarsi syndrome. Radiology 186:233–240
Lee KB, Bai LB, Song EK, Jung ST, Kong IK (2008) Subtalar arthroscopy for sinus Tarsi syndrome: arthroscopic findings and clinical outcomes of 33 consecutive cases. Arthroscopy 24:1130–1134
Matsui K, Burgesson B, Takao M, Stone J, Guillo S, Glazebrook M (2016) Minimally invasive surgical treatment for chronic ankle instability: a systematic review. Knee Surg Sports Traumatol Arthrosc 24:1040–1048
O’Connor D (1958) Sinus tarsi syndrome: a clinical entity. J Bone Joint Surg Am 40:720
Oloff LM, Schulhofer SD, Bocko AP (2001) Subtalar joint arthroscopy for sinus tarsi syndrome: a review of 29 cases. J Foot Ankle Surg 40:152–157
Pellegrini MJ, Glisson RR, Wurm M, Ousema PH, Romash MM, Nunley JA, Easley ME (2016) Systematic quantification of stabilizing effects of subtalar joint soft-tissue constraints in a novel cadaveric model. J Bone Joint Surg Am 98:842–848
Pieters RS, Galvin J (2015) The rare presentation of sinus tarsi syndrome secondary to metastasis in a patient with endometrial carcinoma. Radiol Case Rep 6:414
Ringleb SI, Udupa JK, Siegler S, Imhauser CW, Hirsch BE, Liu J, Odhner D, Okereke E, Roach N (2005) The effect of ankle ligament damage and surgical reconstructions on the mechanics of the ankle and subtalar joints revealed by three-dimensional stress MRI. J Orthop Res 23:743–749
Weindel S, Schmidt R, Rammelt S, Claes L, Campe A, Rein S (2010) Subtalar instability: a biomechanical cadaver study. Arch Orthop Trauma Surg 130:313–319
Yamamoto H, Yagishita K, Ogiuchi T, Sakai H, Shinomiya K, Muneta T (1998) Subtalar instability following lateral ligament injuries of the ankle. Injury 29:265–268
Zwipp H, Bemmerl JG, Holch M et al (1991) Sinus tarsi and canalis tarsi syndromes. A post-traumatic entity. Foot Ankle Surg 2:181–188
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Funding
The study was supported by National Natural Science Foundation of China (NSFC81572209).
Ethical approval
Ethical approval was obtained from the Institutional Review Board (IRB) from Huashan Hospital, Fudan University: No.KY2016-002 and agreement.
Additional information
Sheng-Kun Li and Yu-Jie Song have contributed equally to this work.
Ying-Hui Hua and Hong-Yun Li have contributed equally to this work.
Rights and permissions
About this article
Cite this article
Li, SK., Song, YJ., Li, H. et al. Arthroscopic treatment combined with the ankle stabilization procedure is effective for sinus tarsi syndrome in patients with chronic ankle instability. Knee Surg Sports Traumatol Arthrosc 26, 3135–3139 (2018). https://doi.org/10.1007/s00167-017-4813-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-017-4813-2