Abstract
Purpose
To determine the influence of anatomical features of both the tibia and femur on quantitative pivot shift of anterior cruciate ligament (ACL)-injured patients.
Methods
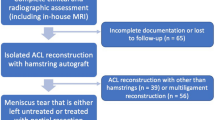
Fifty-three consecutive ACL-injured patients (mean age 26 ± 10.1 years, 36 males) who underwent ACL reconstruction were prospectively enrolled. Two blinded observers measured the parameters of medial and lateral tibial slope, femoral condyle width, notch width, bicondylar width and tibial plateau width on magnetic resonance imaging. The same examiner performed pivot shift under anaesthesia, while a previously validated image analysis technique was used to quantify knee kinematics during examination. The median lateral compartment translation detected during pivot shift testing (2.8 mm) was used to classify patients into “low-grade rotatory laxity” (≤2.8 mm) and “high-grade rotatory laxity” (>2.8 mm) groups.
Results
Twenty-nine subjects were grouped as “low-grade rotatory laxity”, and 24 subjects were grouped as “high-grade rotatory laxity”. Of the tested bone morphologic parameters, lateral tibial plateau slope was significantly greater in “high-grade rotatory laxity” group (9.3° ± 3.4°) compared to “low-grade rotatory laxity” group (6.1° ± 3.7°) (p < 0.05). Lateral tibial plateau slope was a significant predictor of “high-grade rotatory laxity” (odds ratio 1.27, p < 0.05). A tibial slope of 9° and greater predicted “high-grade rotatory laxity” (sensitivity 63 %; specificity 72 %).
Conclusion
Increased slope of the lateral tibial plateau might be an important anatomical variable predicting high-grade rotatory laxity in patients with ACL injury. The finding can be useful in the clinical setting in predicting potential non-copers to conservative therapy and aid in the individualization of the reconstructive procedures of patients.
Level of evidence
Prospective diagnostic study, Level II.



Similar content being viewed by others
References
Ayeni OR, Chahal M, Tran MN, Sprague S (2012) Pivot shift as an outcome measure for ACL reconstruction: a systematic review. Knee Surg Sports Traumatol Arthrosc 20(4):767–777
Bedi A, Musahl V, Lane C, Citak M, Warren RF, Pearle AD (2010) Lateral compartment translation predicts the grade of pivot shift: a cadaveric and clinical analysis. Knee Surg Sports Traumatol Arthrosc 18(9):1269–1276
Boden BP, Dean GS, Feagin JA Jr, Garrett WE Jr (2000) Mechanisms of anterior cruciate ligament injury. Orthopedics 23(6):573–578
Boden BP, Sheehan FT, Torg JS, Hewett TE (2010) Noncontact anterior cruciate ligament injuries: mechanisms and risk factors. J Am Acad Orthop Surg 18(9):520–527
Brandon ML, Haynes PT, Bonamo JR, Flynn MI, Barrett GR, Sherman MF (2006) The association between posterior-inferior tibial slope and anterior cruciate ligament insufficiency. Arthroscopy 22(8):894–899
Fening SD, Kovacic J, Kambic H, McLean S, Scott J, Miniaci A (2008) The effects of modified posterior tibial slope on anterior cruciate ligament strain and knee kinematics: a human cadaveric study. J Knee Surg 21(3):205–211
Fluss R, Faraggi D, Reiser B (2005) Estimation of the Youden Index and its associated cutoff point. Biom J 47(4):458–472
Frobell RB, Roos EM, Roos HP, Ranstam J, Lohmander LS (2010) A randomized trial of treatment for acute anterior cruciate ligament tears. N Engl J Med 363(4):331–342
Hashemi J, Chandrashekar N, Mansouri H, Gill B, Slauterbeck JR, Schutt RC Jr, Dabezies E, Beynnon BD (2010) Shallow medial tibial plateau and steep medial and lateral tibial slopes: new risk factors for anterior cruciate ligament injuries. Am J Sports Med 38(1):54–62
Hoshino Y, Araujo P, Ahlden M, Moore CG, Kuroda R, Zaffagnini S, Karlsson J, Fu FH, Musahl V (2012) Standardized pivot shift test improves measurement accuracy. Knee Surg Sports Traumatol Arthrosc 20(4):732–736
Hoshino Y, Araujo P, Ahlden M, Samuelsson K, Muller B, Hofbauer M, Wolf MR, Irrgang JJ, Fu FH, Musahl V (2013) Quantitative evaluation of the pivot shift by image analysis using the iPad. Knee Surg Sports Traumatol Arthrosc 21(4):975–980
Hudek R, Schmutz S, Regenfelder F, Fuchs B, Koch PP (2009) Novel measurement technique of the tibial slope on conventional MRI. Clin Orthop Relat Res 467(8):2066–2072
Kaplan Y (2011) Identifying individuals with an anterior cruciate ligament-deficient knee as copers and noncopers: a narrative literature review. J Orthop Sports Phys Ther 41(10):758–766
Kocher MS, Steadman JR, Briggs KK, Sterett WI, Hawkins RJ (2004) Relationships between objective assessment of ligament stability and subjective assessment of symptoms and function after anterior cruciate ligament reconstruction. Am J Sports Med 32(3):629–634
Kujala UM, Nelimarkka O, Koskinen SK (1992) Relationship between the pivot shift and the configuration of the lateral tibial plateau. Arch Orthop Trauma Surg 111(4):228–229
Li Y, Hong L, Feng H, Wang Q, Zhang J, Song G, Chen X, Zhuo H (2014) Posterior tibial slope influences static anterior tibial translation in anterior cruciate ligament reconstruction: a minimum 2-year follow-up study. Am J Sports Med 42(4):927–933
Matsumoto H (1990) Mechanism of the pivot shift. J Bone Joint Surg Br 72(5):816–821
Moksnes H, Snyder-Mackler L, Risberg MA (2008) Individuals with an anterior cruciate ligament-deficient knee classified as noncopers may be candidates for nonsurgical rehabilitation. J Orthop Sports Phys Ther 38(10):586–595
Muller B, Hofbauer M, Rahnemai-Azar AA, Wolf M, Araki D, Hoshino Y, Araujo P, Debski RE, Irrgang JJ, Fu FH, Musahl V (2016) Development of computer tablet software for clinical quantification of lateral knee compartment translation during the pivot shift test. Comput Methods Biomech Biomed Eng 19(2):217–228
Musahl V, Ayeni OR, Citak M, Irrgang JJ, Pearle AD, Wickiewicz TL (2010) The influence of bony morphology on the magnitude of the pivot shift. Knee Surg Sports Traumatol Arthrosc 18(9):1232–1238
Musahl V, Citak M, O’Loughlin PF, Choi D, Bedi A, Pearle AD (2010) The effect of medial versus lateral meniscectomy on the stability of the anterior cruciate ligament-deficient knee. Am J Sports Med 38(8):1591–1597
Musahl V, Hoshino Y, Ahlden M, Araujo P, Irrgang JJ, Zaffagnini S, Karlsson J, Fu FH (2012) The pivot shift: a global user guide. Knee Surg Sports Traumatol Arthrosc 20(4):724–731
Petrigliano FA, Suero EM, Voos JE, Pearle AD, Allen AA (2012) The effect of proximal tibial slope on dynamic stability testing of the posterior cruciate ligament- and posterolateral corner-deficient knee. Am J Sports Med 40(6):1322–1328
Sonnery-Cottet B, Mogos S, Thaunat M, Archbold P, Fayard JM, Freychet B, Clechet J, Chambat P (2014) Proximal Tibial Anterior Closing Wedge Osteotomy in Repeat Revision of Anterior Cruciate Ligament Reconstruction. Am J Sports Med 42(8):1873–1880
Tanaka M, Vyas D, Moloney G, Bedi A, Pearle AD, Musahl V (2012) What does it take to have a high-grade pivot shift? Knee Surg Sports Traumatol Arthrosc 20(4):737–742
Uhorchak JM, Scoville CR, Williams GN, Arciero RA, St Pierre P, Taylor DC (2003) Risk factors associated with noncontact injury of the anterior cruciate ligament: a prospective four-year evaluation of 859 West Point cadets. Am J Sports Med 31(6):831–842
Voos JE, Suero EM, Citak M, Petrigliano FP, Bosscher MR, Citak M, Wickiewicz TL, Pearle AD (2012) Effect of tibial slope on the stability of the anterior cruciate ligament-deficient knee. Knee Surg Sports Traumatol Arthrosc 20(8):1626–1631
Vrooijink SH, Wolters F, Van Eck CF, Fu FH (2011) Measurements of knee morphometrics using MRI and arthroscopy: a comparative study between ACL-injured and non-injured subjects. Knee Surg Sports Traumatol Arthrosc 19(Suppl 1):S12–S16
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Volker Musahl, Freddie H Fu and James J Irrgang are part of the group that holds the patent for the software utilized for quantification of the pivot shift in this manuscript. Volker Musahl received funding from Smith and Nephew as an educational consultant, not related to research presented in this manuscript. Freddie H Fu, as chairman of the department of orthopaedic surgery, oversees all research funding for the department. The Department of Orthopaedic Surgery of the University of Pittsburgh receives funding from Arthrocare, Synthes, Stryker, Johnson & Johnson, DePuy, DonJoy, Breg, Omeros, Biomet, Mitek, not related to the research presented in this manuscript.
Rights and permissions
About this article
Cite this article
Rahnemai-Azar, A.A., Abebe, E.S., Johnson, P. et al. Increased lateral tibial slope predicts high-grade rotatory knee laxity pre-operatively in ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 25, 1170–1176 (2017). https://doi.org/10.1007/s00167-016-4157-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-016-4157-3