Abstract
Purpose
The aim of this study was to quantify sagittal and rotational knee laxity profiles taking into account individual influencing factors.
Methods
Linear regression models were used to determine which individual characteristics (age, height, body mass and sex) influenced the outcome in a group of 104 healthy subjects. The standardized residuals were used as individualized (corrected) laxity scores and were combined to determine knee laxity profiles.
Results
Anterior knee laxity was not influenced by individual characteristics. Rotational knee laxity was higher in females and inversely related to body mass. The correlation between anterior laxity and internal rotation scores was weak (r = 0.24, p = 0.02). The proportion of knees concerned by increased laxity scores (scores >1) was similar for anterior displacement, internal and external rotation (15 %). Only 32 % of the tested subjects showed a normal profile (score >−1 and <1) for all three directions, 33 % were concerned by hyperlaxity, 40 % by hypolaxity and 5 % by both.
Conclusions
The diversity of laxity profiles found here highlights that the interpretation of multidirectional knee laxity is complex and suggests the necessity for individualized care of knee diseases and injuries. These results contribute to the understanding of knee laxity and throw the basis for prevention strategies and improvement of treatment outcomes in injuries and diseases.
Level of evidence
Case series with no comparison groups, Level IV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Defining physiological knee laxity, i.e. the natural knee laxity of non-symptomatic and non-traumatic individuals, is a complex issue because of the wide variety of individual anatomical properties of each knee joint. Laxity has been considered to play a role in the development of knee osteoarthritis (OA) [25] and the occurrence of primary non-contact anterior cruciate ligament (ACL) injuries [22], secondary knee injuries [15] as well as worse ACL reconstruction outcomes [4, 8]. It has been shown that patients with hyperextension displayed better stability with a patellar tendon graft compared to a hamstrings tendon graft [9]. However, no data are available on physiological knee laxity. Therefore, establishing individual knee laxity profiles may be helpful to improve the prognostic and therapeutic criteria for primary and recurrent knee injuries and diseases.
Sagittal knee laxity measurements are widely used in the context of ACL injuries diagnosis [23] and reconstructions [11]. The interest to measure rotational laxities is relatively new and arose as a consequence of the discussion on the lack of rotational control provided by the technique of ACL reconstructions which were performed a decade ago [4, 10]. Data documenting normative references for physiological laxity or combined anterior and static rotational knee laxities are, however, sparse. Furthermore, interpreting static knee laxity is a complex matter. It is not only influenced by the precision of measurement devices, but also by individual variables such as gender, BMI and other anatomical factors [12, 19, 20]. Therefore, the practice of comparing laxity results between groups of individuals may be improved by using standardized laxity scores taking into account those individual variables [12].
The main purpose of the present study was to explore anterior and rotational knee laxity in a group of healthy participants and: (1) to determine which individual characteristics influence static anterior and rotational knee measurements, (2) to establish individualized laxity scores for anterior and rotational knee laxity separately and determine their distribution and (3) to describe the different physiological laxity profiles by combining both laxity measurements. The hypothesis of the present study was that anterior and rotational knee laxities are influenced by gender, height, body mass and age and are poorly correlated with each other. These results are expected to improve the understanding of physiological and pathological knee laxity.
Materials and methods
One hundred and four healthy participants (45 females, 33 ± 14 years, 168 ± 7 cm, 58 ± 7 kg; 59 males, 35 ± 12 years, 179 ± 8 cm, 76 ± 11 kg) were included in the study. They reported no history of knee injury or surgery, no other lower limb injury in the 6 months preceding the tests and, for women, no pregnancy. All participants had both knees tested for anterior and rotational joint laxity by a first experienced examiner. The first leg tested was randomized. The precision of the devices was established based on an inter-examiner test–retest design. A second experienced examiner, therefore, retested 61 participants for anterior laxity and 65 for static rotational knee laxity following the test by the first examiner. All participants signed a consent agreement. The study protocol had previously been approved by the National Ethics Committee for Research.
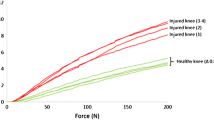
Anterior knee laxity was measured with the GNRB® with an accuracy of 0.1 mm (Fig. 1) [16], a motorized laximeter that mimics the anterior drawer test. The participant was evaluated in a supine position with the knee at 20° flexion. The joint line was placed at the edge of the thigh support. The foot was firmly fixed in neutral rotation using an ankle shell. The tested knee was then fixed with a patella shell carefully positioned so as to keep its centre aligned with the tibial axis. The fixation force applied to the knee was monitored by way of a force sensor placed under the thigh: a minimum pressure of 100 N was applied via the patella shell at the beginning of the test. Finally, the tibia displacement sensor was placed perpendicularly to the tibia on the tibial tubercle. Three separate trials were subsequently performed applying a standard anterior tibial force up to 200 N. The test was considered valid if the sensor placed under the thigh indicated a patellar fixation force above 90 N for the different trials. To permit valid side-to-side comparisons, care was taken to use a similar fixation force for both knees (≤10 N difference).
Static rotational knee laxity was measured with a previously described device with an accuracy of 0.01° (Fig. 2) [12, 21]. The foot was tightly immobilized in a ski boot of appropriate size. The subject lay prone with thighs secured in half-cone supports using Velcro straps. The ski boot was attached to the frame of the device where torques can be applied manually by the examiner through a handle bar. Progressive torques up to 5 Nm were applied for both internal rotation (IR) and external rotation (ER) tests. The starting position (set to 0° angle) of each test was taken as the natural resting position of the tested leg. Four trials were sequentially performed, first in IR then in ER. Between each trial, the handle bar was released to allow the leg to return to its resting position.
Statistical analysis
The average of the two last trials was considered for the different variables studied: anterior tibial displacement at 134 (ATD134) and 200 N (ATD200) as well as internal rotation (IR5) and external rotation (ER5) at 5 Nm. The total range of rotation at 5 Nm (TR5) was obtained by adding IR5 and ER5. To calculate the side-to-side difference (SSD = displacement of one knee − displacement of reference knee), one knee was randomly chosen as the reference knee for each subject.
Statistics were performed using version 20.0 of the SPSS software. The reproducibility and precision of the device were determined by the minimum detectable change (MDC) [26]. It represents the minimum change in a measurement that can be considered a true change. The MDC was established for both absolute and SSD values for all previously described variables. It was calculated as follows: MDC = SEM * 1.96 * √2 with the standard error of measurements (SEM) being the square root of mean square error term obtained from a repeated measures analysis of variance. To test whether age, height, body mass and sex (coded males: 0, females: 1) influence knee laxity measurements, a multiple linear regression analysis (backward method) was performed. Interactions between sex and the other variables were considered. Assumptions for linear regressions were checked. Linear relationship was confirmed with the lack of fit test of a general linear model. Normality of errors was checked with the Kolmogorov–Smirnov test. Homoscedasticity was confirmed by visual inspection of the graph representing standardized residuals versus standardized predicted values, and independence of error was assumed with the Durbin Watson test. Finally, multicollinearity was considered acceptable if the variation inflation factor was lower than 10 [14] and a value was considered as an influential outlier if its Cook’s distance was above 1 [6]. If no individual characteristics were found to be significant, the average and standard deviation values were used to calculate a z score: (observed value − average value)/standard deviation. If one or several characteristics influenced the laxity measurements, the standardized residuals of the final model were used as the laxity score. Standardized residuals indicate by how many standard deviations a value is located from the predicted value given by the model. These are computed as follows: (observed value − predicted value given by the model)/standard deviation of residuals (given by SPSS software). Based on a threshold of one [22], knees were categorized as being hypo- (score <−1), normo- (−1 <score <1) or hyperlax (score >1). Pearson’s correlations were calculated to determine the correlation between anterior and rotational laxity scores. Significance was set at p < 0.05 for all analyses.
Results
The average, standard deviation and MDC for absolute and SSD measurements are presented in Table 1 for both anterior and static rotational knee laxity. MDC for SSD was 1.5 mm for ATD200, 4.4° in IR5, 6.4° in ER and 8.2° for TR.
Potential predictors for knee laxity results included sex (45 females, 59 males), age (range 11–59), body mass (42–106 kg) and height (150–198 cm). Absolute anterior knee laxity was not significantly influenced by any of the considered individual characteristics. Average anterior displacement was 3.3 ± 0.7 mm at 134 N and 4.7 ± 0.7 mm at 200 N. Regarding rotational laxity measurements, females had significantly greater laxity than males, and body mass was negatively associated with IR5, ER5 and TR5. Assumptions of linear regression were confirmed, and neither a collinearity problem nor influential outliers could be identified. In addition, no interaction between the significant predictors could be identified. Adjusted R square, unstandardized coefficients and standard deviations of residuals are presented in Table 2. SSD results were not influenced by any considered individual characteristic, neither for anterior nor rotational knee laxity. Average SSD was 0.0 ± 0.7 mm for ATD134, 0.0 ± 0.8 mm for ATD200, −0.2 ± 2.2° for IR5, −0.7 ± 3.7° for ER5 and −0.9 ± 4.8° for TR5.
ATD134 and ATD200 laxity scores were highly correlated (r = 0.98; p < 0.01). The distribution of the laxity score is represented for ATD200 in Fig. 3. About 15 % of knees were hyperlax (corrected score >1 corresponding to an anterior displacement >5.4 mm) and 16 % were hypolax (corrected score <−1 corresponding to an anterior displacement <3.9 mm). IR5 and ER5 laxity scores were moderately correlated (r = 0.60; p < 0.01). The distributions of the laxity score for IR5 and for ER5 are presented in Figs. 4 and 5, respectively. About 15 % of the tested knees were hyperlax (scores >1) both for IR5 and for ER5. The proportion of hypolax knees (scores <−1) was 19 % for IR5 and 14 % for ER5.
Laxity scores between anterior and static rotational knee laxity were poorly correlated (r < 0.24), although significant between anterior displacement and IR. Figure 6 indicates the distribution of laxity profiles in our healthy population considering IR5, ER5 and ATD200. Only 32 % of healthy knees with normal anterior laxity also demonstrated a normal rotational laxity in both internal and external rotation (IR5 and ER5). Two per cent of the knees were hyperlax and 2 % hypolax for all three measured parameters. Four per cent of the knees displayed increased (score >1) laxity scores in two (of the three studied) directions, and 5 % displayed 2 decreased (score <−1) laxity scores. About 22 % of the knees showed one increased laxity score and 28 % one decreased score (the two other scores being normal). Five per cent of the knees demonstrated both increased and decreased laxity scores.
Distribution of laxity profiles expressed in percentage (%). Decreased: laxity score <−1, normal: laxity score between −1 and 1, increased: laxity score >1. ATD200: anterior tibial displacement at 200 N, IR5: internal rotation at 5 Nm, ER5: external rotation at 5 Nm. Knee laxity profiles: green—normal for all three directions, light blue—decreased for one direction, dark blue—decreased for at least two directions, orange—increased for one direction, red—increased for at least two directions, grey—mixed profile, increased and decreased scores
Discussion
The main findings of this study were that rotational, but not anterior static laxity was related to individual characteristics such as gender and body mass and that both laxities were poorly correlated. Insofar, our starting hypotheses were only partly confirmed. Furthermore, we observed a wide individual variety of laxity scores through the combination of the measured anterior and rotational laxity. According to our definitions, only 32 % of healthy knees showed a normal laxity profile for all three measured laxity directions (anterior displacement, internal and external rotation). A high proportion of healthy knees (33 and 40 %, respectively) were concerned by either hyper- or hypolaxity (stiffness), 5 % of them being affected by both.
The low correlation between anterior displacement and internal rotation (r < 0.24) is in agreement with the current literature [20]. It suggests that both measurements yield complementary information which may play a role in the occurrence of knee injuries or diseases, like in the context of non-contact ACL injuries: both anterior and rotational knee laxities are influenced by the ACL which plays a role in constraining the knee both in the sagittal [7] and in the transverse plane [18]. Combined measurements of anterior and rotational knee laxity might therefore also be useful in the prevention, diagnosis and follow-up of ACL ruptures and may provide new insight into the role of associated injuries on knee laxity. The existence of specific laxity profiles has been previously suggested [19], but their distribution in a general population has not yet been reported. The proposed laxity score allowed for a precise categorization of knee laxity, independently of individual influencing parameters such as body mass or gender. The normative data presented here may allow improving the comprehension of physiological and pathological laxity. Furthermore, they could represent a basis for further observations trying to identify which type of laxity profile might put a person at increased risk for knee injuries or degenerative diseases. Similar attempts have been made previously to define, for instance, the bony morphotypes of the lower extremities [3] and their relation with OA.
Physiological knee laxity has received little attention in spite of indications that it influences knee diseases/injuries and their outcomes. Excessive laxity has been recognized as a risk factor for non-contact ACL injuries [22] and more importantly for worse reconstruction outcomes [4, 8]. As a consequence, patients being identified with hyperlaxity (i.e. in the contralateral leg) at the diagnosis might require specific surgery and a close follow-up regarding laxity and OA symptoms throughout the years following surgery. This approach has already been applied to assess the influence of hypermobility on ACL reconstruction outcomes: patients with hyperextension displayed better stability with a patellar tendon graft compared to a hamstrings tendon graft [9]. No data are available yet on physiological laxity; insofar, the present results represent an interesting contribution to this field. Excessive knee laxity is also assumed to be a risk factor for knee OA in non-traumatic knees. Anterior laxity is indeed known to be increased in patient knees with a Kellgren/Lawrence score of I compared to healthy controls, and cross-sectional studies showed that anterior and rotational laxity decrease with severity of knee OA [25]. These findings highlight the potential of knee laxity measurements to follow OA progression in a non-invasive manner, providing sufficiently precise evaluations to compare a particular patient to the healthy population. Hypolaxity has not been previously defined, and its potential influence on injuries or degenerative joint disease is unknown. Our findings may therefore stimulate the debate around the need for individualized care of knee injuries and disease. More work is needed to improve the comprehension of the role of individual knee function in the occurrence of degenerative knee diseases, knee injuries (e.g. non-contact ACL injuries) and poor treatment outcomes.
None of the considered individual characteristics was found to influence anterior knee laxity measurements. So far, there is no agreement in the literature regarding the relationship between anterior laxity and gender. Some studies showed greater anterior knee laxity in females (up to 2.5 mm) compared to males [20, 22], whereas others did not (<0.3 mm) [17].Unlike us, some authors also reported a significant effect of BMI, height, age, hip anteversion and navicular drop on anterior laxity [19]. As for rotational knee laxity, several studies recognized an increased rotational laxity in females as compared to males [2, 12, 20]. According to our own experience [12, 21], interpretation of static rotational laxity measurements is very complex and requires further investigation. Some authors recently hypothesized that the increased laxity often observed in females may be explained by sex differences in body composition [12, 19] and lower limb alignment [19]. Its significance has not been completely elucidated yet, but it may be one of the multiple factors playing a role in the increased risk of non-contact ACL injuries or certain types of OA in females.
A critical appraisal of previously reported differences in laxity measurements is difficult, since the precision of the used devices has rarely been reported. A difference that is inferior to the precision of the device might reveal a measurement error rather than a real difference. A strength of this study is the test–retest design and the reporting of MDC values for both anterior and rotational knee laxity measurement devices. Measurement of anterior laxity has been shown to be more reproducible with the GNRB® than the KT-1000 regardless of the examiner’s experience [5, 16]. Previous work evaluated intra-examiner reproducibility precision of the GNRB® at 2–4 mm depending on the installation procedures [24].Here, we found a considerably better inter-examiner precision of 1.2 mm at 200 N, probably related to our rigorous standardization of subject positioning, as previously recommended [24]. Considering the static rotational laxity measurement device (second version), this study reports for the first time its precision.
The present study has some limitations. Anatomical knee integrity was limited to the participants’ self-report of previous knee injuries or surgery. Only anterior and rotational knee laxities were considered, although varus–valgus laxity and genu recurvatum assessment may also be interesting to describe individual knee laxity profiles. The use of other laxity devices, especially for rotational knee laxity measurement, might yield different laxity values due to the technical discrepancies [13]. Measuring knee rotation at the foot has indeed been shown to be less accurate than directly on the overlying skin [1]. The approach presented in this paper can, however, easily be adapted to any laxity measurement device. It allows for a convenient classification of knees as hypo-, normo- and hyperlax for rotation and anterior tibial displacement. Moreover, through the standardization of the score, comparison of an individual person to a general population is now possible irrespective of individual differences in gender or BMI.
Conclusion
To conclude, the large variation of knee laxity profiles, the influence of gender and body mass on rotational knee laxity as well as the low correlation between static anterior and rotational knee laxities illustrate the high degree of complexity of knee function. This suggests that combined measurements of anterior and rotational static knee laxity might provide additional clinical information for the understanding of OA development and the diagnosis of knee soft tissue injuries. These results contribute to the understanding of knee injuries and diseases and are the starting point for prevention strategies and improvement of treatment outcomes.
References
Alam M, Bull AM, Thomas RD, Amis AA (2011) Measurement of rotational laxity of the knee. In vitro comparison of accuracy between the tibia, overlying skin, and foot. Am J Sports Med 39:2575–2581
Almquist PO, Ekdahl C, Isberg PE, Friden T (2013) Knee rotation in healthy individuals related to age and gender. J Orthop Res 31:23–28
Bellemans J, Colyn W, Vandenneucker H, Victor J (2012) The Chitranjan Ranawat award: is neutral mechanical alignment normal for all patients? The concept of constitutional varus. Clin Orthop Relat Res 470:45–53
Branch TP, Siebold R, Freedberg HI, Jacobs CA (2011) Double-bundle ACL reconstruction demonstrated superior clinical stability to single-bundle ACL reconstruction: a matched-pairs analysis of instrumented tests of tibial anterior translation and internal rotation laxity. Knee Surg Sports Traumatol Arthrosc 19:432–440
Collette M, Courville J, Forton M, Gagniere B (2012) Objective evaluation of anterior knee laxity; comparison of the KT-1000 and GNRB(R) arthrometers. Knee Surg Sports Traumatol Arthrosc 20:2233–2238
Cook RD, Weisberg S (1982) Residuals and influence in regression. Chapman and Hall, New York
Fukubayashi T, Torzilli PA, Sherman MF, Warren RF (1982) An in vitro biomechanical evaluation of anterior–posterior motion of the knee. Tibial displacement, rotation, and torque. J Bone Jt Surg Am 64:258–264
Kim SJ, Choi DH, Mei Y, Hwang BY (2011) Does physiologic posterolateral laxity influence clinical outcomes of anterior cruciate ligament reconstruction? J Bone Jt Surg Am 93:2010–2014
Kim SJ, Moon HK, Kim SG, Chun YM, Oh KS (2010) Does severity or specific joint laxity influence clinical outcomes of anterior cruciate ligament reconstruction? Clin Orthop Relat Res 468:1136–1141
Lorbach O, Kieb M, Brogard P, Maas S, Pape D, Seil R (2012) Static rotational and sagittal knee laxity measurements after reconstruction of the anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc 20:844–850
Meredick RB, Vance KJ, Appleby D, Lubowitz JH (2008) Outcome of single-bundle versus double-bundle reconstruction of the anterior cruciate ligament: a meta-analysis. Am J Sports Med 36:1414–1421
Mouton C, Seil R, Agostinis H, Maas S, Theisen D (2012) Influence of individual characteristics on static rotational knee laxity using the Rotameter. Knee Surg Sports Traumatol Arthrosc 20:645–651
Mouton C, Theisen D, Pape D, Nuhrenborger C, Seil R (2012) Static rotational knee laxity in anterior cruciate ligament injuries. Knee Surg Sports Traumatol Arthrosc 20:652–662
Myers RH (1990) Classical and modern regression with applications. PWS-KENT Publishing Company, Boston
Neuman P, Kostogiannis I, Friden T, Roos H, Dahlberg LE, Englund M (2012) Knee laxity after complete anterior cruciate ligament tear: a prospective study over 15 years. Scand J Med Sci Sports 22:156–163
Robert H, Nouveau S, Gageot S, Gagniere B (2009) A new knee arthrometer, the GNRB: experience in ACL complete and partial tears. Orthop Traumatol Surg Res 95:171–176
Sharma L, Lou C, Felson DT, Dunlop DD, Kirwan-Mellis G, Hayes KW et al (1999) Laxity in healthy and osteoarthritic knees. Arthritis Rheum 42:861–870
Shoemaker SC, Markolf KL (1985) Effects of joint load on the stiffness and laxity of ligament-deficient knees. An in vitro study of the anterior cruciate and medial collateral ligaments. J Bone Jt Surg Am 67:136–146
Shultz SJ, Dudley WN, Kong Y (2012) Identifying multiplanar knee laxity profiles and associated physical characteristics. J Athl Train 47:159–169
Shultz SJ, Shimokochi Y, Nguyen AD, Schmitz RJ, Beynnon BD, Perrin DH (2007) Measurement of varus–valgus and internal–external rotational knee laxities in vivo—part II: relationship with anterior–posterior and general joint laxity in males and females. J Orthop Res 25:989–996
Tardy N, Mouton C, Boisrenoult P, Theisen D, Beaufils P, Seil R (2013) Rotational profile alterations after anatomic posterolateral corner reconstructions in multiligament injured knees. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-013-2655-0
Uhorchak JM, Scoville CR, Williams GN, Arciero RA, St Pierre P, Taylor DC (2003) Risk factors associated with noncontact injury of the anterior cruciate ligament: a prospective four-year evaluation of 859 West Point cadets. Am J Sports Med 31:831–842
van Eck CF, Loopik M, van den Bekerom MP, Fu FH, Kerkhoffs GM (2013) Methods to diagnose acute anterior cruciate ligament rupture: a meta-analysis of instrumented knee laxity tests. Knee Surg Sports Traumatol Arthrosc 21:1989–1997
Vauhnik R, Perme MP, Barcellona MG, Rugelj D, Morrissey MC, Sevsek F (2013) Robotic knee laxity testing: reliability and normative data. Knee 20:250–255
Wada M, Imura S, Baba H, Shimada S (1996) Knee laxity in patients with osteoarthritis and rheumatoid arthritis. Br J Rheumatol 35:560–563
Weir JP (2005) Quantifying test–retest reliability using the intraclass correlation coefficient and the SEM. J Strength Cond Res 19:231–240
Acknowledgments
The present project has been supported by the National Research Fund, Luxembourg (1084312) and by the Oeuvre Nationale de Secours Grande-Duchesse Charlotte.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made.
The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
To view a copy of this licence, visit https://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mouton, C., Seil, R., Meyer, T. et al. Combined anterior and rotational laxity measurements allow characterizing personal knee laxity profiles in healthy individuals. Knee Surg Sports Traumatol Arthrosc 23, 3571–3577 (2015). https://doi.org/10.1007/s00167-014-3244-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-014-3244-6