Abstract
The aim of the study was to evaluate the time zero mechanical properties of single- versus double-row configuration for rotator cuff repair in an animal model with consideration of the stitch technique and suture material. Thirty-two fresh-frozen sheep shoulders were randomly assigned to four repair groups: suture anchor single-row repair coupled with (1) braided, nonabsorbable polyester suture sized USP No. 2 (SRAE) or (2) braided polyblend polyethylene suture sized No. 2 (SRAH). The double-row repair was coupled with (3) USP No. 2 (DRAE) or (4) braided polyblend polyethylene suture No. 2 (DRAH). Arthroscopic Mason–Allen stitches were used (single-row) and combined with medial horizontal mattress stitches (double-row). Shoulders were cyclically loaded from 10 to 180 N. Displacement to gap formation of 5- and 10-mm at the repair site, cycles to failure, and the mode of failure were determined. The ultimate tensile strength was verified in specimens that resisted to 3,000 cycles. DRAE and DRAH had a lower frequency of 5- (P = 0.135) and 10-mm gap formation (P = 0.135). All DRAE and DRAH resisted 3,000 cycles while only three SRAE and one SRAH resisted 3,000 cycles (P < 0.001). The ultimate tensile strength in double-row specimens was significantly higher than in others (P < 0.001). There was no significant variation in using different suture material (P > 0.05). Double-row suture anchor repair with arthroscopic Mason–Allen/medial mattress stitches provides initial strength superior to single-row repair with arthroscopic Mason–Allen stitches under isometric cyclic loading as well as under ultimate loading conditions. Our results support the concept of double-row fixation with arthroscopic Mason–Allen/medial mattress stitches in rotator cuff tears with improvement of initial fixation strength and ultimate tensile load. Use of new polyblend polyethylene suture material seems not to increase the initial biomechanical aspects of the repair construct.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Despite encouraging clinical outcomes, recurrent tears remain one of the most frequent complications especially seen in arthroscopic rotator cuff repair [2, 3, 13]. Although, failures are often attributed to the severity of the tear or poor quality of the tendon, another theory of failure is the inferior mechanical strength of the repair technique, e.g. use of a single-row of suture anchors [16]. Moreover, these repairs may not adequately restore the native footprint contact [16, 33]. Therefore, the goal is to re-establish the anatomical configuration of the tendon-bone construct, accompanied by the restoration of its mechanical performance. With use of the double-row technique the native footprint area could be recreated more accurately and therefore may improve the ability of the tendon to heal to bone [1, 11, 19]. The configuration of the suture in the soft tissue is an important part of the success or failure of this procedure as well [8]. The modified Mason–Allen stitch has superior strength compared to simple and horizontal mattress stitches applied in rotator cuff repair [16]. However, arthroscopic techniques for rotator cuff repair usually use the easier-to-perform simple or horizontal stitches fixed with suture anchors, because of the technical difficulty of placing modified Mason–Allen stitches. Thus, arthroscopic achievement of a firm tendon-bone construct is not met with ease, and it remains a need for a solid tissue-holding technique [20].
Scheibel and Habermeyer [29] used a so-called arthroscopic Mason–Allen technique for suture anchor repair. The technique consists of a combination of a horizontal mattress and a single stitch through the same anchor. In a recent investigation, we demonstrated that the combination of bioabsorbable suture anchors and arthroscopic Mason–Allen stitches in a single-row configuration provides strength superior to that of the traditional transosseous suture and modified Mason–Allen stitches under isometric cyclic loading [17].
The objective of this biomechanical assessment was to determine the initial biomechanical properties of a double-row suture anchor technique in order to consider improvements in rotator cuff repair. In addition, we assessed the biomechanical differences in cyclic loading of a new high-performance polyblend suture material and a braided polyester suture. We hypothesized that the combination of arthroscopic Mason–Allen and medial mattress stitches in a double-row configuration using a high-performance polyblend polyethylene suture material would have a superior response in cyclic loading compared to a repair using the single-row technique with arthroscopic Mason–Allen stitches. Moreover, we performed a detailed review of the medical literature using MEDLINE to give an overview of the results of biomechanical studies regarding the double-row technique for the repair of rotator cuff tears.
Materials and methods
Thirty-two fresh sheep shoulders (specimen age, 2 years) were harvested fresh, wrapped in saline-soaked gauze, and stored frozen at −20°C [17, 34].
The shoulders were dissected from all of the soft tissues except for the infraspinatus muscle and tendon. No pre-existing rotator cuff abnormalities were noted in all of the specimens. The infraspinatus tendon was sharply detached from its insertion site to mimic a full-thickness tear, as established in previous investigations at our institution [17, 18]. Right and left shoulders were randomly assigned among four treatment groups that were based on the use of absorbable suture anchors (Duet Suture Anchor®, ConMed Linvatec, Largo, FL, USA) coupled either with braided nonabsorbable polyester suture sized USP No. 2 (Ethibond®; Ethicon, Sommerville, NJ, USA) or with new high-performance polyblend polyethylene suture sized No. 2 (HiFi®; ConMed Linvatec, Largo, FL, USA). The groups were as follows:
-
•
single-row repair using one line of two suture anchors coupled with double-loaded Ethibond® suture (SRAE) (stitch: arthroscopic Mason–Allen).
-
•
single-row repair using one line of two suture anchors coupled with double-loaded HiFi® suture (SRAH) (stitch: arthroscopic Mason–Allen).
-
•
double-row repair using two lines with a total of four suture anchors coupled with Ethibond® suture (DRAE) [stitch: arthroscopic Mason–Allen (lateral/double-loaded)-horizontal mattress stitch (medial/single-loaded)].
-
•
double-row repair using two lines with a total of four suture anchors coupled with HiFi® suture (DRAH) [stitch: arthroscopic Mason–Allen (lateral/double-loaded)-horizontal mattress stitch (medial/single-loaded)].
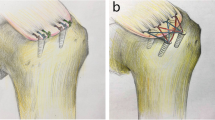
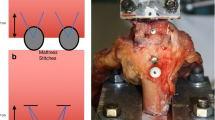
Each anchor system was placed according to the manufacturer guidelines over a guidewire after using a cannulated tap to prepare the bone; the anchor was then inserted into the bone at a 45° angle to the diaphysis of the humerus with the eyelet flush with the bone [4, 9, 31]. Then, the tendon was reattached to its insertion site with the anchors placed 5 mm apart and 5 mm from the distal tendon margin for single-row, and 5 mm from the proximal tendon margin for double-row repair (medial row). Arthroscopic Mason–Allen stitches were used for the lateral row of anchors; horizontal mattress stitches were used for the medial row (Figs. 1, 2). Bone troughs were not used and no pretension was applied to the tendon during repair [17, 18]. All steps of insertion of the anchor systems, as well as suture passing, were performed with the use of instruments for arthroscopic repair (Spectrum tissue repair system, ConMed Linvatec, Largo, FL, USA) to simulate an arthroscopic setting. The orientation of the cannulae corresponded to the anterior, lateral, and posterior portals for shoulder arthroscopy [31]. The procedure was performed in an air environment, with the use of an arthroscopic knot-tying technique. Each stitch was first tied with the use of a sliding double half-hitch knot, secured by a series of four reversing half-hitches on alternative posts.
The dissections, preparations, and repairs were performed by one single experienced shoulder surgeon (MHB) after thawing the shoulders for 24 h at room temperature. Standard procedures for rotator cuff repairs were used to minimize variability in the technique. Specimens were kept moist with 0.9% saline during dissection, preparation, and biomechanical testing.
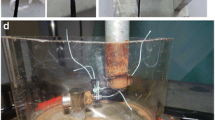
Experimental testing
The investigations were performed at room temperature using a material testing machine (Zwick 1445, Zwick-Roell, Ulm, Germany), which recorded the data with the dedicated software (Textexpert 8.1, Zwick-Roell, Ulm, Germany), and evaluated the data with a load-displacement curve. The proximal end of the infraspinatus tendon was set in a tendon clamp, leaving approximately 6 cm between the clamp and the site of repair (Fig. 3). To prevent it from slipping out of the clamp during the experiment, “cryo-jaws” for soft tissue fixation were used [28]. The humerus was fixed in a custom rig designed to evenly distribute loads across the tendon.
Cyclic loading testing
The shoulders were loaded to a physiologic direction of the rotator cuff tendon perpendicular to the longitudinal axis of the humerus as previously described [10, 26]. To simulate postoperative conditions, a cyclic loading was performed, similar to previous studies [6, 27]. These parameters have been reported as the physiologic loads and speeds that occur in normal daily activity and were therefore considered the best manner to simulate the postoperative condition [5, 17]. After pretension to 10 N for 1 min, each construct was cyclically loaded to 3,000 cycles from 10 to 180 N with a 5-s cycle [5, 6, 17]. The tests were stopped when complete failure (e.g. repair site gap 10 mm, defect of the tendon-bone construct) or a total of 3,000 cycles was attained. The loading force was applied with the humerus maintained at a constant angle relative to the tendon, resulting in simulated isometric muscle contraction [28]. Gap formation at each repair site was measured using an extensometer. Based on previous studies at our institution, the number of cycles creating a 5- and 10-mm gap was recorded, along with the mechanism of failure [17, 28].
Load-to-failure testing
Following the cyclic loading procedure, specimens that resisted 3,000 cycles were loaded to failure at a constant displacement rate of 1 mm/s. A pretension of 10 N was applied and the clamp and custom rig were checked for tightness before beginning the load-to-failure testing. The time between protocols was the same for all specimens. The load (N) and the displacement (mm) were digitally recorded by a deformation curve, and the mode of failure was documented.
Statistical analysis
The tendon repairs were tested on separate specimens. Statistical analysis was performed using SPSS software (Rel. 13.0, SPSS, Chicago, IL, USA). Results are reported as mean values ± standard deviation. Frequencies were compared by using the chi-square test. The Kolmogorov–Smirnov test and analysis of variance (ANOVA) were used, in addition to the Mann–Whitney U test; the level of significance set at P < 0.05.
Results
The number of cycles to 5-mm gap formation was significantly higher in the DRAE (2,942.6 ± 50.5 cycles) and the DRAH (2,934 cycles) than that for the SRAE (1,977 ± 944.3 cycles) and the SRAH (1,475.2 ± 913.3 cycles) (P < 0.05). Single-row specimen (SRAE, SRAH) had a lower number of cycles to a 5-mm gap (P = 0.135). In both single-row specimens (SRAE, SRAH) five of eight reached a 5-mm gap. Double-row specimens (DRAE, DRAH) had a lower frequency of 5-mm gap formation (three of eight in DRAE, and one of eight in DRAH) (P = 0.135).
For 10-mm gap formation, the DRAH withstood a mean of 2,934 cycles while the SRAE lasted 2,437 ± 620.8 cycles and the SRAH 2,227.5 ± 154.8 cycles, respectively. The frequency of 10-mm gap formation in both single-row specimens (SRAE, SRAH) was two of eight, whereas double-row specimen (DRAE, DRAH) had a lower frequency of 10-mm gap formation (none in DRAE group, and one of eight in the DRAH group) (P = 0.456). No significant difference between the groups was evaluated regarding to the number of cycles for 10-mm gap formation (P = 0.551).
All double-row specimens (DRAE, DRAH) resisted against 3,000 cycles. Only three of the SRAE and one of the SRAH specimen resisted 3,000 cycles (P < 0.001). The mean number of cycles of the specimens with a resistance of less than 3,000 cycles was 926. There was no significant difference when comparing the different repair groups (P = 0.274). Specimens which resisted more than 3,000 cycles had an ultimate tensile strength of 334.3 ± 81.1 N. The tensile strength in double-row specimens (DRAE, DRAH) was significantly higher than in others (P < 0.001).
There was no anchor-related failure during cycling loading and load to failure testing. In one case the failure was related to the breakage of the suture (SRAE). The other failure was caused by the suture pulling through the tendon in four of the SRAE and seven of the SRAH repairs. During load to failure testing all of the failure was caused by suture breakage (DRAE as well as DRAH). There was no significant difference in using the various suture materials (P > 0.05).
Discussion
The objective of this study was to compare the biomechanical properties of single- and double-row fixation for rotator cuff tears with consideration of the stitch technique and suture material. We confirmed our hypothesis with the principle result that double-row repair provides significantly better resistance to cyclic elongation and load-to-failure than do single-row repairs (P < 0.001). However, we can not confirm significant differences between the use of nonabsorbable polyester suture (Ethibond®) compared to polyblend high-performance suture (HiFi®) (P > 0.05).
Numerous studies have documented the mechanical characteristics of several refixation techniques in the repair of rotator cuff tears [6, 9, 10, 14, 17, 31]. Most evaluations have dealt with investigations on traditional transosseous or anchor single-row fixations [6, 9, 10, 14, 17, 31]. In our review of the current literature, few articles have been published regarding the biomechanical properties of double-row repair using different stitch techniques (Tables 1, 2) [16, 20–25, 30].
Mazzocca et al. [22] randomly assigned 20 fresh-frozen cadaveric shoulders to four arthroscopic repair techniques: (1) a single-row of anchors, (2) a diamond anchor, (3) a mattress double-anchor, and (4) a modified mattress double-anchor. The shoulders were positioned to enable an arthroscopic-like repair with the use of shuttle devices as compared to our study. They defined a gap formation of greater than 4 mm and a load-to-failure of less than 250 N for biomechanical failure. In contrast to our results, there was no significant difference among the treatment groups in load-to-failure and displacement. All repairs demonstrated a load-to-failure greater than 250 N (Table 2).
This is comparable to the results of a study of [21]. Double-row repair in a bovine model did not show a biomechanical advantage compared to single-row repair with no significant differences for loads at 3-, 5-, and 10-mm elongation. Unlike these results Milano et al. [24] reported a significantly higher resistance of double-row repair to cyclic loading than single-row repair. Their investigation was done with an animal model (porcine shoulders) as well. On the contrary to our study they used both, a tension-free and a tension repair for each, the single-row and the double-row repair. Both of the double-row repair groups resisted a maximum of 1,000 cycles with the lowest total elongation seen in the tension-free repair group (6.9 ± 1.5 mm). They concluded that double-row anchor repair could therefore primarily be considered for large and unstable rotator cuff tears.
Kim et al. [16] performed an investigation in nine matched pairs of fresh-frozen cadaver shoulders and reattached the supraspinatus tendon with a single- and double-row repair, each sutured with No. 2 FiberWire®. No information was given as to whether they used arthroscopic instruments to place the sutures (Table 1). Each specimen underwent cyclic loading from 10 to 180 N for 200 cycles, followed by tensile load-to-failure. As demonstrated in our investigation, they showed a significantly smaller gap formation for the double-row repair compared to the single-row technique. The ultimate failure load increased by 48%, as compared to the single-row repair (Table 2), which is comparable to our result.
Ma et al. [20] used (1) a two-simple, (2) a massive cuff, (3) an arthroscopic Mason–Allen, and (4) a double-row fixation. A No. 2 FiberWire® was used for fixation (Table 1). Splitted tendons were cyclically loaded between 5 and 100 N with a significantly higher ultimate tensile load for the double-row repair as shown in our recent study (Table 2).
Meier and Meier [23] compared the initial mechanical strength of (1) the transosseous suture technique, (2) a single-row suture anchor fixation, and (3) a double-row suture fixation. There was no information given regarding the stitch configuration (Table 1). After a preload to 5 N, cyclic loading of each specimen was performed to 5,000 cycles. Group 3 had no failures until the samples were stopped when 5,000 cycles had been completed (Table 2). In our assessment, used double-row configurations resisted the defined maximum of 3,000 cycles as well, whereas only four of the single-row configurations resisted this point.
Smith et al. [30] used the two-simple stitch for single-row repair. For double-row repair, a combination of one mattress stitch medial (anchor single-loaded) and two simple stitches lateral (double-loaded) were used (Table 1). They concluded that the double-row technique had a superior resistance to gap formation under static loading as compared to single-row repair (Table 2).
Park et al. [25] compared the initial mechanical strength of a (1) transosseous suture technique and (2) a double-row suture fixation. After a preload to 10 N, cyclic loading of each specimen was performed to 30 cycles. No statistically significant differences between the two repair groups were mentioned (Table 2).
Although our investigation orientated itself to former studies for comparison, it presents some weaknesses. Previous experimental assessments established the sheep shoulder as a valid model for the study of human rotator cuff repair techniques [14, 17, 20]. But one has to consider, that the sheep infraspinatus tendon is different from the degenerated and thinner supraspinatus tendon seen in human shoulders with chronic rotator cuff tears [14]. In the recent study, use of the single-row repair often results in cutting the suture through the tendon, whereas in using the double-row repair, failure is due to suture breakage resulting in higher failure force. We suspect that this phenomenon is due to a steady pressure distribution of the tendon-bone construct in using the double-row repair. Therefore, we are in agreement with Cummis and Murrell [8] that considered that a point is reached at which the weakest link of the repair became the suture material itself. This may be solved by improved material properties of the suture. Nevertheless, in our mind it has to be noted that the more rigid characteristics of the new braided polyblend polyethylene suture material [35] can more easily cut in a parallel direction through the defective tendon as compared to the healthy rotator cuff specimens used in our study. We made this experience in using the single-row repair, in which the suture pulls through the tendon in seven of the SRAH repairs. This aspect is particularly important, because most of the torn human tendons are degenerated, and the tendons that fail the repair using a single-row technique are in the major part grade III degenerate tendons according to the classification of [15].
We used instruments for arthroscopic repair to simulate the arthroscopic environment as best as possible. Nevertheless, stitches were placed in an air environment. The arthroscopic sequences, such as sliding knots as well as alternating half-stitches were used. This could have added enhanced strength and reproducibility to the knots.
Despite excellent results of the double-row technique regarding its initial mechanical strength, it has to be critically discussed for clinical application. It is a more complex method and requires potentially more surgical time compared to treatment with a single-row of anchors. It requires careful suture management and a safe command level, especially with arthroscopic repair and, in addition, produces more costs in suture anchor material. Furthermore, Kim et al. [16] observed anchor failure by greater tuberosity facture in two of their tested specimen. They suspected potential stress risers by placing four anchors to restore the footprint area. In the recent study, we did not observe this complication, but one have to keep this problem in mind, mainly in osteoporotic bone when using the double-row repair. Moreover, the mechanical strength and suture anchor placement of a double-row repair may produce more tension, especially on the medial part of the tendon. This could lead to impaired tissue healing, concerning particularly the vascular conditions of the tendon.
Additionally, the clinical superiority of the double-row technique compared to other techniques could not be proved so far. To our knowledge there are only few studies investigating the clinical outcome of single- versus double-row repair. Sugaya et al. [32] compared both methods retrospectively. The integrity of the repaired cuff was detected by MRI with a significantly better structural outcome in the double-row repair. But no statistical differences were found regarding range of motion, patients’ satisfaction, and pain relief. Franceschi et al. [12] found neither statistical difference in a clinical nor in an MR arthrography follow-up after a mean of 2 years comparing both techniques. These results are in concordance to the study of [7] that used computed tomographic arthrography for assessment. Although in the study of [8] different methods of repair were used, a comparison between single- and double-row is difficult: single-row was only used for small, and double-row was used for the repair of large tears.
In conclusion, the fundamental results of our time-zero evaluation support the hypothesis that cyclic loading and initial ultimate tensile strength of a double-row configuration is superior to the single-row repair technique and provides superior resistance to gap formation. No significant differences (P > 0.05) in using different suture materials could be stated. Considering the outcome of the recent clinical and biomechanical trials in our literature review, there is further need to improve our knowledge in restoring the rotator cuff footprint and to achieve lower failure rates. We have to justify the publicity regarding the double-row technique to apply it clinically, because it will take longer surgical time and will be more expensive than other repair techniques. The superior initial mechanical strength is promising but the data regarding cell biological characteristics has to be expanded. Therefore, we may wait the results of future experimental investigations to determine the in vivo conditions and the extent to which the presented fundamental outcome of our ex vivo study may contribute to improve the healing rates in rotator cuff repair.
References
Apreleva M, Özbaydar M, Fitzgibbons PG, Warner JJP (2002) Rotator cuff tears: the effect of the reconstruction method on three-dimensional repair site area. Arthroscopy 18:519–526
Bishop J, Klepps S, Lo IK, Bird J, Gladstone JN, Flatow EL (2006) Cuff integrity after arthroscopic versus open rotator cuff repair: a prospective study. J Shoulder Elbow Surg 15:290–299
Boileau P, Brassart N, Watkinson DJ, Carles M, Hatzidakis AM, Krishnan SG (2005) Arthroscopic repair of full-thickness tears of the supraspinatus: does the tendon really heal? J Bone Joint Surg Am 87-A:1229–1240
Burkhart SS (1995) The deadman theory of suture anchors: observations along a south Texas fence line. Arthroscopy 11:119–123
Burkhart SS, Diaz Pagan JL, Wirth MA, Athanasiou KA (1997) Cyclic loading of anchor-based rotator cuff repairs: confirmation of the tension overload phenomenon and comparison of suture anchor fixation with transosseous fixation. Arthroscopy 13:720–724
Burkhart SS, Johnson TC, Wirth MA, Athanasiou KA (1997) Cyclic loading of transosseous rotator cuff repairs: tension overload as a possible cause of failure. Arthroscopy 13:172–176
Charousset C, Grimberg J, Duranthon LD, Bellaiche L, Petrover D (2007) Can a double-row anchorage technique improve tendon healing in arthroscopic rotator cuff repair? A prospective, nonrandomized, comparative study of double-row and single-row anchorage techniques with computed tomography arthrography tendon healing assessment. Am J Sports Med 35:1247–1253
Cummis CA, Murrell GA (2003) Mode of failure for rotator cuff repair with suture anchors identified at revision surgery. J Shoulder Elbow Surg 12:128–133
DeCarli A, Vadala A, Monaco E, Labianca L, Zanzotto E, Ferretti A (2005) Effect of cyclic loading on new polyblend suture coupled with different anchors. Am J Sports Med 33:214–219
Demirhan M, Atalar AC, Kilicoglu O (2003) Primary fixation strength of rotator cuff repair techniques: a comparative study. Arthroscopy 19:572–576
Fealy S, Kingham TP, Altcheck DW (2002) Mini-open rotator cuff repair using a two-row fixation technique: outcomes analysis in patients with small, moderate and large rotator cuff tears. Arthroscopy 18:665–670
Franceschi F, Ruzzini L, Longo UG, Martina FM, Zobel BB (2007) Equivalent clinical results of arthroscopic single-row and double-row suture anchor repair for rotator cuff tears. Am J Sports Med 35:1254–1260
Galatz LM, Ball CM, Teefey SA, Middleton WD, Yamaguchi K (2004) The outcome and repair integrity of completely arthroscopically repaired large and massive rotator cuff tears. J Bone Joint Surg Am 86-A:219–224
Gerber C, Schneeberger AG, Beck M, Schlegel U (1994) Mechanical strength of repairs of the rotator cuff. J Bone Joint Surg Br 76-B:371–380
Goutallier D, Postel JM, Bernageau J, Lavau L, Voisin MC (1994) Fatty muscle degeneration in cuff ruptures. Pre- and post-operative evaluation by CT scan. Clin Orthop Relat Res 304:78–83
Kim DH, ElAttrache NS, Tibone JE, Jun BJ, DeLaMora SN, Kvitne RS, Lee TQ (2005) Biomechanical comparison of a single-row versus double-row suture anchor technique for rotator cuff repair. Am J Sport Med 34:407–414
Klinger HM, Steckel H, Spahn G, Buchhorn GH, Baums MH (2007) Biomechanical comparison of double-loaded suture anchors using arthroscopic Mason-Allen stitches versus traditional transosseous suture technique and modified Mason-Allen stitches for rotator cuff repair. Clin Biomech 22:106–111
Klinger H-M, Kahl E, Buchhorn GH, Heidrich G, Steckel H, Baums MH (2008) Biomechanical evaluation of rotator cuff repairs in a sheep model: Suture anchors using arthroscopic Mason-Allen stitches compared with transosseous sutures using traditional modified Mason-Allen stitches. Clin Biomech 23:291–298
Lo IK, Burkart SS (2003) Double-row arthroscopic rotator cuff repair: re-establishing the footprint of the rotator cuff. Arthroscopy 19:1035–1042
Ma CM, Comerford L, Wilson J, Puttlitz CM (2006) Biomechanical evaluation of arthroscopic rotator cuff repairs: double-row compared with single-row fixation. J Bone Joint Surg Am 88-A:403–410
Mahar A, Tamborlane J, Oka R, Esch J, Pedowitz RA (2007) Single-row suture anchor repair of the rotator cuff is biomechanically equivalent to double-row repair in a bovine model. Arthroscopy 23:1265–1270
Mazzocca AD, Millet PJ, Guanche CA, Santangelo SA, Arciero RA (2005) Arthroscopic single-row versus double-row suture anchor rotator cuff repair. Am J Sports Med 33:1861–1868
Meier SW, Meier JD (2006) The effect of double-row fixation on initial repair strength in rotator cuff repair: a biomechanical study. Arthroscopy 22:1168–1173
Milano G, Grasso A, Zarelli D, Deriu L, Cillo M, Fabbriciani C (2008) Comparison between single-row and double-row rotator cuff repair: a biomechnical study. Knee Surg Sports Traumatol Arthrosc 16:75–80. doi:10.1007/s00167-007-0382-0
Park MC, Tibone JE, ElAttrache NS, Ahmad CS, Jun BJ, Lee TQ (2007) Part II: biomechanical assessment for a footprint-restoring transosseous-eqivalent rotator cuff repair technique compared with a double-row repair technique. J Shoulder Elbow Surg 16:469–476
Petit CJ, Boswell R, Mahar A, Tasto J, Pedowitz RA (2003) Biomechanical evaluation of a new technique for rotator cuff repair. Am J Sports Med 31:849–853
Reed SC, Glossop N, Ogilvie-Harris DJ (1996) Full-thickness rotator cuff tears. A biomechanical comparison of suture versus bone anchor techniques. Am J Sports Med 24:46–48
Rickert M, Georgousis H, Witzel U (1998) Tensile strength of the tendon of the supraspinatus muscle in the human. A biomechanical study [German]. Unfallchirurg 101:265–270
Scheibel MT, Habermeyer P (2003) A modified Mason-Allen technique for rotator cuff repair using suture anchors. Arthroscopy 19:330–333
Smith CD, Alexander S, Hill AM, Huijsmans PE, Bull AMJ, Amis AA, Beer JF, Wallace AL (2006) A biomechanical comparison of single and double-row fixation in arthroscopic rotator cuff repair. J Bone Joint Surg Am 88-A:2425–2431
Schneeberger AG, von Roll A, Kalberer F, Jacob HA, Gerber C (2002) Mechanical strength of arthroscopic rotator cuff repair techniques: an in vitro study. J Bone Joint Surg Am 84-A:2152–2160
Sugaya H, Maeda K, Matsuki K, Moriishi J (2007) Repair integrity and functional outcome after arthroscopic double-row rotator cuff repair. J Bone Joint Surg Am 89-A:953–960
Tuoheti Y, Itoi E, Yamamoto N, Seki N, Abe H, Minagawa H, Okada K, Shimada Y (2005) Contact area, contact pressure, and pressure patterns of the tendon-bone interface after rotator cuff repair. Am J Sports Med 33:1869–1874
Woo SL, Orlando CA, Camp JF, Akeson WH (1986) Effects of postmortem storage by freezing on ligament tensile behavior. J Biomech 19:399–404
Wüst DM, Meyer DC, Favre P, Gerber C (2006) Mechanical and handling properties of braided polyblend polyethylene sutures in comparison to braided polyester and monofilament polydioxanone sutures. Arthroscopy 22:1146–1153
Acknowledgments
The authors appreciate Mrs. G. Wolf-Bergk for creating the anatomical line drawings in this report. The work was founded by the Research programme, University of Göttingen Medical Centre (UMG), Georg-August-University, Germany.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License ( https://creativecommons.org/licenses/by-nc/2.0 ), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Baums, M.H., Buchhorn, G.H., Spahn, G. et al. Biomechanical characteristics of single-row repair in comparison to double-row repair with consideration of the suture configuration and suture material. Knee Surg Sports Traumatol Arthr 16, 1052–1060 (2008). https://doi.org/10.1007/s00167-008-0590-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-008-0590-2