Abstract
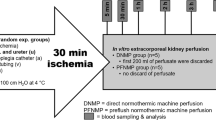
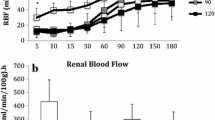
The aim of this study was to determine the potential benefit of aerobic machine preservation (MP) with non-colloidal histidine–tryptophan–ketoglutarate (HTK) solution compared with MP with Belzer machine perfusion solution (MPS) and standard cold storage, after marginal kidneys had been obtained from non-heart-beating donors. Cardiac arrest was electrically induced in anaesthetized German landrace pigs (20–25 kg bw). Their kidneys were harvested 40 min thereafter, flushed with HTK by gravity of 100 cm H2O via the renal artery and then stored in HTK for 18 h at 4°C. Other organs were subjected to oxygenated (pO2>500 mmHg) hypothermic pulsatile low-flow machine perfusion with HTK or MP with Belzer MPS at Pmax=40 mmHg, yielding transrenal flow values of 0.2–0.3 ml/min per g with HTK and approximately twice that amount with Belzer MPS. A well-preserved vascular endothelium and intact tubular epithelium were documented by electron microscopy at the end of perfusion preservation in both solutions as well as after cold storage. Concentrations of ATP (in micromoles per gramme) in tissue homogenates at the end of perfusion preservation with HTK were 1.18±0.12 vs 0.16±0.02 (P<0.05) after simple cold storage and 2.43±0.23 after perfusion with Belzer MPS, thus documenting a relevant effect of low-flow perfusion on tissue oxygenation. Viability of the grafts was followed for 1 week after heterotopic transplantation and bilateral nephrectomy in the recipient pigs. Machine perfusion with HTK significantly improved cortical microcirculation upon early reperfusion in vivo, as well as maximal serum levels of urea and creatinine, compared to recipients receiving cold-stored grafts. No differences could be found between MP with HTK or Belzer MPS. In conclusion, provision of oxygen during storage is possible by low-flow perfusion with HTK as with Belzer MPS and apparently improves graft viability after transplantation.


Similar content being viewed by others
References
Cho YW, Terasaki PI, Cecka JM, Gjertson DW. Transplantation of kidneys from donors whose hearts have stopped beating. N Engl J Med 1998; 338:221.
Kootstra G, Kievit JK, Heineman E. The non heart-beating donor. Br Med Bull 1997; 53:844.
Ethics Committee ACoCCMSoCCM. Recommendations for nonheartbeating organ donation. A position paper by the Ethics Committee, American College of Critical Care Medicine, Society of Critical Care Medicine. Crit Care Med 2001; 29:1826.
Casavilla A, Ramirez C, Shapiro R, Nghiem D, Miracle K, Bronsther O, et al. Experience with liver and kidney allografts from non-heart- beating donors. Transplantation 1995; 59:197.
Wijnen RMH, Booster MH, Stubenitsky BM, deBoer J, Heinemann E, Kootstra G. Outcome of transplantation of non-heart-beating donor kidneys. Lancet 1995; 345:1067.
Valdes F, Pita S, Alonso A, Rivera CF, Cao M, Fontan MP, et al. Comparative study of the use of systolic and asystolic kidney donors between 1981–1995 in La Coruna, Spain. Transplant Proc 1997; 29:3565.
Daemen JH, de WR, Bronkhorst MW, Marcar ML, Yin M, Heineman E, et al. Short-term outcome of kidney transplants from non-heart-beating donors after preservation by machine perfusion. Transplant Int 1996; 9 [Suppl 1]:S76.
Balupuri S, Buckley P, Mohamad M, Chidambaram V, Gerstenkorn C, Sen B, et al. Early results of a non-heartbeating donor (NHBD) programme with machine perfusion. Transplant Int 2000; 13 [Suppl 1]:S255.
Light JA, Barhyte DY, Gage FA, Sasaki TM, Aquino AO. Long-term graft survival after transplantation with kidneys from uncontrolled nonheartbeating donors. Transplantation 1999; 68:1910.
Polyak MM, Arrington BO, Stubenbord WT, Boykin J, Brown T, Jean-Jacques MA, et al. The influence of pulsatile preservation on renal transplantation in the 1990s. Transplantation 2000; 69:249.
Toledo-Pereyra LH, Palma-Vargas JP, Paez-Rollys AJ. Kidney preservation. In: Toledo-Pereyra LH, Austin TX (eds) Organ procurement and preservation for transplantation. Landes Bioscience, 1997: p111.
Yamauchi J, Richter S, Vollmar B, Menger MD, Minor T. Microcirculatory perfusion pattern during harvest of livers from non-heart beating donors: Beneficial effect of warm preflush with streptokinase. Transplant Proc 2000; 32:21.
Yamauchi J, Schramm R, Richter S, Vollmar B, Menger MD, Minor T. Improvement of microvascular graft equilibration and preservation in non-heart-beating donors by warm preflush with streptokinase. Transplantation 2003; 75:449.
Morariu AM, Vd PA, Oeveren V, ‘T Hart NA, Leuvenink HG, Graaff R, et al. Hyperaggregating effect of hydroxyethyl starch components and University of Wisconsin solution on human red blood cells: a risk of impaired graft perfusion in organ procurement? Transplantation 2003; 76:37.
Yu W, Coddington D, Bitter-Suermann H. Use of crystalloids prior to storage in University of Wisconsin solution is deleterious in liver preservation. Transplant Proc 1991; 23:664.
Minor T, Olschewski P, Tolba R, Akbar S, Kocálková M, Dombrowski F. Liver preservation with HTK: salutary effect of hypothermic aerobiosis by either gaseous oxygen or machine perfusion. Clin Transplant 2002; 16:206.
Lauschke H, Olschewski P, Tolba R, Schulz S, Minor T. Oxygenated machine perfusion mitigates surface antigen expression and improves preservation of predamaged donor livers. Cryobiology 2003; 46:53.
Cerra FB, Raza S, Andres GA, Siegel JH. The endothelial damage of pulsatile renal preservation and its relationship to perfusion pressure and colloid osmotic pressure. Surgery 1977; 81:534.
Minor T, Isselhard W, Yamaguchi T. Involvement of platelet activating factor in microcirculatory disturbances after global hepatic ischemia. J Surg Res 1995; 58:536.
Richardson KC, Jarett L, Finke EH. Embedding in epoxy resins for ultrathin sectioning in electron microscopy. Stain Technol 1960; 35:313.
Minor T, Hachenberg A, Tolba R, Pauleit D, Akbar S. Fibrinolytic preflush upon liver retrieval from non-heart beating donors to enhance postpreservation viability and energetic recovery upon reperfusion. Transplantation 2001; 71:1792.
Dutkowski P, Schonfeld S, Odermatt B, Heinrich T, Junginger T. Rat liver preservation by hypothermic oscillating liver perfusion compared to simple cold storage. Cryobiology 1998; 36:61.
Lokkegaard H, Gyrd-Hansen N, Hansen RI, Hasselager E, Nerstrom B, Rasmussen F. 48-hour preservation of pig kidneys using continuous hypothermic plasma perfusion. Effect and complications. Acta Med Scand 1972; 192:243.
Minor T, Akbar S, Tolba R, Dombrowski F. Cold preservation of fatty liver grafts: prevention of functional and ultrastructural impairments by venous oxygen persufflation. J Hepatol 2000; 32:105.
Pegg DE. Organ preservation. Surg Clin North Am 1986; 66:617.
Minor T, Saad S, Nagelschmidt M, Kötting M, Fu Z, Paul A, et al. Successful transplantation of porcine livers after warm ischemic insult in situ and cold preservation including postconditioning with gaseous oxygen. Transplantation 1998; 65:1262.
Iwamoto H, Matsuno N, Narumi Y, Uchiyama M, Kozaki K, Degawa H, et al. Beneficial effect of machine perfusion preservation on liver transplantation from non-heart-beating donors. Transplant Proc 2000; 32:1645.
Acknowledgements
Thomas Minor was supported by the Deutsche Forschungsgemeinschaft (DFG; grant number Mi 470/8-1). Frank Dombrowski was supported by the DFG (grant number Do 622/1-5). The authors gratefully acknowledge the valuable technical assistance of Mariana Kocalkova in preparing the electron micrographs and Susanne Schulz in performing the biochemical analyses.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Minor, T., Sitzia, M. & Dombrowski, F. Kidney transplantation from non-heart-beating donors after oxygenated low-flow machine perfusion preservation with histidine–tryptophan–ketoglutarate solution. Transpl Int 17, 707–712 (2005). https://doi.org/10.1007/s00147-004-0795-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00147-004-0795-3