Abstract
Purpose
Patients with persistent critical illness may account for up to half of all intensive care unit (ICU) bed-days. It is unknown if there is hospital variation in the development of persistent critical illness and if hospital performance affects the incidence of persistent critical illness.
Methods
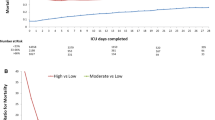
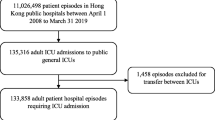
This is a retrospective analysis of Veterans admitted to the Veterans Administration (VA) ICUs from 2015 to 2017. Hospital performance was defined by the risk- and reliability-adjusted 30-day mortality. Persistent critical illness was defined as an ICU length of stay of at least 11 days. We used 2-level multilevel logistic regression models to assess variation in risk- and reliability-adjusted probabilities in the development of persistent critical illness.
Results
In the analysis of 100 hospitals which encompassed 153,512 hospitalizations, 4.9% (N = 7640/153,512) developed persistent critical illness. There was variation in the development of persistent critical illness despite controlling for patient characteristics (intraclass correlation: 0.067, 95% CI 0.049–0.091). Hospitals with higher risk- and reliability-adjusted 30-day mortality had higher probabilities of developing persistent critical illness (predicted probability: 0.057, 95% CI 0.051–0.063, p < 0.01) compared to those with lower risk- and reliability-adjusted 30-day mortality (predicted probability: 0.046, 95% CI 0.041–0.051, p < 0.01). The median odds ratio was 1.4 (95% CI 1.33–1.49) implying that, for two patients with the same physiology on admission at two different VA hospitals, the patient admitted to the hospital with higher adjusted mortality would have 40% greater odds of developing persistent critical illness.
Conclusion
Hospitals with higher risk- and reliability-adjusted 30-day mortality have a higher probability of developing persistent critical illness. Understanding the drivers of this variation may identify modifiable factors contributing to the development of persistent critical illness.


Similar content being viewed by others
References
Nelson JE, Cox CE, Hope AA, Carson SS (2010) Chronic critical illness. Am J Respir Crit Care Med 182(4):446–454
Iwashyna TJ, Hodgson CL, Pilcher D et al (2016) Timing of onset and burden of persistent critical illness in Australia and New Zealand: a retrospective, population-based, observational study. Lancet Respir Med 4(7):566–573
Iwashyna TJ, Hodgson CL, Pilcher D, Bailey M, Bellomo R (2015) Persistent critical illness characterised by Australian and New Zealand ICU clinicians. Crit Care Resusc 17(3):153–158
Nelson JE, Meier DE, Litke A, Natale DA, Siegel RE, Morrison RS (2004) The symptom burden of chronic critical illness. Crit Care Med 32(7):1527–1534
Bagshaw SM, Stelfox HT, Iwashyna TJ, Bellomo R, Zuege D, Wang X (2018) Timing of onset of persistent critical illness: a multi-centre retrospective cohort study. Intensive Care Med 44(12):2134–2144
Viglianti EM, Zajic P, Iwashyna TJ, Amrein K (2019) Neither vitamin D levels nor supplementation are associated with the development of persistent critical illness: a retrospective cohort analysis. Crit Care Resusc 21(1):39–44
Viglianti EM, Kramer R, Admon AJ et al (2018) Late organ failures in patients with prolonged intensive care unit stays. J Crit Care 46:55–57
Darvall JN, Boonstra T, Norman J et al (2019) Persistent critical illness: baseline characteristics, intensive care course, and cause of death. Crit Care Resusc 21(2):110–118
Brochard L, Thille AW (2009) What is the proper approach to liberating the weak from mechanical ventilation? Crit Care Med 37(10 Suppl):S410–S415
Stefos T, Lehner L, Render M, Moran E, Almenoff P (2012) Determining population based mortality risk in the Department of Veterans Affairs. Health Care Manag Sci 15(2):121–137
Sakusic A, Gajic O (2016) Chronic critical illness: unintended consequence of intensive care medicine. Lancet Respir Med 4(7):531–532
Rose L, Istanboulian L, Allum L et al (2019) Patient and family centered actionable processes of care and performance measures for persistent and chronic critical illness: a systematic review. Crit Care Explor 1(4):e0005
Render ML, Deddens J, Freyberg R et al (2008) Veterans Affairs intensive care unit risk adjustment model: validation, updating, recalibration. Crit Care Med 36(4):1031–1042
Render ML, Kim HM, Deddens J et al (2005) Variation in outcomes in Veterans Affairs intensive care units with a computerized severity measure. Crit Care Med 33(5):930–939
Kizer KW, Fonseca ML, Long LM (1997) The veterans healthcare system: preparing for the twenty-first century. Hosp Health Serv Adm 42(3):283–298
US Department of Veteran Affairs. Veteran Health Administration. https://www.va.gov/health/aboutvha.asp. Published 2018. Accessed 2 July 2019
Wang XQ, Vincent BM, Wiitala WL et al (2019) Veterans affairs patient database (VAPD 2014–2017): building nationwide granular data for clinical discovery. BMC Med Res Methodol 19(1):94
Viglianti EM, Bagshaw SM, Bellomo R et al (2020) Late vasopressor administration in ICU patients: a retrospective cohort study. Chest S0012-3692(20)30591-2. https://doi.org/10.1016/j.chest.2020.02.071
Knaus WA, Zimmerman JE, Wagner DP, Draper EA, Lawrence DE (1981) APACHE-acute physiology and chronic health evaluation: a physiologically based classification system. Crit Care Med 9(8):591–597
van Walraven C, Austin PC, Jennings A, Quan H, Forster AJ (2009) A modification of the Elixhauser comorbidity measures into a point system for hospital death using administrative data. Med Care 47(6):626–633
Dimick JB, Staiger DO, Birkmeyer JD (2010) Ranking hospitals on surgical mortality: the importance of reliability adjustment. Health Serv Res 45(6 Pt 1):1614–1629
Dimick JB, Birkmeyer NJ, Finks JF et al (2014) Composite measures for profiling hospitals on bariatric surgery performance. JAMA Surg 149(1):10–16
Prescott HC, Kepreos KM, Wiitala WL, Iwashyna TJ (2015) Temporal changes in the influence of hospitals and regional healthcare networks on severe sepsis mortality. Crit Care Med 43(7):1368–1374
Merlo J, Chaix B, Ohlsson H et al (2006) A brief conceptual tutorial of multilevel analysis in social epidemiology: using measures of clustering in multilevel logistic regression to investigate contextual phenomena. J Epidemiol Community Health 60(4):290–297
Hayward RA, Heisler M, Adams J, Dudley RA, Hofer TP (2007) Overestimating outcome rates: statistical estimation when reliability is suboptimal. Health Serv Res 42(4):1718–1738
Merlo J, Yang M, Chaix B, Lynch J, Rastam L (2005) A brief conceptual tutorial on multilevel analysis in social epidemiology: investigating contextual phenomena in different groups of people. J Epidemiol Commun Health 59(9):729–736
Larsen K, Merlo J (2005) Appropriate assessment of neighborhood effects on individual health: integrating random and fixed effects in multilevel logistic regression. Am J Epidemiol 161(1):81–88
Walkey AJ, Wiener RS (2014) Hospital case volume and outcomes among patients hospitalized with severe sepsis. Am J Respir Crit Care Med 189(5):548–555
Gaieski DF, Edwards JM, Kallan MJ, Mikkelsen ME, Goyal M, Carr BG (2014) The relationship between hospital volume and mortality in severe sepsis. Am J Respir Crit Care Med 190(6):665–674
Kahn JM, Werner RM, Carson SS, Iwashyna TJ (2012) Variation in long-term acute care hospital use after intensive care. Med Care Res Rev 69(3):339–350
Makam AN, Nguyen OK, Xuan L, Miller ME, Goodwin JS, Halm EA (2018) Factors associated with variation in long-term acute care hospital vs skilled nursing facility use among hospitalized older adults. JAMA Intern Med 178(3):399–405
Kahn JM, Barnato AE, Lave JR et al (2015) A comparison of free-standing versus co-located long-term acute care hospitals. PLoS ONE 10(10):e0139742
Viglianti EM, Kruser JM, Iwashyna T (2019) The heterogeneity of prolonged ICU hospitalisations. Thorax 74:1015–1017
Iwashyna TJ, Viglianti EM (2018) Patient and population-level approaches to persistent critical illness and prolonged intensive care unit stays. Crit Care Clin 34(4):493–500
Zampieri FG, Iwashyna TJ, Viglianti EM et al (2018) Association of frailty with short-term outcomes, organ support and resource use in critically ill patients. Intensive Care Med 44(9):1512–1520
Muscedere J, Waters B, Varambally A et al (2017) The impact of frailty on intensive care unit outcomes: a systematic review and meta-analysis. Intensive Care Med 43(8):1105–1122
Silber JH, Williams SV (1992) Hospital and patient characteristics associated with death after surgery—a study of adverse occurrence and failure to rescue. Med Care 30(7):615–629
Ghaferi AA, Birkmeyer JD, Dimick JB (2009) Variation in hospital mortality associated with inpatient surgery. N Engl J Med 361(14):1368–1375
Funding
This work was supported by Grants NHLBI T32 HL7749-25 (EMV), K12 HL138039 (EMV, TJI). Dr. Bagshaw is supported by a Canada Research Chair in Critical Care Nephrology.
Author information
Authors and Affiliations
Contributions
EMV designed the study, performed the statistical analyses, interpreted the results, compiled the manuscript, and is accountable for all aspects of the work. SMB interpreted the results and provided critical revisions for the manuscript. RB interpreted the results and provided critical revisions for the manuscript. JM interpreted the results and provided critical revisions for the manuscript. XQW performed statistical analyses and provided critical revisions for the manuscript. SS refined the analysis, assisted in interpreting the findings, and provided critical revisions for the manuscript. TJI consulted on the design of the study, refined the analyses, assisted in interpreting the findings, and provided critical revisions of the manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest. This work does not represent the official views of the US Government or the US Department of Veteran Affairs.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Viglianti, E.M., Bagshaw, S.M., Bellomo, R. et al. Hospital-level variation in the development of persistent critical illness. Intensive Care Med 46, 1567–1575 (2020). https://doi.org/10.1007/s00134-020-06129-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-020-06129-9