Abstract
Purpose
Relatives of intensive care unit (ICU) patients suffer emotional distress that impairs their ability to acquire the information they need from the staff. We sought to evaluate whether providing relatives with a list of important questions was associated with better comprehension on day 5.
Methods
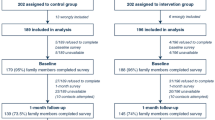
Randomized, parallel-group trial. Relatives of mechanically ventilated patients were included from 14 hospitals belonging to the FAMIREA study group in France. A validated list of 21 questions was handed to the relatives immediately after randomization. The primary endpoint was comprehension on day 5. Secondary endpoints were satisfaction (Critical Care Family Needs Inventory, CCFNI) and symptoms of anxiety and depression (Hospital Anxiety and Depression Scale, HADS).
Results
Of 394 randomized relatives, 302 underwent the day-5 assessment of all outcomes. Day-5 family comprehension was adequate in 68 (44.2%) and 75 (50.7%) intervention and control group relatives (P = 0.30), respectively. Over the first five ICU days, median number of family–staff meetings/patient was 6 [3–9], median total meeting time was 72.5 [35–110] min, and relatives asked a median of 20 [8–33] questions including 11 [6–13] from the list, with no between-group difference. Satisfaction and anxiety/depression symptoms were not significantly different between groups. The only variable significantly associated with better day-5 comprehension by multivariable analysis was a higher total number of questions asked before day 5.
Conclusions
Providing relatives with a list of questions did not improve day-5 comprehension, secondary endpoints, or information time. Further research is needed to help families obtain the information they need.
Trial registration
ClinicalTrials.gov Identifier: NCT02410538.



Similar content being viewed by others
References
Davidson JE, Aslakson RA, Long AC et al (2017) Guidelines for family-centered care in the neonatal, pediatric, and adult ICU. Crit Care Med 45:103–128. https://doi.org/10.1097/CCM.0000000000002169
Pochard F, Azoulay E, Chevret S et al (2001) Symptoms of anxiety and depression in family members of intensive care unit patients: ethical hypothesis regarding decision-making capacity. Crit Care Med 29:1893–1897
Azoulay E, Pochard F, Kentish-Barnes N et al (2005) Risk of post-traumatic stress symptoms in family members of intensive care unit patients. Am J Respir Crit Care Med 171:987–994. https://doi.org/10.1164/rccm.200409-1295OC
Azoulay E, Pochard F, Chevret S et al (2001) Meeting the needs of intensive care unit patient families: a multicenter study. Am J Respir Crit Care Med 163:135–139. https://doi.org/10.1164/ajrccm.163.1.2005117
Lautrette A, Darmon M, Megarbane B et al (2007) A communication strategy and brochure for relatives of patients dying in the ICU. N Engl J Med 356:469–478. https://doi.org/10.1056/NEJMoa063446
Netzer G, Sullivan DR (2014) Recognizing, naming, and measuring a family intensive care unit syndrome. Ann Am Thorac Soc 11:435–441. https://doi.org/10.1513/AnnalsATS.201309-308OT
Azoulay E, Pochard F, Chevret S et al (2002) Impact of a family information leaflet on effectiveness of information provided to family members of intensive care unit patients: a multicenter, prospective, randomized, controlled trial. Am J Respir Crit Care Med 165:438–442. https://doi.org/10.1164/ajrccm.165.4.200108-006oc
Curtis JR, Treece PD, Nielsen EL et al (2016) Randomized trial of communication facilitators to reduce family distress and intensity of end-of-life care. Am J Respir Crit Care Med 193:154–162. https://doi.org/10.1164/rccm.201505-0900OC
Connors AF, Dawson NV, Desbiens NA, Fulkerson WJ, Goldman L, Knaus WA, Lynn J, Oye RK, Bergner M, Damiano A, Hakim R, et al. (1995) A controlled trial to improve care for seriously ill hospitalized patients. The study to understand prognoses and preferences for outcomes and risks of treatments (SUPPORT). The SUPPORT Principal Investigators. JAMA 274:1591–1598
Peigne V, Chaize M, Falissard B et al (2011) Important questions asked by family members of intensive care unit patients. Crit Care Med 39:1365–1371. https://doi.org/10.1097/CCM.0b013e3182120b68
Rodriguez RM, Navarrete E, Schwaber J et al (2008) A prospective study of primary surrogate decision makers’ knowledge of intensive care. Crit Care Med 36:1633–1636. https://doi.org/10.1097/CCM.0b013e31816a0784
Azoulay E, Chevret S, Leleu G et al (2000) Half the families of intensive care unit patients experience inadequate communication with physicians. Crit Care Med 28:3044–3049
Kentish-Barnes N, Chevret S, Azoulay E (2016) Impact of the condolence letter on the experience of bereaved families after a death in intensive care: study protocol for a randomized controlled trial. Trials 17:102. https://doi.org/10.1186/s13063-016-1212-9
Kentish-Barnes N, Chaize M, Seegers V et al (2015) Complicated grief after death of a relative in the intensive care unit. Eur Respir J 45:1341–1352. https://doi.org/10.1183/09031936.00160014
Azoulay E, Pochard F (2002) Meeting the needs of intensive care unit patients’ family members: beyond satisfaction. Crit Care Med 30:2171. https://doi.org/10.1097/01.CCM.0000026738.53285.D9
Moreau D, Goldgran-Toledano D, Alberti C et al (2004) Junior versus senior physicians for informing families of intensive care unit patients. Am J Respir Crit Care Med 169:512–517. https://doi.org/10.1164/rccm.200305-645OC
Howell AA, Nielsen EL, Turner AM et al (2014) Clinicians’ perceptions of the usefulness of a communication facilitator in the intensive care unit. Am J Crit Care 23:380–386. https://doi.org/10.4037/ajcc2014517
Curtis JR, Engelberg RA, Wenrich MD et al (2002) Studying communication about end-of-life care during the ICU family conference: development of a framework. J Crit Care 17:147–160
Lilly CM, De Meo DL, Sonna LA et al (2000) An intensive communication intervention for the critically ill. Am J Med 109:469–475
Lilly CM, Sonna LA, Haley KJ, Massaro AF (2003) Intensive communication: 4-year follow-up from a clinical practice study. Crit Care Med 31:S394–399. https://doi.org/10.1097/01.CCM.0000065279.77449.B4
Bosslet GT, Pope TM, Rubenfeld GD et al (2015) An official ATS/AACN/ACCP/ESICM/SCCM policy statement: responding to requests for potentially inappropriate treatments in intensive care units. Am J Respir Crit Care Med 191:1318–1330. https://doi.org/10.1164/rccm.201505-0924ST
Kentish-Barnes N, Chevret S, Champigneulle B et al (2017) Effect of a condolence letter on grief symptoms among relatives of patients who died in the ICU: a randomized clinical trial. Intensive Care Med 43:473–484. https://doi.org/10.1007/s00134-016-4669-9
Funding
The study was funded by the French Ministry of Health, which had no role in the study design, conduct, interpretation, reporting, or publication decisions.
Author information
Authors and Affiliations
Contributions
Authors have participated in the design (EA, LP, NKB, MM, EJ), acquisition (JMF, IV, AR, SV, SJ, JDG, CS, HG, SM, AC, SH, LA, ML), analysis (EA, LP, NKB, MM, EJ), and interpretation of the data (EA, LP, NKB, MM, EJ, JRC). All have participated in drafting and revising the paper. All approved the final version and all are accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflicts of interest
Dr. Azoulay reports personal fees and other from Gilead, personal fees from Astellas, personal fees from Baxter, personal fees from Alexion, personal fees from Ablynx, outside the submitted work. Other authors declare no conflict of interest.
Ethical standards
The study protocol was approved by the appropriate ethics committee (IFR 48 #13-004, Marseille) and French health authorities (CNIL DR-2013-497; CCTIRS 13.332). The trial was registered on ClinicalTrials.gov (NCT02410538). Informed consent was obtained from all participants.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Azoulay, E., Forel, JM., Vinatier, I. et al. Questions to improve family–staff communication in the ICU: a randomized controlled trial. Intensive Care Med 44, 1879–1887 (2018). https://doi.org/10.1007/s00134-018-5423-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-018-5423-2