Abstract
Purpose
Recent clinical data suggest that terlipressin, a vasopressin analogue, may be more beneficial in septic shock patients than catecholamines. However, terlipressin’s effect on mortality is unknown. We set out to ascertain the efficacy and safety of continuous terlipressin infusion compared with norepinephrine (NE) in patients with septic shock.
Methods
In this multicentre, randomised, double-blinded trial, patients with septic shock recruited from 21 intensive care units in 11 provinces of China were randomised (1:1) to receive either terlipressin (20–160 µg/h with maximum infusion rate of 4 mg/day) or NE (4–30 µg/min) before open-label vasopressors. The primary endpoint was mortality 28 days after the start of infusion. Primary efficacy endpoint analysis and safety analysis were performed on the data from a modified intention-to-treat population.
Results
Between 1 January 2013 and 28 February 2016, 617 patients were randomised (312 to the terlipressin group, 305 to the NE group). The modified intention-to-treat population comprised 526 (85.3%) patients (260 in the terlipressin group and 266 in the NE group). There was no significant difference in 28-day mortality rate between the terlipressin group (40%) and the NE group (38%) (odds ratio 0.93 [95% CI 0.55–1.56]; p = 0.80). Change in SOFA score on day 7 was similar between the two groups: − 7 (IQR − 11 to 3) in the terlipressin group and − 6 (IQR − 10 to 5) in the NE group. There was no difference between the groups in the number of days alive and free of vasopressors. Overall, serious adverse events were more common in the terlipressin group than in the NE group (30% vs 12%; p < 0.001).
Conclusions
In this multicentre, randomised, double-blinded trial, we observed no difference in mortality between terlipressin and NE infusion in patients with septic shock. Patients in the terlipressin group had a higher number of serious adverse events.
Trial registration
This trial is registered at ClinicalTrials.gov: ID NCT01697410.
Similar content being viewed by others
Up to now, this multicenter, randomized, double-blind trial is the largest study regarding efficacy and safety of continuous terlipressin infusion in septic shock.We did not find a significant reduction in 28-day mortality rate with terlipressin. Terlipressin is effective in reversing sepsis-induced arterial hypotension. Furthermore, compared to norepinephrine, terlipressin treatment improved serum creatine and SOFA score. Digital ischemia must be intensively monitored during terlipressin treatment. The dosing regimen and safety of continuous terlipressin infusion in septic shock need to be further investigated. |
Introduction
Despite the significant progress made in intensive care medicine, septic shock remains associated with high morbidity and mortality [1,2,3]. To correct hypotension in septic shock, norepinephrine (NE) is the first-line recommended vasopressor [4]. However, achieving the arterial blood pressure target may require high doses of NE, which may result in myocardial injury and alter the sepsis-associated immunomodulation [5].
Vasopressin, an endogenously released peptide hormone, has emerged as a potential adjunct to NE in case of refractory hypotension or when the dose of NE needed to reach the arterial blood pressure target is judged to be high [4]. The recent Vasopressin (Arginine vasopressin, AVP) and Septic Shock Trial (VASST) failed to show benefit of vasopressin compared to NE [6], while the VANISH randomized clinical trial demonstrated that early vasopressin reduced the use of renal replacement therapy in patients with septic shock [7]. Vasopressin may stimulate multiple receptors, namely V1 receptors, V2 receptors, oxytocin receptors, and purinergic receptors, and activation of the V1 receptor leads to vasoconstriction and arterial blood pressure increase [8]. However, AVP has no selectivity for the V1 receptor and may have side effects due to activation of the other receptors [9, 10]. Terlipressin, a synthetic, long-acting vasopressin analogue, has a much higher affinity to the V1 receptor than to other receptors [8]. Preliminary clinical analysis has shown that terlipressin effectively reduces the NE requirements in patients with septic shock [11, 12]. A recent meta-analysis found that the use of terlipressin and vasopressin, compared to NE, may decrease mortality in patients with septic shock [13]. However, another meta-analysis failed to confirm these results [14]. Until now, there has been no trial powered enough to evaluate the effect of terlipressin on mortality, organ dysfunction or safety in septic shock patients.
To determine the efficiency of terlipressin versus NE in septic shock, we conducted a multicentre, randomised, double-blind trial with 28-day mortality as the primary outcome.
Methods
Study design and participants
This prospective, multicentre, randomised, double-blind trial was conducted between January 2013 and February 2016 in 21 intensive care units in 11 provinces of China. The medical ethics research committee of the First Affiliated Hospital of Sun Yat-sen University approved the study with subsequent sanctioning of all participating hospitals.
Patients older than 18 years diagnosed with septic shock during their ICU stay were considered for enrolment. Septic shock was defined by the presence of two or more diagnostic criteria for the systemic inflammatory response syndrome. Proven or suspected infection, and hypotension despite adequate fluid resuscitation (sepsis-induced hypotension defined as systolic blood pressure (SBP) < 90 mmHg or mean arterial pressure < 70 mmHg or an SBP decrease > 40 mmHg or > 2SD below normal for age in the absence of other causes of hypotension) [15]. Exclusion criteria included (1) unstable coronary syndrome (acute myocardial infarction during this episode of shock based on the combination of history, electrocardiogram and enzyme changes, (2) previous use of terlipressin for arterial blood pressure support during the current ICU admission, (3) malignancy or other irreversible disease or condition for which mortality was estimated to be very high (defined by investigator), (4) acute mesenteric ischaemia either proven or suspected, (5) Raynaud’s phenomenon, (6) pregnancy, (7) organ transplantation. For all patients informed consent was obtained and signed by their next of kin, or another surrogate decision maker, before entering the study. The trial was registered with ClinicalTrials.gov, number NCT01697410.
Randomisation and masking
We randomly assigned patients who met eligibility criteria to receive either terlipressin or NE. Randomisation was done with sequentially numbered, opaque, computer-generated sealed envelopes. The allocation sequence was concealed from the researchers. To reduce the impact on the results from heterogeneity of septic shock and inter-hospital variation as much as possible, stratification by the investigating centre in combination with block randomisation (block size = 10) according to the sequence of recruitment was employed in the enrolment process. Eligible patients were randomly assigned in a 1:1 ratio in each hospital with randomisation stratified by study centre. The random number was written on the sealed randomisation envelopes. Once the patient was included in the study, the sealed envelope was handed over to an independent pharmaceutical nurse who worked in an isolated pharmacy. This pharmaceutical nurse prepared the study medication according to the allocated group written on a card inside the envelope, wrote the random number of the included patient on a confidential medication form, and then resealed the envelope. Subsequently, the sealed envelope and medication form were locked in an independent safe box in the pharmacy. The study drug was prepared in a standard 50-mL syringe and the drug solution was colourless and transparent. The clinical staffs, investigators, researchers, patients and their families who were involved in this study were strictly masked to the treatment assignment during the trial period. Clinicians who enrolled the subjects were not involved in data collection. To prevent advance knowledge of treatment assignment and subversion of the allocation sequence, the trial entry sheet of the case report form (CRF) was filled out and informed consent was obtained before disclosing the unique participant number and allocation; the unique number generated could not be changed or deleted afterward.
Procedures and sepsis management
Terlipressin (1 mg) or NE (11 mg) was dissolved in a 50-mL syringe containing 5% dextrose in water, with final concentrations of 0.02 mg of terlipressin per mL and 0.22 mg of NE per mL. The terlipressin or NE infusion was colourless and transparent. Therefore the study drug could not be identified by appearance of the syringe. Infusion was started at 1 mL/h and titrated to achieve the target blood pressure. The maximum infusion rate of the study drug was 8 mL/h. Thus, the terlipressin infusion was started at 20 µg/h and titrated to a maximum of 160 µg/h, whereas the NE infusion was started at 4 μg/min and titrated to a maximum of 30 µg/min. In several previous studies, a 1-mg terlipressin bolus was given to maintain blood pressure in septic shock every 6 h [8, 11]. The half-life terlipressin is 6 h [8]. Therefore, the maximum dosage of continuous terlipressin infusion was 4 mg/day in our study. The study drugs were manufactured and distributed by Hybio Phamaceutical (Shenzhen, China) to the participating hospital pharmacies.
An initial target mean arterial pressure of 65–75 mmHg was recommended. However, the ICU physician was allowed to modify the target arterial blood pressure of each patient. The study drug was given first to achieve the target blood pressure. During the initiation and titration of the study drug, the bedside nurse was allowed to administer open-label NE in case the recommended mean arterial pressure was not reached on maximal study drug infusion. Other open-label vasopressors such as dopamine and epinephrine were allowed to be added if the maximum doses of both the study drug and the open-label NE were not effective to achieve or maintain the target blood pressure. Tapering of open-label vasopressors was permitted only when the target mean arterial pressure had been reached during the study drug infusion. Tapering of the study drug was commenced only when the target mean arterial pressure had been maintained for 12 h without any open-label vasopressors. However, the ICU physician or nurse could modify the titration speed according to the variation of arterial blood pressure.
The study drug infusion was interrupted if any of the following serious adverse events occurred: acute ST-segment elevation confirmed by a 12-lead electrocardiogram, serious or life-threatening (haemodynamically unstable) cardiac arrhythmias, acute mesenteric ischaemia, digital ischaemia or severe diarrhoea. If the clinical team noted any of the aforementioned adverse events that they considered to be related to the study drug, the study drug was discontinued for at least 12 h and a serious adverse event was reported. The study drug could be resumed if the adverse event had been controlled and the event was deemed to be unrelated to the study drug or the study protocol as judged by the investigators.
If vasopressor support was required during the same admission to the ICU after a patient had been already weaned from the study drug, the study drug was preferentially re-infused, as long as no exclusion criterion was met. The treatment of sepsis followed the current international guidelines [13].
Outcomes
The primary outcome was death from any cause and was assessed 28 days after the start of study drug infusion. Secondary outcomes included changes in the Sequential Organ Failure Assessment (SOFA) score on day 7 after randomisation and days alive and free of vasopressor during 28 days after randomisation. We also evaluated the incidence of serious adverse events.
Statistical analysis
On the basis of a previous study [1], a sample size of 1000 patients was originally calculated to show a reduction in 28-day mortality rate from 50% to 40% by terlipressin treatment, with a two-sided test (error = 5%; power = 80%). Considering a possible drop-out rate of 10%, the trial would need to enrol 1100 patients. An independent data and safety monitoring committee reviewed the safety and efficacy data. Formal interim analyses were scheduled after approximately 30%, 50%, 80% and 100% of intention-to-treat patient data had accrued. An O’Brien–Fleming approach was used for sequential stopping rules for safety and efficacy according to the Lan–DeMets method [16]. The study would continue until the final analysis if a stopping boundary was not crossed at the interim analysis.
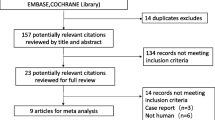
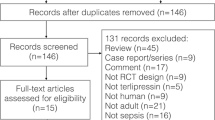
The primary analysis, which compared 28-day mortality between the two treatment groups, was performed using an unadjusted chi-square test. The analyses were performed on data from the modified intention-to-treat population, defined as all randomly assigned patients with at least once infusion except those who could be excluded without the risk of bias [17] (patients who were confirmed to be ineligible and did not receive the study infusion) and those for whom we did not have consent for the use of data (Fig. 1). Results are presented as absolute and relative risks and 95% confidence intervals.
A logistic regression procedure and significant covariates that predicted outcomes were used to adjust raw values for 28-day mortality. Age, illness severity (Acute Physiology and Chronic Health Evaluation II [APACHE II] score at baseline), serious coexisting conditions and other baseline covariates that predicted outcome were entered into the model. Results are presented as odds ratios and 95% confidence intervals. Parametric procedures (independent t test) and repeated-measures analysis of variance were used to compare all secondary outcomes.
The data analyst and investigators remained unaware of the treatment assignments while undertaking the final analyses. Analysis was conducted with the use of SAS software (version 9.1.3), and all p values were two-sided. Guangzhou Hipower Pharmaceutical R&D Co. Ltd as a data monitoring committee supervised the study.
Role of funding source
The funder of the study had no role in study design, data collection, data analysis, data interpretation or writing of the report. The corresponding author had full access to all the study’s data and had the final responsibility for the decision to submit for publication.
Results
Enrolment started in January 2013. Two planned interim analyses were conducted after approximately 300 and 600 patients had been enrolled. In the second interim analysis, the data and safety monitoring board reviewed intention-to-treat data on the 28-day mortality rate. Two-sided O'Brien–Fleming boundaries were used to assess potential early stopping of the trial. Using SAS software, this interim analysis fulfilled the stopping rules of p < 0.0036 for efficacy and p > 0.2235 for futility. The observed p value (see results below) fell within the futility region. On the basis of all available data, the data and safety monitoring board recommended cessation of the trial. Recruitment was stopped early at 50% enrolment in February 2016.
Between 1 January 2013 and 28 February 2016, among 684 eligible patients, 617 were randomised after providing informed consent. Among these 617 patients, 13 withdrew their consent, 21 did not receive the study drug infusion because of rapid improvement, 13 were confirmed ineligible and 35 were withdrawn from care without infusion. Thus 535 patients underwent randomisation and infusion of the study drug. Out of these 535 patients, five withdrew their consent and four were lost to follow-up. Thus, 526 patients were included in the final primary analysis: 260 patients were randomised to the terlipressin group and 266 to the NE group (Fig. 1). The baseline characteristics of the two groups are shown in Table 1. Enrolled patients were severely ill, as indicated by the APACHE II and SOFA scores and the serum lactate concentration at inclusion, the incidence of organ dysfunction and the incidence of comorbidities. The most common sites of infection were lung and abdomen, with an incidence of 51% and 54%, respectively, and with mixed pathogens or Gram-negative organisms accounting for the majority of cases (Table 1).
Arterial blood pressure and serum lactate during the first 7 days of the study in the two treatment groups are shown in Fig. 2.
Outcomes
There was no significant difference in the primary outcome between the terlipressin group and the NE group (40% vs 38%, respectively; p = 0.633) (Table 2). The absolute risk difference between the terlipressin group and the NE group was 2% (95% CI − 9.8% to 18.8%). The relative risk was 1.053 (95% CI 0.742–1.496). The results remained nonsignificant after multivariate logistic regression analysis (odds ratio for death in the terlipressin group at 28 days, 0.93 [95% CI 0.55–1.60]). Compared to baseline, the SOFA score on day 7 after randomisation was improved in both groups (p < 0.05). The change in SOFA score on day 7 after randomisation was similar between groups, − 7 (IQR − 11 to 3) in the terlipressin group and − 6 (IQR − 10 to 5) in the NE group (Table 2). Days alive and free of vasopressor were similar between groups (Table 2).
More patients in the terlipressin group had serious adverse events than in the NE group (30% vs 12%, p < 0.01; Table 3). Thirty-three out of 260 (12.6%) patients who received terlipressin infusion experienced digital ischaemia after the start of infusion versus only one in the NE group (p < 0.0001) (Table 3). Globally, 76% of digital ischaemia emerged during the first 24 h after the start of infusion. Out of the 33 patients, 31 (94%) with digital ischaemia received an open-label vasopressor in addition to the study drug to maintain the target arterial blood pressure. No patient with digital ischaemia required surgical intervention. Severe diarrhoea was more common in the terlipressin group than in the NE group (p < 0.05). There were no significant differences in the overall rates of serious arrhythmia, intestinal ischaemia and hyponatraemia between the two groups (Table 3).
Furthermore, we did some post hoc analyses of other outcomes, the results of which were presented in the supplement.
Discussion
To the best of our knowledge, our study of continuous terlipressin infusion in patients with septic shock is the largest randomised, controlled, double-blind, multicentre study conducted so far. Continuous administration of terlipressin compared to NE in patients with septic shock did not decrease 28-day mortality. The changes in SOFA score on day 7 after randomisation were similar in the two groups. Serious adverse events were more common in the terlipressin group.
We set up the study to detect an absolute difference in 28-day mortality of 10% from an expected 50% as indicated in previous trials [1]. However, the observed mortality rates in both the terlipressin and NE groups were lower compared to previous studies [1, 2]. The reduction of mortality rates might be possibly due to an overall improvement in the care of patients with septic shock over the years. Furthermore, the mortality rates of septic shock varied among studies from different regions [1, 7, 18]. The current study showed the 28-day mortality of septic shock in mainland of China. The absolute difference of 28-day mortality rate between the groups was, however, only 2%.
The SOFA score is the predominant severity score currently used during sepsis [3]. A higher SOFA score is associated with an increased probability of death [19]. Rapid improvement in SOFA score has been associated with lower mortality rates [20, 21]. The current trial demonstrates that compared to baseline, the SOFA score on day 7 after randomisation was improved in both the terlipressin group and NE group. Furthermore, the improvements of SOFA score on day 7 after randomisation were similar between groups. Animal experiments showed evidence that terlipressin might protect organ function by improving myocardial contractility, renal function and vascular leakage in septic shock [22,23,24]. The VANISH randomized clinical trial was the latest trail to evaluate the effect of early vasopressin vs norepinephrine on renal function in patients with septic shock. Among adults with septic shock, the early use of vasopressin compared with norepinephrine reduced the use of renal replacement therapy [7]. In the post hoc analyses of our trial (presented in the supplement), we found a greater reduction of serum creatinine on days 5 and 7 after randomisation in the terlipressin group compared to the NE group. However, we failed to demonstrate a reduction in renal replacement therapy or acute kidney injury with terlipressin. Recently, in a phase IIa randomised, placebo-controlled trial in septic shock patients, selepressin, a novel selective vasopressin V1A agonist, may improve fluid balance and shorten the time of mechanical ventilation [25]. Our post hoc analyses failed to find the benefits of terlipressin on fluid balance and mechanical ventilation.
One of the main results of our study was the significantly higher rate of serious adverse events, in particular the digital ischaemia, in the terlipressin group compared to the NE group. However, no patient needed surgical interventions for digital ischaemia. Previous reports show that serious ischaemic adverse events associated with terlipressin, such as skin ischaemia involving the extremities, scrotum, trunk and abdominal skin, are rarely observed [26]. At least two reasons may be responsible for the high rate of terlipressin-associated digital ischaemia in our septic shock patients. Firstly, 94% patients with digital ischaemia received terlipressin and open-label NE treatment at the same time. Such a combination may cause massive peripheral vasoconstriction, thus promoting the risk of ischaemia. Secondly, the dosage of terlipressin with a maximum of 4 mg/day in our trial was higher than the maximum of 1–2 mg/day reported in previous studies [11, 12, 27, 28]. High dosage may lead to increased vasoconstriction and ultimately in peripheral ischaemia. It is noteworthy that other adverse effects including myocardial infarction or ischaemia and life-threatening arrhythmia were rare in both groups of our study. Exclusion of patients who had acute coronary syndromes could account for the lack of adverse cardiovascular effects in our trial.
Several limitations of our trial should be mentioned. Firstly, terlipressin is a synthetic, long-acting vasopressin analogue with high affinity to the V1 receptor. No equivalent dose of terlipressin compared to NE or vasopressin has been reported. We could not measure the serum level of terlipressin as a guide to estimate the dose and duration effect. Secondly, the sample size was originally designed for the primary endpoint. As a result of the small difference in the primary endpoint between the two groups, the trial was terminated at 50% enrolment. Therefore, the study might be underpowered for the outcomes analysis. Thirdly, the SOFA score of circulation was calculated according to the dosage of NE or dopamine. In this trial, however, the investigators were blinded to the experimental drugs. Therefore, on the basis of our protocol, they treated all the experimental drugs as NE, and subsequently calculated SOFA score according to infusion dose of the drug. This method might disturb the accuracy of SOFA score. Furthermore, the relatively high number of exclusions after randomisation in our modified intention-to-treat population might influence the accuracy of our conclusions.
In conclusion, we evaluated the effect of continuous terlipressin infusion (maximum 4 mg/day) compared to NE in patients with septic shock. We did not find a significant reduction in 28-day mortality rate with terlipressin. Change in SOFA score on day 7 after randomisation was similar in both the norepinephrine and terlipressin group. We observed higher rates of serious adverse events, in particular digital ischaemia, in the terlipressin group as compared to the NE group. The dosing regimen and safety of continuous terlipressin infusion in septic shock need to be further investigated.
References
Annane D, Aegerter P, Jars-Guincestre MC, Guidet B (2003) Current epidemiology of septic shock: the CUB-Réa network. Am J Respir Crit Care Med 168:165–172
Vincent JL, Sakr Y, Sprung CL (2006) Sepsis in European intensive care units: results of the SOAP study. Crit Care Med 34:344
Singer M, Deutschman CS, Seymour CW et al (2016) The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA 315:801–810
Rhodes A, Evans LE, Alhazzani W et al (2017) Surviving Sepsis Campaign: international guidelines for management of sepsis and septic shock: 2016. Intensive Care Med 43:304–377
Mullner M, Urbanek B, Havel C, Losert H et al (2004) Vasopressors for shock. Cochrane Datab Syst Rev 3:CD3709
Russell JA, Walley KR, Singer J et al (2008) Vasopressin versus norepinephrine infusion in patients with septic shock. N Engl J Med 358:877–887
Gordon AC, Mason AJ, Thirunavukkarasu N et al (2016) Effect of early vasopressin vs norepinephrine on kidney failure in patients with septic shock: the VANISH randomized clinical trial. JAMA 316:509–518
Lange Matthias, Ertmer Christian, Westphal Martin (2009) Vasopressin vs. terlipressin in the treatment of cardiovascular failure in sepsis. Intensive Care Med 34:821–832
Torgersen C, Dunser MW, Wenzel V et al (2010) Comparing two different arginine vasopressin doses in advanced vasodilatory shock: a randomized, controlled, open-label trial. Intensive Care Med 36:57
Salazar M, Hu BB, Vazquez J et al (2015) Exogenous vasopressin-induced hyponatremia in patients with vasodilatory shock: two case reports and literature review. J Intensive Care Med 30:253
Leone M, Albanèse J, Delmas A et al (2004) Terlipressin in catecholamine-resistant septic shock patients. Shock 22:314–319
Morelli A, Ertmer C, Rehberg S et al (2009) Continuous terlipressin versus vasopressin infusion in septic shock (TERLIVAP): a randomized, controlled pilot study. Crit care 13:R130
Sepra N, Nassar Junior AP, Cardoso SO et al (2012) Vasopressin and terlipressin in adult vasodilatory shock: a systematic review and meta-analysis of nine randomized controlled trials. Crit Care 16:R154
Polito Angelo, Parisini Emilio, Ricci Zaccaria et al (2012) Vasopressin for treatment of vasodilatory shock: an ESICM systematic review and meta-analysis. Intensive Care Med 38:9–19
Surviving Sepsis Campaign Guidelines Committee including The Pediatric Subgroup (2013) Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock: 2012. Intensive Care Med 39:165–228
Gordon Lan KK, Demets DL (1983) Discrete sequential boundaries for clinical trials. Biometrika 70:659–663
Fergusson D, Aaron SD, Guyatt G et al (2002) Post-randomisation exclusions: the intention to treat principle and excluding patients from analysis. BMJ 325:652–654
SepNet Critical Care Trials Group (2016) Incidence of severe sepsis and septic shock in German intensive care units: the prospective, multicentre INSEP study. Intensive Care Med 42:1980–1989
Vincent JL, de Mendonca A, Cantraine F et al (1998) Working Group on “Sepsis-Related Problems” of the European Society of Intensive Care Medicine. Use of the SOFA score to assess the incidence of organ dysfunction/failure in intensive care units: results of a multicenter, prospective study. Crit Care Med 26:1793–1800
Levy MM, Macias WL, Vincent JL et al (2005) Early changes in organ function predict eventual survival in severe sepsis. Crit Care Med 33:2194–2201
Ferreira FL, Bota DP, Bross A, Mélot C, Vincent JL (2001) Serial evaluation of the SOFA score to predict outcome in critically ill patients. JAMA 286:1754–1758
Lange M, Ertmer C, Rehberg S et al (2011) Effects of two different dosing regimens of terlipressin on organ functions in ovine endotoxemia. Inflamm Res 60:429–437
Morelli Andrea, Rocco Monica, Conti Giorgio et al (2004) Effects of terlipressin on systemic and regional haemodynamics in catecholamine-treated hyperkinetic septic shock. Intensive Care Med 30:597–604
Rehberg Sebastian, Ertmer Christian, Köhler Gabriele et al (2009) Role of arginine vasopressin and terlipressin as first-line vasopressor agents in fulminant ovine septic shock. Intensive Care Med 35:1286–1296
Russell JA, Vincent JL, Kjølbye AL et al (2017) Selepressin, a novel selective vasopressin V1A agonist, is an effective substitute for norepinephrine in a phase IIa randomized, placebo-controlled trial in septic shock patients. Crit Care 21:213
Ozel Coskun BD, Karaman A, Gorkem H et al (2014) Terlipressin-induced ischemic skin necrosis: a rare association. Am J Case Rep 15:476–479
Albanèse J, Leone M, Delmas A, Martin C (2005) Terlipressin or norepinephrine in hyperdynamic septic shock: a prospective, randomized study. Crit Care Med 33:1897–1902
Xiao X, Zhang J, Wang Y et al (2016) Effects of terlipressin on patients with sepsis via improving tissue blood flow. J Surg Res 200:274–282
Acknowledgments
We would like to thank all of the doctors, nurses, technicians and patients involved at the participating centres for their dedication to the study. We also thank Xuyu Zhang, Michael Quintel, Ström Christer, JL Teboul, Jianfeng Wu and Yao Nie for their kind help with the manuscript. This study was funded by Sun Yat-sen University Clinical Research Program 5010 (NO 2007015) and by Major Science and Technology Project (NO 2012A080204018) of Guangdong province, China.
Study Group of investigators
Xiang-Dong Guan, Zi-Meng Liu and Juan Chen (The First Affiliated Hospital of Sun Yatsen University); Aihua Lin, Jie Zeng and Yanlin Huang (School of Public Health, Sun Yat-sen University), Qiuye Kou and Enhe Liu (The Sixth Affiliated Hospital of Sun Yatsen University), Qinhan Lin and Jianling Liu (Qingyuan People's Hospital), Xiaobo Huang and Xiaoqin Zhang (Sichuan Academy of Medical Sciences & Sichuan Provincial People’s Hospital), Zhanhong Tang and Yaoping Pan (The First Affiliated Hospital, GuangXi Medical University), Yan Kang and Yao Chen (West China Hospital), Ke Li and Jiji Cheng (Chinese PLA 302 Hospital), Lixin Zhou and Xinhua Qiang (Foshan First Municipal People’s Hospital), Qing Song and Li Wang (Chinese PLA General Hospital), Tongwen Sun (The First Affiliated Hospital, Zhengzhou University), Ling Zhao and Jiwen Zhong (Zhuhai People's Hospital), Xue Wang and Hongli Chen (The First Affiliated Hospital, Xi,An JiaoTong University), Xiandi He and Qiang Wu (The First Affiliated Hospital, Bengbu Medical college), Chunting Wang and Juan Zeng(Shandong Provincial Hospital), Benquan Wu and Jinmei Luo (The Third Affiliated Hospital of Sun Yat-sen University), Jiandong Lin and Zhaohui Fu (Fujian Provincial Hospital), Shiying Yuan(Wuhan Union Hospital, Tongji Medical College, Huazhong University of Science and Technology), Qin Gu and Ning Liu (The Affiliated Drum Tower hospital of Nanjing University Medical school), Kejian Qian (The First Affiliated Hospital, Nanchang University), Xianqing Shi(Guizhou Provincial Hospital), Yongwen Feng and Suiqing Gui (The Second People's Hospital of Shenzhen).
Author information
Authors and Affiliations
Consortia
Contributions
ZL and JC contributed eaqually to this work. ZL, JC and XG designed the research; QK, JC, QL, XH, ZT, YK, KL, LZ, QS, TS, LZ, XW, XH, CW, BW, JL, SY, QG, KQ, XS and YW performed the research and collected data; AL analysed the data; ZL wrote the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
We declare no competing interests.
Electronic supplementary material
Below is the link to the electronic supplementary material.
134_2018_5267_MOESM1_ESM.tif
Comparison of fluid intake between groups. Values are mean ± standard deviation. There were no statistically significant differences between the norepinephrine and terlipressin groups in fluid intake, P = 0.876. The p value for the interaction term (between group and time) was 0.523 (TIFF 492 kb)
134_2018_5267_MOESM2_ESM.tif
Kaplan–Meier estimate of the probability of 28-day survival. P values were calculated with the use of the log-rank test (TIFF 654 kb)
134_2018_5267_MOESM3_ESM.tif
Comparison of serum alanine transaminase (ALT) between groups. Values were presented as median and interquartile range. Between groups, the changes of serum ALT of each day were similar, P = 0.953. The p value for the interaction term (between group and time) was 0.659 (TIFF 496 kb)
134_2018_5267_MOESM4_ESM.tif
Comparison of serum total bilirubin between groups. Values were presented as median and interquartile range. Between groups, the serum bilirubin of each day was similar, P = 0.785. The p value for the interaction term (between group and time) was 0.497 (TIFF 474 kb)
134_2018_5267_MOESM5_ESM.tif
Comparison of serum creatinine between groups. Values were presented as mean ± standard deviation. The serum creatinine level significantly decreased compared to day 0 in both groups, p = 0.000. The reductions in serum creatinine level were more remarkable in the terlipressin group compared to the NE group, P = 0.035. The p value for the interaction term (between group and time) was 0.132 (TIFF 465 kb)
134_2018_5267_MOESM6_ESM.tif
Comparison of serum base excess between groups. Values were presented as median and interquartile range. Compared to baseline, the serum base excess increased significantly both in the norepinephrine and terlipressin groups, P = 0.025. Between groups, the serum base excess of each day was similar, P = 0.892. The p value for the interaction term (between group and time) was 0.444 (TIFF 454 kb)
Rights and permissions
About this article
Cite this article
Liu, ZM., Chen, J., Kou, Q. et al. Terlipressin versus norepinephrine as infusion in patients with septic shock: a multicentre, randomised, double-blinded trial. Intensive Care Med 44, 1816–1825 (2018). https://doi.org/10.1007/s00134-018-5267-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-018-5267-9