Abstract
Purpose
To test the effectiveness of a central venous catheter (CVC) insertion strategy and a hand hygiene (HH) improvement strategy to prevent central venous catheter-related bloodstream infections (CRBSI) in European intensive care units (ICUs), measuring both process and outcome indicators.
Methods
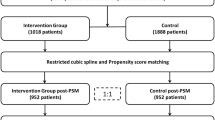
Adult ICUs from 14 hospitals in 11 European countries participated in this stepped-wedge cluster randomised controlled multicentre intervention study. After a 6 month baseline, three hospitals were randomised to one of three interventions every quarter: (1) CVC insertion strategy (CVCi); (2) HH promotion strategy (HHi); and (3) both interventions combined (COMBi). Primary outcome was prospective CRBSI incidence density. Secondary outcomes were a CVC insertion score and HH compliance.
Results
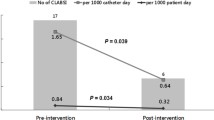
Overall 25,348 patients with 35,831 CVCs were included. CRBSI incidence density decreased from 2.4/1000 CVC-days at baseline to 0.9/1000 (p < 0.0001). When adjusted for patient and CVC characteristics all three interventions significantly reduced CRBSI incidence density. When additionally adjusted for the baseline decreasing trend, the HHi and COMBi arms were still effective. CVC insertion scores and HH compliance increased significantly with all three interventions.
Conclusions
This study demonstrates that multimodal prevention strategies aiming at improving CVC insertion practice and HH reduce CRBSI in diverse European ICUs. Compliance explained CRBSI reduction and future quality improvement studies should encourage measuring process indicators.


Similar content being viewed by others
References
ECDC (2013) Point prevalence survey of healthcare-associated infections and antimicrobial use in European acute care hospitals. European Centre for Disease Prevention and Control, Stockholm
Zingg W, Hopkins S, Gayet-Ageron A, Holmes A, Sharland M, Suetens C, for the ECDC PPS group (2017) Health-care-associated infections in neonates, children, and adolescents: an analysis of paediatric data from the European Centre for Disease Prevention and Control point-prevalence survey. Lancet Infect Dis 17:381–389
Hansen S, Schwab F, Behnke M, Carsauw H, Heczko P, Klavs I, Lyytikainen O, Palomar M, Riesenfeld Orn I, Savey A, Szilagyi E, Valinteliene R, Fabry J, Gastmeier P (2009) National influences on catheter-associated bloodstream infection rates: practices among national surveillance networks participating in the European HELICS project. J Hosp Infect 71:66–73
Hansen S, Schwab F, Gastmeier P, on behalf of the PROHIBIT study group (2015) Provision and consumption of alcohol-based hand rubs in European hospitals. Clin Microbiol Infect 21:1047–1051
Hansen S, Zingg W, Ahmad R, Kyratsis Y, Behnke M, Schwab F, Pittet D, Gastmeier P, on behalf of the PROHIBIT study group (2015) Organization of infection control in European hospitals. J Hosp Infect 91:338–345
Martin M, Zingg W, Hansen S, Gastmeier P, Wu AW, Pittet D, Dettenkofer M, on behalf of the PROHIBIT study group (2013) Public reporting of healthcare-associated infection data in Europe. What are the views of infection prevention opinion leaders? J Hosp Infect 83:94–98
Martin M, Zingg W, Knoll E, Wilson C, Dettenkofer M, on behalf of the PROHIBIT study group (2014) National European guidelines for the prevention of Clostridium difficile infection: a systematic qualitative review. J Hosp Infect 87:212–219
van der Kooi T, Wolkewitz M, van Benthem B, de Greeff S, Grundmann H, Zingg W, on behalf of the PROHIBIT study group (2013) Prohibit (Preventing hospital-acquired infections by intervention and training): preliminary results of a European multi-center study on the effectiveness of a hand hygiene campaign and a central venous catheter bundle (abstract O83). In: International conference of prevention and infection control (ICPIC), Geneva
van der Kooi T, Wolkewitz M, van Benthem B, de Greeff S, Grundmann H, Zingg W, on behalf of the PROHIBIT study group (2014) Unusual distribution of pathogens in a European multi-centre study about central venous catheter-related bloodstream infections (Abstract P0519). In: European congress of clinical microbiology and infectious diseases (ECCMID), Barcelona
van der Kooi T, Wolkewitz M, van Benthem B, de Greeff S, Grundmann H, Zingg W, on behalf of the PROHIBIT study group (2014) The PROHIBIT (Preventing hospital-acquired infections by intervention and training) intervention tria—results of a cluster-randomized European multi-center study on the reduction of central-line related bloodstream infections (Abstract O198). In: European Congress of Clinical Microbiology and Infectious Diseases (ECCMID), Barcelona
Zingg W, Cartier V, Inan C, Touveneau S, Theriault M, Gayet-Ageron A, Clergue F, Pittet D, Walder B (2014) Hospital-wide multidisciplinary, multimodal intervention programme to reduce central venous catheter-associated bloodstream infection. PLoS ONE 9:e93898
Pittet D, Allegranzi B, Storr J (2008) The WHO Clean Care is Safer Care programme: field-testing to enhance sustainability and spread of hand hygiene improvements. J Infect Public Health 1:4–10
ECDC (2010) European surveillance of healthcare-associated infections in intensive care units—HAI-Net ICU protocol, version 1.01. European Centre for Disease Prevention and Control, Stockholm
Sax H, Allegranzi B, Chraiti MN, Boyce J, Larson E, Pittet D (2009) The World Health Organization hand hygiene observation method. Am J Infect Control 37:827–834
Eggimann P, Harbarth S, Constantin MN, Touveneau S, Chevrolet JC, Pittet D (2000) Impact of a prevention strategy targeted at vascular-access care on incidence of infections acquired in intensive care. Lancet 355:1864–1868
Wolkewitz M, Cooper BS, Bonten MJ, Barnett AG, Schumacher M (2014) Interpreting and comparing risks in the presence of competing events. BMJ 349:g5060
Pittet D, Hugonnet S, Harbarth S, Mourouga P, Sauvan V, Touveneau S, Perneger TV (2000) Effectiveness of a hospital-wide programme to improve compliance with hand hygiene. Infection Control Programme. Lancet 356:1307–1312
Ista E, van der Hoven B, Kornelisse RF, van der Starre C, Vos MC, Boersma E, Helder OK (2016) Effectiveness of insertion and maintenance bundles to prevent central-line-associated bloodstream infections in critically ill patients of all ages: a systematic review and meta-analysis. Lancet Infect Dis 16:724–734
Blot K, Bergs J, Vogelaers D, Blot S, Vandijck D (2014) Prevention of central line-associated bloodstream infections through quality improvement interventions: a systematic review and meta-analysis. Clin Infect Dis 59:96–105
Scales DC, Dainty K, Hales B, Pinto R, Fowler RA, Adhikari NK, Zwarenstein M (2011) A multifaceted intervention for quality improvement in a network of intensive care units: a cluster randomized trial. JAMA 305:363–372
Burrell AR, McLaws ML, Murgo M, Calabria E, Pantle AC, Herkes R (2011) Aseptic insertion of central venous lines to reduce bacteraemia. The Central Line Associated Bacteraemia in, N. S. W. Intensive Care Units Collaborative. Med J Aust 194:583–587
Schweizer ML, Reisinger HS, Ohl M, Formanek MB, Blevins A, Ward MA, Perencevich EN (2014) Searching for an optimal hand hygiene bundle: a meta-analysis. Clin Infect Dis 58:248–259
Jeong IS, Park SM, Lee JM, Song JY, Lee SJ (2013) Effect of central line bundle on central line-associated bloodstream infections in intensive care units. Am J Infect Control 41:710–716
Tang HJ, Lin HL, Lin YH, Leung PO, Chuang YC, Lai CC (2014) The impact of central line insertion bundle on central line-associated bloodstream infection. BMC Infect Dis 14:356
Bonello RS, Fletcher CE, Becker WK, Clutter KL, Arjes SL, Cook JJ, Petzel RA (2008) An intensive care unit quality improvement collaborative in nine Department of Veterans Affairs hospitals: reducing ventilator-associated pneumonia and catheter-related bloodstream infection rates. Jt Comm J Qual Patient Saf 34:639–645
Longmate AG, Ellis KS, Boyle L, Maher S, Cairns CJ, Lloyd SM, Lang C (2011) Elimination of central-venous-catheter-related bloodstream infections from the intensive care unit. BMJ Qual Saf 20:174–180
McLaws ML, Burrell AR (2012) Zero risk for central line-associated bloodstream infection: are we there yet? Crit Care Med 40:388–393
Derde LP, Cooper BS, Goossens H, Malhotra-Kumar S, Willems RJ, Gniadkowski M, Hryniewicz W, Empel J, Dautzenberg MJ, Annane D, Aragao I, Chalfine A, Dumpis U, Esteves F, Giamarellou H, Muzlovic I, Nardi G, Petrikkos GL, Tomic V, Marti AT, Stammet P, Brun-Buisson C, Bonten MJ, Team MWS (2014) Interventions to reduce colonisation and transmission of antimicrobial-resistant bacteria in intensive care units: an interrupted time series study and cluster randomised trial. Lancet Infect Dis 14:31–39
Erasmus V, Daha TJ, Brug H, Richardus JH, Behrendt MD, Vos MC, van Beeck EF (2010) Systematic review of studies on compliance with hand hygiene guidelines in hospital care. Infect Control Hosp Epidemiol 31:283–294
Allegranzi B, Gayet-Ageron A, Damani N, Bengaly L, McLaws ML, Moro ML, Memish Z, Urroz O, Richet H, Storr J, Donaldson L, Pittet D (2013) Global implementation of WHO’s multimodal strategy for improvement of hand hygiene: a quasi-experimental study. Lancet Infect Dis 13:843–851
ECDC (2012) Annual epidemiological report. Reporting on 2010 surveillance data and 2011 epidemic intelligence data. European Centre for Disease Prevention and Control, Stockholm
Dudeck MA, Horan TC, Peterson KD, Allen-Bridson K, Morrell G, Anttila A, Pollock DA, Edwards JR (2013) National Healthcare Safety Network report, data summary for 2011, device-associated module. Am J Infect Control 41:286–300
Rosenthal VD, Maki DG, Mehta Y, Leblebicioglu H, Memish ZA, Al-Mousa HH, Balkhy H, Hu B, Alvarez-Moreno C, Medeiros EA, Apisarnthanarak A, Raka L, Cuellar LE, Ahmed A, Navoa-Ng JA, El-Kholy AA, Kanj SS, Bat-Erdene I, Duszynska W, Van Truong N, Pazmino LN, See-Lum LC, Fernandez-Hidalgo R, Di-Silvestre G, Zand F, Hlinkova S, Belskiy V, Al-Rahma H, Luque-Torres MT, Bayraktar N, Mitrev Z, Gurskis V, Fisher D, Abu-Khader IB, Berechid K, Rodriguez-Sanchez A, Horhat FG, Requejo-Pino O, Hadjieva N, Ben-Jaballah N, Garcia-Mayorca E, Kushner-Davalos L, Pasic S, Pedrozo-Ortiz LE, Apostolopoulou E, Mejia N, Gamar-Elanbya MO, Jayatilleke K, de Lourdes-Duenas M, Aguirre-Avalos G, International Nosocomial Infection Control C (2014) International Nosocomial Infection Control Consortium (INICC) report, data summary of 43 countries for 2007–2012. Device-associated module. Am J Infect Control 42:942–956
Centers for Disease Control and Prevention (CDC)/National Healthcare Safety Network (NHSN) (2017) https://www.cdc.gov/nhsn/pdfs/pscmanual/4psc_clabscurrent.pdf. Accessed 6 Dec 2017
Mannien J, van den Hof S, Muilwijk J, van den Broek PJ, van Benthem B, Wille JC (2008) Trends in the incidence of surgical site infection in the Netherlands. Infect Control Hosp Epidemiol 29:1132–1138
Zuschneid I, Schwab F, Geffers C, Ruden H, Gastmeier P (2003) Reducing central venous catheter-associated primary bloodstream infections in intensive care units is possible: data from the German nosocomial infection surveillance system. Infect Control Hosp Epidemiol 24:501–505
Almirante B, Limon E, Freixas N, Gudiol F, Program V (2012) Laboratory-based surveillance of hospital-acquired catheter-related bloodstream infections in Catalonia Results of the VINCat Program (2007–2010). Enferm Infecc Microbiol Clin 30(Suppl 3):13–19
Bion J, Richardson A, Hibbert P, Beer J, Abrusci T, McCutcheon M, Cassidy J, Eddleston J, Gunning K, Bellingan G, Patten M, Harrison D, Matching Michigan C, Writing C (2013) ‘Matching Michigan’: a 2-year stepped interventional programme to minimise central venous catheter-blood stream infections in intensive care units in England. BMJ Qual Saf 22:110–123
Dixon-Woods M, Leslie M, Tarrant C, Bion J (2013) Explaining Matching Michigan: an ethnographic study of a patient safety program. Implement Sci 8:70
Beggs CB, Shepherd SJ, Kerr KG (2008) Increasing the frequency of hand washing by healthcare workers does not lead to commensurate reductions in staphylococcal infection in a hospital ward. BMC Infect Dis 8:114
Nicolau DV Jr, Kith G, Oshmyansky A (2010) Evidence for a simple linear relationship between MRSA rates and hand-washing compliance. J Hosp Infect 75:140–141
Wang J, Wang L, Magal P, Wang Y, Zhuo J, Lu X, Ruan S (2011) Modelling the transmission dynamics of meticillin-resistant Staphylococcus aureus in Beijing Tongren hospital. J Hosp Infect 79:302–308
Srigley JA, Furness CD, Baker GR, Gardam M (2014) Quantification of the Hawthorne effect in hand hygiene compliance monitoring using an electronic monitoring system: a retrospective cohort study. BMJ Qual Saf 23:974–980
Pronovost PJ, Goeschel CA, Colantuoni E, Watson S, Lubomski LH, Berenholtz SM, Thompson DA, Sinopoli DJ, Cosgrove S, Sexton JB, Marsteller JA, Hyzy RC, Welsh R, Posa P, Schumacher K, Needham D (2010) Sustaining reductions in catheter related bloodstream infections in Michigan intensive care units: observational study. BMJ 340:c309
Acknowledgements
We thank Sylvie Touveneau, Marie-Noëlle Chraïti and Benedetta Allegranzi, who devoted themselves to the training of the on-site investigators and study nurses in the workshops, both at the University Medical Center Groningen and the HUG. We thank Lauren Clack for editing. Our gratitude extends also to the participating centres for collaborating in this study, especially the on-site investigators and study nurses, physicians, (auxiliary) nurses and other healthcare professionals that responded positively to the challenge to improve their hand hygiene and CVC insertion practices and thus contributed to the increased safety of the patients in their care. Martin Wolkewitz has been funded by the German Research Foundation (Deutsche Forschungsgemeinschaft; Grant No WO 1746/1-1).
PROHIBIT Consortium: PROHIBIT Study Group: Pittet D (principaI investigator), Zingg W (coordinator), Ahmad R, Allegranzi B, Cookson B, Dettenkofer M, Gastmeier P, Grundmann H, Hansen S, Heczko PB, Holmes A, Kyratsis Y, Magiorakos A, Martin M, Richet H, Sax H, Szilágyi E, van Benthem B, van der Kooi T, Wu AW.
Author information
Authors and Affiliations
Consortia
Contributions
DP, HG, AW, WZ and HS conceived the study. HG, WZ, HS, BB and TK further designed the study and developed the study protocol. BW, LC and VC trained the on-site investigators and study nurses. ME, AB, KL, MPM, OP, MP, ES, TW, SF, AR, UD, PS, MZ, CG and TL were responsible for the local study coordination, data collection and implementation of the interventions. TK was responsible for random allocation of interventions to hospitals, data management and, together with MW, SH, JK and HB, for statistical analyses. TK and WZ wrote the initial draft of the manuscript, with contributions of HS, HG, JD, and LC, which was revised and approved by all authors. The guarantor is TK.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no interests to disclose.
Data sharing
The data are stored with the RIVM. Applications to use the data for further research can be sent to Dr. Walter Zingg (e-mail, Walter.Zingg@hcuge.ch).
Additional information
Hajo Grundmann and Walter Zingg contributed equally to this work.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
van der Kooi, T., Sax, H., Pittet, D. et al. Prevention of hospital infections by intervention and training (PROHIBIT): results of a pan-European cluster-randomized multicentre study to reduce central venous catheter-related bloodstream infections. Intensive Care Med 44, 48–60 (2018). https://doi.org/10.1007/s00134-017-5007-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-017-5007-6