Abstract
Purpose
Guidelines recommend teaching of lung ultrasound for critical care, though little information exists on how much training is required for independent practice, especially for non-physician trainees. We thus aimed to elucidate a threshold number of cases above which competency for independent practice may be attained for respiratory therapists (RTs).
Methods
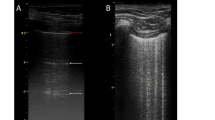
We conducted a prospective audit of lung ultrasound training between July 2014 and April 2015 in our 20-bed medical intensive care unit. Following theoretical instruction and self-learning, trainees acquired images from 12 lung zones under direct supervision and classified images into six patterns. Assistance during image acquisition and correct interpretation of ultrasound images were recorded.
Results
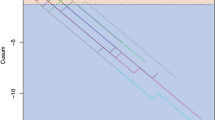
Eleven ultrasound-naïve RTs scanned an average of 15 patients each (170 patients in total). Among supervisor-adjudicated lung ultrasound findings, 35.5 % were abnormal. Blinded verification of the adjudicated findings was done for the first 92 patients (1104 images), with an agreement of 95.4 %. As RTs scanned more patients, there was a significant decrease in the proportion of images requiring supervisor assistance (Cuzick’s P < 0.001), and a significant increase in the proportion of correctly identified images (Cuzick’s P = 0.008). After trainees performed at least ten scans, less than 2 % of images required assistance with acquisition and less than 5 % were wrongly interpreted.
Conclusions
Our training method allowed RTs to independently perform lung ultrasound after at least ten directly supervised scans. Given that RTs are likely to have less ultrasound knowledge and less clinical know-how compared to physicians, we believe that the same threshold number of scans may be also safely applied to the latter.


Similar content being viewed by others
References
Xirouchaki N, Kondili E, Prinianakis G, Malliotakis P, Georgopoulos D (2014) Impact of lung ultrasound on clinical decision making in critically ill patients. Intensive Care Med 40:57–65
Havelock T, Teoh R, Laws D, Gleeson F, British Thoracic Society Pleural Disease Guideline Group (2010) Pleural procedures and thoracic ultrasound: British Thoracic Society pleural disease guideline 2010. Thorax 65(Suppl 2):ii61–ii76
Sim SS, Lien WC, Chou HC, Chong KM, Liu SH, Wang CH, Chen SY, Hsu CY, Yen ZS, Chang WT, Huang CH, Ma MH, Chen SC (2012) Ultrasonographic lung sliding sign in confirming proper endotracheal intubation during emergency intubation. Resuscitation 83:307–312
Soummer A, Perbet S, Brisson H, Arbelot C, Constantin JM, Lu Q, Rouby JJ, Lung Ultrasound Study Group (2012) Ultrasound assessment of lung aeration loss during a successful weaning trial predicts postextubation distress. Crit Care Med 40:2064–2072
Lichtenstein DA (2015) BLUE-protocol and FALLS-protocol: two applications of lung ultrasound in the critically ill. Chest 147:1659–1670
Volpicelli G, Skurzak S, Boero E, Carpinteri G, Tengattini M, Stefanone V, Luberto L, Anile A, Cerutti E, Radeschi G, Frascisco MF (2014) Lung ultrasound predicts well extravascular lung water but is of limited usefulness in the prediction of wedge pressure. Anesthesiology 121:320–327
Bouhemad B, Brisson H, Le-Guen M, Arbelot C, Lu Q, Rouby JJ (2011) Bedside ultrasound assessment of positive end-expiratory pressure-induced lung recruitment. Am J Respir Crit Care Med 183:341–347
Via G, Storti E, Gulati G, Neri L, Mojoli F, Braschi A (2012) Lung ultrasound in the ICU: from diagnostic instrument to respiratory monitoring tool. Minerva Anestesiol 78:1282–1296
See KC, Ong V, Ng J, Tan RA, Phua J (2014) Basic critical care echocardiography by pulmonary fellows: learning trajectory and prognostic impact using a minimally resourced training model. Crit Care Med 42:2169–2177
Neri L, Storti E, Lichtenstein D (2007) Toward an ultrasound curriculum for critical care medicine. Crit Care Med 35:S290–S304
Cholley BP, Mayo PH, Poelaert J, Vieillard-Baron A, Vignon P, Alhamid S, Balik M, Beaulieu Y, Breitkreutz R, Canivet JL, Doelken P, Flaatten H, Frankel H, Haney M, Hilton A, Maury E, McDermid RC, McLean AS, Mendes C, Pinsky MR, Price S, Schmidlin D, Slama M, Talmor D, Teles JM, Via G, Voga G, Wouters P, Yamamoto T, Expert Round Table on Ultrasound in ICU (2011) International expert statement on training standards for critical care ultrasonography. Intensive Care Med 37:1077–1083
Volpicelli G, Elbarbary M, Blaivas M, Lichtenstein DA, Mathis G, Kirkpatrick AW, Melniker L, Gargani L, Noble VE, Via G, Dean A, Tsung JW, Soldati G, Copetti R, Bouhemad B, Reissig A, Agricola E, Rouby JJ, Arbelot C, Liteplo A, Sargsyan A, Silva F, Hoppmann R, Breitkreutz R, Seibel A, Neri L, Storti E, Petrovic T, International Liaison Committee on Lung Ultrasound for International Consensus Conference on Lung Ultrasound (2012) International evidence-based recommendations for point-of-care lung ultrasound. Intensive Care Med 38:577–591
Alexandrou E, Spencer TR, Frost SA, Mifflin N, Davidson PM, Hillman KM (2014) Central venous catheter placement by advanced practice nurses demonstrates low procedural complication and infection rates—a report from 13 years of service. Crit Care Med 42:536–543
Royal College of Radiologists (2012) Ultrasound training recommendations for medical and surgical specialities. RCR, London
Ambrose SA (2010) How learning works: seven research-based principles for smart teaching. Jossey-Bass, San Francisco
See KC, Ong V, Teoh CM, Ooi OC, Widjaja LS, Mujumdar S, Phua J, Khoo KL, Lee P, Lim TK (2014) Bedside pleural procedures by pulmonologists and non-pulmonologists: a 3-year safety audit. Respirology 19:396–402
Larsen DP, Butler AC, Roediger HL 3rd (2008) Test-enhanced learning in medical education. Med Educ 42:959–966
Lichtenstein DA (2014) Lung ultrasound in the critically ill. Ann Intensive Care 4:1
Lichtenstein DA, Meziere GA (2008) Relevance of lung ultrasound in the diagnosis of acute respiratory failure: the BLUE protocol. Chest 134:117–125
Lichtenstein D, Meziere GA (2011) The BLUE-points: three standardized points used in the BLUE-protocol for ultrasound assessment of the lung in acute respiratory failure. Crit Ultrasound J 3:109–110
Cuzick J (1985) A Wilcoxon-type test for trend. Stat Med 4:87–90
Volpicelli G, Boero E, Sverzellati N, Cardinale L, Busso M, Boccuzzi F, Tullio M, Lamorte A, Stefanone V, Ferrari G, Veltri A, Frascisco MF (2014) Semi-quantification of pneumothorax volume by lung ultrasound. Intensive Care Med 40:1460–1467
Leblanc D, Bouvet C, Degiovanni F, Nedelcu C, Bouhours G, Rineau E, Ridereau-Zins C, Beydon L, Lasocki S (2014) Early lung ultrasonography predicts the occurrence of acute respiratory distress syndrome in blunt trauma patients. Intensive Care Med 40:1468–1474
Mayo PH, Beaulieu Y, Doelken P, Feller-Kopman D, Harrod C, Kaplan A, Oropello J, Vieillard-Baron A, Axler O, Lichtenstein D, Maury E, Slama M, Vignon P (2009) American College of Chest Physicians/La Societe de Reanimation de Langue Francaise statement on competence in critical care ultrasonography. Chest 135:1050–1060
Ericsson KA (2004) Deliberate practice and the acquisition and maintenance of expert performance in medicine and related domains. Acad Med 79:S70–S81
Patel R, Sandars J, Carr S (2015) Clinical diagnostic decision-making in real life contexts: a trans-theoretical approach for teaching: AMEE Guide No. 95. Med Teach 37:211–227
Spencer J (2003) Learning and teaching in the clinical environment. BMJ 326:591–594
Acknowledgments
All the authors jointly conceived the study and prepared the manuscript. Dr. See, Ms. Wong, Mr. Leanda, Ms. Santos, and Mr. Taculod organized and implemented the training curriculum. Ms. Ong, and Ms. Wong performed the data extraction. Dr. See performed the data analysis. Dr. Phua and Dr. Teoh supervised the analysis and edited the article. Dr. See had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors have disclosed that they do not have any potential conflicts of interest.
Additional information
This work was performed at the National University Health System, Singapore.
Take-home message: Ultrasound-naïve respiratory therapists (RTs) can be readily trained to perform lung ultrasound independently and competently: low levels of assistance (less than 2 %) were required after six cases, while high levels of accuracy (greater than 95 %) can be attained with at least ten cases. This has important implications in guiding training curricula and processes: (1) Given that RTs are likely to have less ultrasound knowledge and less clinical know-how compared to physicians, our study results could be extrapolated to ultrasound-naïve physician-trainees; (2) RTs may help physicians perform lung ultrasound, potentially improving the array of ICU services without further burdening physicians.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
See, K.C., Ong, V., Wong, S.H. et al. Lung ultrasound training: curriculum implementation and learning trajectory among respiratory therapists. Intensive Care Med 42, 63–71 (2016). https://doi.org/10.1007/s00134-015-4102-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-015-4102-9