Abstract
Background
In severe sepsis, guidelines recommend de-escalating the empirical antimicrobial treatment as soon as the microbiological results are available. We aimed to determine the rate of de-escalation of the empirical antimicrobial treatment in neutropenic patients with severe sepsis. The characteristics of antimicrobial treatment associated with de-escalation and its impact on short- and long-term survival were also determined.
Methods
In the intensive care unit (ICU) of a cancer referral center, we prospectively collected observational data related to the antimicrobial management in neutropenic patients who developed severe sepsis and were admitted to ICU for at least 48 h. De-escalation of antimicrobial therapy consisted either of deleting one of the empirical antibiotics of a combined treatment, or, whenever possible, to use a betalactam antibiotic with a narrower spectrum of activity. Multivariate logistic regression was conducted to determine the factors associated with de-escalation, while a Cox proportional hazards model with a time-dependent covariate was fitted to assess the effect of de-escalation on 30-day survival. Finally 1-year survival after ICU discharge was compared across de-escalation groups.
Results
Cumulative incidence of de-escalation of the empirical antimicrobial treatment among the 101 patients of the cohort was 44 %, [95 % confidence interval (CI) 38–53 %], including 30 (68 %) patients with ongoing neutropenia. A microbiological documentation was available in 63 (63 %) patients. Factors associated with de-escalation were the adequation of the empirical antimicrobial treatment in ICU [OR = 10.8 (95 % CI 1.20–96)] for adequate documented treatment versus appropriate empirical treatment, the compliance with guidelines regarding the empirical choice of the anti-pseudomonal betalactam [OR = 10.8 (95 % CI 1.3–89.5)]. De-escalation did not significantly modify the hazard of death within the first 30 days [HR = 0.51 (95 % CI 0.20–1.33)], nor within 1 year after ICU discharge [HR = 1.06 (95 % CI 0.54–2.08)].
Conclusion
Our data suggest that, in ICU, de-escalation of the empirical antimicrobial treatment is frequently applied in neutropenic cancer patients with severe sepsis. No evidence of any prognostic impact of this de-escalation was found.

Similar content being viewed by others
References
Dellinger RP, Levy MM, Rhodes A et al (2013) Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock, 2012. Intensive Care Med 39:165–228
Kollef MH, Micek ST (2005) Strategies to prevent antimicrobial resistance in the intensive care unit. Crit Care Med 33:1845–1853
Shorr AF (2009) Review of studies of the impact on Gram-negative bacterial resistance on outcomes in the intensive care unit. Crit Care Med 37:1463–1469
Leone M, Bourgoin A, Cambon S, Dubuc M, Albanese J, Martin C (2003) Empirical antimicrobial therapy of septic shock patients: adequacy and impact on the outcome. Crit Care Med 31:462–467
Leone M, Garcin F, Bouvenot J et al (2007) Ventilator-associated pneumonia: breaking the vicious circle of antibiotic overuse. Crit Care Med 35:379–385
Rello J, Vidaur L, Sandiumenge A et al (2004) De-escalation therapy in ventilator-associated pneumonia. Crit Care Med 32:2183–2190
Heenen S, Jacobs F, Vincent JL (2012) Antibiotic strategies in severe nosocomial sepsis: why do we not de-escalate more often? Crit Care Med 40:1404–1409
Talpaz M, Shah NP, Kantarjian H et al (2006) Dasatinib in imatinib-resistant Philadelphia chromosome-positive leukemias. N Engl J Med 354:2531–2541
Vanneman M, Dranoff G (2012) Combining immunotherapy and targeted therapies in cancer treatment. Nat Rev Cancer 12:237–251
Song JU, Suh GY, Park HY et al (2012) Early intervention on the outcomes in critically ill cancer patients admitted to intensive care units. Intensive Care Med 38:1505–1513
Legrand M, Max A, Schlemmer B, Azoulay E, Gachot B (2011) The strategy of antibiotic use in critically ill neutropenic patients. Ann Intensive Care 1:22
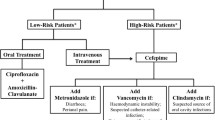
Freifeld AG, Bow EJ, Sepkowitz KA et al (2011) Clinical practice guideline for the use of antimicrobial agents in neutropenic patients with cancer: 2010 update by the infectious diseases society of America. Clin Infect Dis 52:427–431
American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference (1992) Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Crit Care Med 20:864–874
Bernard GR, Artigas A, Brigham KL et al (1994) The American-European consensus conference on ARDS. Definitions, mechanisms, relevant outcomes, and clinical trial coordination. Am J Respir Crit Care Med 149:818–824
Knaus WA, Draper EA, Wagner DP, Zimmerman JE (1985) Prognosis in acute organ-system failure. Ann Surg 202:685–693
Le Gall JR, Lemeshow S, Saulnier F (1993) A new simplified acute physiology score (SAPS II) based on a European/north American multicenter study. JAMA 270:2957–2963
Vincent JL, de Mendonça A, Cantraine F et al (1998) Use of the SOFA score to assess the incidence of organ dysfunction/failure in intensive care units: results of a multicenter, prospective study. Working group on “sepsis-related problems” of the European Society of Intensive Care Medicine. Crit Care Med 26:1793–1800
Azoulay E, Mokart D, Lambert J et al (2010) Diagnostic strategy for hematology and oncology patients with acute respiratory failure: randomized controlled trial. Am J Respir Crit Care Med 182:1038–1046
Azoulay E, Schlemmer B (2006) Diagnostic strategy in cancer patients with acute respiratory failure. Intensive Care Med 32:808–822
Meunier F, Lukan C (2008) The first European conference on infections in leukaemia—ECIL1: a current perspective. Eur J Cancer 44:2112–2117
Buchheidt D, Bohme A, Cornely OA et al (2003) Diagnosis and treatment of documented infections in neutropenic patients–recommendations of the infectious diseases working party (AGIHO) of the German society of hematology and oncology (DGHO). Ann Hematol 82(Suppl 2):S127–S132
Harbarth S, Garbino J, Pugin J, Romand JA, Lew D, Pittet D (2003) Inappropriate initial antimicrobial therapy and its effect on survival in a clinical trial of immunomodulating therapy for severe sepsis. Am J Med 115:529–535
Mikulska M, Akova M, Averbuch D, Klyasova G, Livemore D, Orasch C et al. 4th European Conference on Infections in Leukemia. http://www.ebmt.org/Contents/Resources/Library/ECIL/Documents/ECIL4%202011%20Bacterial%20resistance%20in%20Haematology.pdf. 14-2-2012
Trecarichi EM, Tumbarello M, Spanu T et al (2009) Incidence and clinical impact of extended-spectrum-beta-lactamase (ESBL) production and fluoroquinolone resistance in bloodstream infections caused by Escherichia coli in patients with hematological malignancies. J Infect 58:299–307
Tumbarello M, Spanu T, Sanguinetti M et al (2006) Bloodstream infections caused by extended-spectrum-beta-lactamase-producing Klebsiella pneumoniae: risk factors, molecular epidemiology, and clinical outcome. Antimicrob Agents Chemother 50:498–504
Safdar A, Rolston KV (2007) Stenotrophomonas maltophilia: changing spectrum of a serious bacterial pathogen in patients with cancer. Clin Infect Dis 45:1602–1609
Kollef MH (2006) Providing appropriate antimicrobial therapy in the intensive care unit: surveillance vs. de-escalation. Crit Care Med 34:903–905
Morel J, Casoetto J, Jospe R et al (2010) De-escalation as part of a global strategy of empiric antibiotherapy management. A retrospective study in a medico-surgical intensive care unit. Crit Care 14:R225
Karvunidis T, Chvojka J, Lysak D et al (2012) Septic shock and chemotherapy-induced cytopenia: effects on microcirculation. Intensive Care Med 38:1336–1344
Mokart D, van Craenenbroeck T, Lambert J et al (2012) Prognosis of acute respiratory distress syndrome in neutropenic cancer patients. Eur Respir J 40:169–176
Xu XJ, Tang YM, Liao C et al (2013) Inflammatory cytokine measurement quickly discriminates gram-negative from gram-positive bacteremia in pediatric hematology/oncology patients with septic shock. Intensive Care Med 39:319–326
Depuydt P, Benoit D, Vogelaers D et al (2006) Outcome in bacteremia associated with nosocomial pneumonia and the impact of pathogen prediction by tracheal surveillance cultures. Intensive Care Med 32:1773–1781
Azoulay E, Mokart D, Rabbat A et al (2008) Diagnostic bronchoscopy in hematology and oncology patients with acute respiratory failure: prospective multicenter data. Crit Care Med 36:100–107
Burghi G, Lemiale V, Seguin A et al (2011) Outcomes of mechanically ventilated hematology patients with invasive pulmonary aspergillosis. Intensive Care Med 37:1605–1612
Silva BN, Andriolo RB, Atallah AN, Salomao R (2013) De-escalation of antimicrobial treatment for adults with sepsis, severe sepsis or septic shock. Cochrane Database Syst Rev 3:CD007934
Acknowledgments
The study was funded by the Department of Anesthesiology and Critical Care of Paoli-Calmettes Institute.
Conflicts of interest
M. L. has received consultancy fees from LFB Biomédicaments and honoraria from Fresenius Kabi and Novartis for lectures. D. M., A. S., L. C. C., J. P. B., M. F., G. S., P. B., S. D., N. V.,C. S., and J. L. B. declare no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Mokart, D., Slehofer, G., Lambert, J. et al. De-escalation of antimicrobial treatment in neutropenic patients with severe sepsis: results from an observational study. Intensive Care Med 40, 41–49 (2014). https://doi.org/10.1007/s00134-013-3148-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-013-3148-9