Abstract
Purpose
To assess the time interval required to reach a new steady state of oxygenation-, ventilation-, respiratory mechanics- and hemodynamics-related variables after decreasing/increasing positive end expiratory pressure (PEEP).
Methods
In 23 patients (group 1) with acute respiratory distress syndrome (ARDS), PEEP was decreased from 10 to 5 cmH2O and, after 60′, it was increased from 5 to 15 cmH2O. In 21 other ARDS patients (group 2), PEEP was increased from 10 to 15 cmH2O and, after 60′, decreased from 15 to 5 cmH2O. Oxygenation, ventilation, respiratory mechanics and hemodynamic variables were recorded at time 5′, 15′, 30′ and 60′ after each PEEP change.
Results
When PEEP was decreased, PaO2, PaO2/FiO2, venous admixture and arterial oxygen saturation reached their equilibrium after 5′. In contrast, when PEEP was increased, the equilibrium was not reached even after 60′. The ventilation-related variables did not change significantly with PEEP. The respiratory system compliance, when PEEP was decreased, significantly worsened only after 60′. Hemodynamics did not change significantly with PEEP. In the individual patients the change of oxygenation-related variables and of respiratory system compliance observed after 5′ could predict the changes recorded after 60′. This was not possible for PaCO2.
Conclusions
We could not find a unique equilibration time for all the considered variables. However, in general, a decremental PEEP test requires far lower equilibrium time than an incremental PEEP test, suggesting a different time course for derecruitment and recruitment patterns.
Similar content being viewed by others
Introduction
Positive end expiratory pressure (PEEP) is frequently applied in Intensive Care, either to improve oxygenation [1] or to protect the lung [2, 3]. However the selection of the “optimum” PEEP level [4] for an individual patient is still an unresolved problem in clinical practice [5]. Incremental or decremental PEEP [6] tests are frequently performed to determine the best compromise between recruitment and over distension with tolerable hemodynamic changes. Therefore, the evaluation of changes following the increase and decrease in PEEP level is a frequent requirement in intensive care units (ICU). The equilibration time for oxygenation has been described after setting PEEP 2 cmH2O higher than inflection point of the pressure–volume curve [7]. The equilibration time for other oxygenation-related variables, respiratory system compliance and hemodynamics, during both incremental and decremental PEEP tests is not well established, although in clinical practice 20–30 min is allowed as “equilibration period.” Consequently, a considerably long time may be required if more than one level of PEEP is tested. In patients with acute respiratory distress syndrome (ARDS), we aimed to assess the equilibrium time required for the variables most commonly used in clinical practice, after both incremental or decremental PEEP test.
Materials and methods
Study population
The study was approved by the institutional review board of our hospital, and informed consent was obtained according to the Italian national regulations. Mechanically ventilated patients, fulfilling the diagnostic criteria of ARDS (American European Consensus Conference definition [8]), admitted to the intensive care unit of our institution, were enrolled in this study from January 2006 to April 2008. Exclusion criteria were age lower than 18 years, hemodynamic instability, documented barotrauma, pulmonary emphysema and pulmonary fibrosis.
Study protocol
All enrolled patients were sedated with propofol and midazolam and paralyzed with vecuronium to assure muscle relaxation. A recruitment maneuver was performed to normalize lung volumes just before beginning the study procedures: patients were ventilated for 2 min in pressure-controlled ventilation at an inspiratory plateau pressure of 45 cmH2O, a positive end expiratory pressure (PEEP) of 5 cmH2O, a respiratory rate (RR) of ten breaths per minute and a 1:1 ratio of inspiration to expiration (I:E). Thereafter patients were ventilated for 60′ with a PEEP level of 10 cmH2O and tidal volume (Vt) of 6–8 ml per kilogram of actual body weight with an I:E ratio of 1:1. During this period, the inspired oxygen fraction (FiO2) was adjusted to maintain arterial saturation between 90 and 100 %, and the RR was adjusted to maintain arterial partial pressure of carbon dioxide (PaCO2) between 35 and 50 mmHg. After this period, the ventilatory setting (FiO2, minute ventilation, I:E ratio, Vt, RR) was maintained unchanged throughout the study, while the PEEP was increased or decreased according to the protocol.
Forty-four patients were randomized into two groups. In the 23 patients in group 1, PEEP changed from 10 to 5 cmH2O and afterwards from 5 to 15 cmH2O, while in the 21 patients in group 2, PEEP changed from 10 to 15 cmH2O and afterwards from 15 to 5 cmH2O. Each level of PEEP was maintained for 60′.
Measurements and data collection
Respiratory and hemodynamic parameters were recorded at time 0′, that is, before PEEP changes, and time 5′, 15′, 30′ and 60′ after each PEEP change. At each time we collected/computed the following variables (see Supplementary Appendix for details and computations).
Oxygen- related variables
These were arterial and central venous oxygen partial pressure (PaO2 and PvO2), PaO2/FiO2, arterial and central venous oxygen saturation (SaO2 and SvO2) and venous admixture.
Ventilation-related variables
PaCO2, the end tidal partial pressure of carbon dioxide (EtCO2) and expired CO2 in 1 min (PECO2) were measured by means of continuous expiratory air sampling (CO2SMO PLUS 8100; Novametrix Medical System Inc., Wallingford, CT). The physiologic and alveolar dead space fraction (Vd/Vt physiol. and Vd/Vt alveolar) were computed according to standard formulas.
Respiratory mechanics-related variables
Minute ventilation, peak pressure, inspiratory plateau pressure and mean airway pressure were recorded. Respiratory system compliance was also computed.
Hemodynamics-related variables
Heart rate, central venous pressure (CVP) and mean arterial pressure were recorded for every patient. Values of cardiac output were measured when the pulmonary catheter was in place (seven patients in group 1 and five patients in group 2).
Statistical analysis
Results are presented as mean ± standard deviation. Comparison of clinical variables, respiratory and physiological variables was performed by one-way or two-way analysis of variance on repeated measures or Student’s t test in the case of variables that were normally distributed and by one-way or two-way analysis of variance on repeated measures on ranks or the Wilcoxon test in the case of variables that did not appear normally distributed. The chi-square test was used in case of qualitative variables. When analysis of variance revealed a significant difference, Bonferroni’s t-test or Tukey’s test was used. Linear regression was used to assess the relationship between early and late changes of the considered variables. P < 0.05 was accepted as significant. Analysis was performed with SigmaPlot 11.0 (Systat Software, Inc.).
Results
The baseline characteristics of the study population are summarized in Table 1. The two groups did not show any differences in any of the variables except for the respiratory rate, which was slightly lower in group 2.
Decreasing PEEP
The effects of decreasing PEEP from 10 to 5 and from to 15 to 5 cmH2O on PaO2 (upper panel), PaCO2 (middle panel) and respiratory system compliance (lower panel) are shown in Fig. 1. For completeness, we reported the response of oxygenation- ventilation-, respiratory mechanics- and hemodynamics-related variables to PEEP decay at different times in the supplementary appendix, Table E1. As shown, we found that PaO2 values recorded from 5′ to 60′ are different from those recorded at time 0′, but we could not find any difference in values recorded from time 5′ to 60′ after decreasing PEEP. This indicates that, when PEEP is decreased, the equilibration time for arterial oxygenation is reached within 5′. PaO2/FiO2, venous admixture and arterial saturation similarly worsened at time 5′ and remained stable thereafter. In contrast, the PaCO2 significantly increased at time 30′ and 60′ after PEEP decrease. The EtCO2 significantly decreased in both groups at time 5′ and returned to the baseline level between time 15′ and 60′. Interestingly, however, physiological and alveolar dead space did not show any statistically significant change throughout the whole observation period.
Response of PaO2 (upper panel), PaCO2 (middle panel) and respiratory system compliance (Crs) (lower panel) to PEEP decay at different times. Black dots represent PEEP decay from 10 to 5 cmH2O; white dots represent PEEP decay from 15 to 5 cmH2O. P values resulting from one-way analysis of variance on repeated measures (on ranks when required): PEEP decay from 10 to 5 cmH2O, PaO2 P < 0.001, PaCO2 = 0.025, Crs P < 0.001; PEEP decay from 15 to 5 cmH2O, PaO2 P < 0.001, PaCO2 = 0.010, Crs P < 0.001. Symbols refer to post hoc analysis. *P < 0.05 vs. time 0′; # P < 0.05 vs. time 5′
According to respiratory system mechanics, the significant decrease in plateau pressure at time 5′ matched the decrease of PEEP as the respiratory system compliance was unmodified. At time 60′, however, plateau pressure increased and respiratory system compliance decreased significantly compared to time 5′. Concerning hemodynamics-related variables, no changes in mean arterial pressure and heart rate occurred from baseline to time 60′, while cardiac output increased significantly at time 30′ and time 60′ only when PEEP was decreased from 15 to 5 cmH2O. The central venous pressure significantly decreased at time 5′ and thereafter remained stable. The decrease of SvO2 was statistically significant at time 5′ when PEEP decreased from 10 to 5 cmH2O and matched the decrease of the SaO2. Thereafter, the SvO2 remained stable throughout the whole observation period.
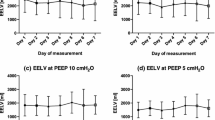
Increasing PEEP
The effects of increasing PEEP from 10 to 15 and from to 5 to 15 cmH2O on PaO2 (upper panel), PaCO2 (middle panel) and respiratory system compliance (lower panel) are shown in Fig. 2. For completeness, we reported the response of oxygenation- ventilation-, respiratory mechanics- and hemodynamics-related variables to PEEP increase at different times in the supplementary appendix, Table E2. As shown, the PaO2 values progressively increased from time 5′ to time 60′, and no equilibrium was reached within this 60-min interval, as indicated by the statistically significant difference between non-contiguous values. The venous admixture, after a significant improvement at time 5′, remained stable throughout the observation period, while arterial saturation and PaO2/FiO2 continuously increased with time as PaO2 did. Both PaCO2 and EtCO2 significantly decreased at time 5′ and, thereafter, returned to values equal to or significantly greater than baseline. Physiological and alveolar dead space did not change with PEEP increases and remained unmodified throughout the observation period.
Response of PaO2 (upper panel), PaCO2 (middle panel) and respiratory system compliance (Crs) (lower panel) to PEEP increases at different times. Black dots represent PEEP increase from 10 to 15 cmH2O; white dots represent PEEP increase from 5 to 15 cmH2O. P values resulting from one-way analysis of variance on repeated measures (on ranks when required): PEEP increase from 10 to 15 cmH2O, PaO2 P < 0.001, PaCO2 = 0.043, Crs P = 0.494; PEEP increase from 5 to 15 cmH2O, PaO2 P < 0.001, PaCO2 < 0.001, Crs P < 0.001. Symbols refer to post hoc analysis. *P < 0.05 vs. time 0′; # P < 0.05 vs. time 5′; °P < 0.05 vs. time 15′; § P < 0.05 vs. time 30′
The plateau pressure increased significantly at time 5′, matching the PEEP increase, the respiratory system compliance being unmodified. However, in the patients in whom PEEP increased from 5 to 15 cmH2O, the plateau pressure showed an increasing trend up to time 60′, but without reaching statistical significance. The respiratory system compliance showed a similar but opposite behavior. Mean arterial pressure, cardiac output and SvO2 were not affected by PEEP increase, and CVP significantly increased, while the heart rate remained stable.
Individual patient variability
Data reported in Tables E1 and E1 and in Figs. 1 and 2 are expressed as mean and standard deviation. The standard deviation values, however, showed great variability of the values recorded before and after the PEEP change in the study population. Therefore, for completeness, we reported the individual patient time courses of the analyzed variables in the online supplementary appendix (from page E9 to E39). As shown, the single patient behavior is consistent with the average values in the majority of cases.
Equilibration time and ARDS severity
When the response to incremental or decremental PEEP changes were examined after stratifying the patients into less and more severe ARDS according to the median FiO2 (median 50 % IQR 40–60), we could not find any difference in equilibration time in any of the considered variables. A detailed report of the time courses of the considered variables in patients with different ARDS severity is presented in the supplementary appendix.
Relationship between early and late response to PEEP change
In Fig. 3, upper panel, we represent the changes (indicated by the prefix “d”) between time 0′ and time 60′ of PaO2, respiratory system compliance and PaCO2 as a function of the changes of the same variables observed between time 0′ and time 5′. As shown, the relationship indicates that nearly 87 % of the late changes are explained by the early changes of PO2 [(dPaO2 from 0′ to 60′) = −9.58 + 1.13*(dPaO2 from 0′ to 5′), P < 0.001, r 2 = 0.87)]. In contrast, as shown in the middle panel, the changes in PaCO2 after 60′ are less predictable than its early changes [(dPaCO2 from 0′ to 60′) = −1.68 + 0.93*(dPaCO2 from 0′ to 5′), P < 0.001, r 2 = 0.37)]. In the lower panel, the late changes in respiratory mechanics appear well predicted by the early changes [(dCrs from 0′ to 60′) = 1.94 + 0.92*(dCrs from 0′ to 5′), P < 0.001, r 2 = 0.87)].
Relationship between changes (indicated by the prefix “d”) recorded at 5′ and changes recorded at 60′ of three variables representative of oxygenation (PaO2, first panel), ventilation (PaCO2, middle panel) and respiratory mechanics [respiratory system compliance (Crs), lower panel]. Black dots indicate PEEP decay from 10 to 5 cmH2O; black squares indicate PEEP increase from 10 to 15 cmH2O; white dots indicate PEEP increase from 5 to 15 cmH2O, and white squares indicate PEEP decay from 15 to 5 cmH2O. Solid lines represent the linear regression: (dPaO2 from 0′ to 60′) = −9.58 + 1.13*(dPaO2 from 0′ to 5′), P < 0.001, r 2 = 0.87 (dPaCO2 from 0′ to 60′) = −1.68 + 0.93*(dPaCO2 from 0′ to 5′), P < 0.001, r 2 = 0.37 (dCrs from 0′ to 60′) = 1.94 + 0.92*(dCrs from 0′ to 5′), P < 0.001, r 2 = 0.87
Discussion
It is a common practice in intensive care, before assessing the effects of changes of the ventilator setting on relevant variables, to wait for an “equilibration time.” As an example, it was found that after changing FiO2, the oxygenation reaches its equilibrium in <10′ [9, 10], while, when total ventilation is increased, the PaCO2 falls exponentially, reaching its equilibrium in 10–20′. In contrast, when ventilation is decreased, the rate of change of PaCO2 is far lower, and the equilibration time requires up to 45–60′ [11, 12]. The present study was designed to describe the equilibration time of oxygenation-, ventilation- and respiratory mechanics-related variables after incremental or decremental PEEP. We arbitrarily set the time 60′ as the longest time allowed for equilibration, assuming that a longer period could imply, in some patients, a dramatic change of the underlying pathophysiological conditions of the lung, which may confound the effects of PEEP alone. Tugrul et al. [7], after setting PEEP values according to the inflection point of the pressure volume curve, found 20′ sufficient to reach 90 % of the PaO2 recorded at time 60′, which was assumed as a “full equilibration time.” In contrast, in our study, we found that each group of variables reached its equilibrium at different times; moreover, we noted that some variables did not reach the equilibrium even at 60′. Finally, the time to equilibrium of the same variable was sometimes different when PEEP was decreased or increased, and, interestingly, the severity of ARDS, and, by inference, the lung recruitability, did not affect the equilibration time in any of the considered variables.
Oxygenation-related variables
When PEEP was decreased, the PO2 and the other oxygenation-related variables significantly decreased within 5′ and remained unmodified in the following 55′, suggesting that the oxygenation equilibrium was reached almost immediately. The PaO2 decrease is likely due to the immediate collapse of the most dependent lung regions, as observed by CT scan [13], which remain perfused. The initial collapse is primarily due to the gravity-dependent closure of the small airways (“loose” atelectasis). If the inspiratory pressure is sufficient to open them, an opening/closing phenomenon is generated [14]. With time the “loose” atelectasis may become “sticky” because of the gas reabsorption, and the opening pressure become greater [15]. This phenomenon may affect the lung mechanics but is probably irrelevant for oxygenation, which is impaired in the presence of either loose or sticky atelectasis, provided that atelectatic regions are perfused. It is also possible that, when atelectasis shifts from an opening/closing to always closed status, which should lead to a further deterioration of oxygenation, more blood flow is diverted to aerated regions, limiting the fall of PO2 (hypoxic vasoconstriction) [16, 17]. Independently from the causative mechanism, however, the PO2 values after 5′ are highly representative of the values observed up to 60′ (see Fig. 3).
In contrast, when PEEP was increased, the PO2 continuously rose, suggesting that equilibrium was not reached even at time 60′. In our setting, the PO2 increase was likely due to recruitment of previously collapsed and perfused pulmonary units, as FiO2, minute ventilation and hemodynamics were unchanged. The slow PaO2 increase confirms that, although most of the recruitment occurs rapidly, the remaining opening is a “slow” phenomenon [18]. In fact, recruitment depends on the interaction between the increase of opening pressure (the plateau pressure raised proportionally to the PEEP value) and the increased threshold for closing pressure (higher PEEP maintains open regions that would collapse at lower PEEP) [14, 19, 20]. Whatever the mechanism underlying the recruitment, it is obvious that its early assessment by observing PO2 variations during incremental PEEP may be misleading because of the slow equilibration time of the oxygenation-related variables. However, the PO2 values obtained after 5′, although not in equilibrium, may be sufficient to indicate the oxygenation trend (see Fig. 3).
Ventilation-related variables
When PEEP is decreased, we did not observe significant changes of PaCO2 throughout the observation period compared to basal values. To discuss the PaCO2 behavior, it is important to recall that the amount of CO2 in the body is very high (about 20-fold more than oxygen) and that it is distributed within fast (the blood) and intermediate and slow compartments (extracellular and intracellular). Due to this physiological characteristic, whatever the change in the fast compartment induced by changes of the ventilation/perfusion ratio, it is “buffered” with time by the re-equilibration between the fast compartment and the other body compartments. The practical consequence is that establishing the equilibrium of CO2 requires time [21].
When PEEP is increased, the lung volume increases and the alveolar PaCO2 (and EtCO2) immediately decreases, as we observed at time 5′. Afterwards, the PaCO2 returns to its baseline values. It must be noted, however, that an unmodified PaCO2 may reflect the coexistence of two opposite phenomena, a regional decrease of dead space due to recruitment of perfused units and the regional increase of dead space due to hyper-distention. It must be also noted, however, that the rate of the PaCO2 increase due to alveolar hypo-ventilation is far slower than its rate of decrease during hyper-ventilation [11, 12]. Moreover, we must also consider that changes of 1 or 2 mmHg of PaCO2, although physiologically important, are in the range of error of measurements of either the blood gas analyzer or capnography. All these facts account for the long “equilibration” time of PaCO2. Consequently late PaCO2 changes cannot be reliably predicted by its early changes, as indicated by the low coefficient of determination (see Fig. 3).
Respiratory mechanics-related variables
When PEEP was decreased, the respiratory system mechanics was unchanged at time 5′. However, with time, the respiratory system compliance tended to decrease, reaching statistical significance at time 60′. In this case, referring to an equilibration time may be inappropriate, as the changes of compliance likely reflect a progressive change of the underlying lung pathology. In fact, when PEEP is decreased, the pulmonary units, in which the superimposed pressure is higher than PEEP, will collapse. These units can reopen only if the lower plateau pressure (due to the lower PEEP) is still sufficient to overcome the opening pressures of the collapsed units. If so, these pulmonary units will undergo an intra-tidal opening/closing phenomenon. Initially, the respiratory system compliance is not affected, as plateau pressure and PEEP are, on average, equally decreased. With time, however, the regions undergoing opening and closing phenomena may undergo complete collapse due to gas reabsorption, and the inspiratory pressures are no longer sufficient to open these sticky atelectasis [15]. This time-dependent mechanism, leading to a decrease of the “baby lung” size, will result in a progressive decrease with time of respiratory system compliance, as we observed at time 60′.
When PEEP was increased from 10 to 15 cmH2O, we did not observe significant changes in respiratory system compliance. In this setting, as the oxygenation continuously increases with time, it is possible that the increase in respiratory system compliance associated with recruitment of new pulmonary units is offset by the hyper-inflation of other regions, as observed in animal models [20] or in CT studies [19]. When PEEP was increased from 5 to 15 cmH2O, the lung recruitment likely prevailed on the over-inflation, and at time 5′ and 15′ the respiratory system compliance increased significantly compared to the baseline. In summary, as the variations of compliance are likely associated with recruitment/derecruitment phenomena, not surprisingly they do not reach an immediate equilibrium.
Hemodynamics-related variables
Changes of PEEP are usually associated with a change of hemodynamics. In this series of patients, they were a minor entity, but, when occurring, they were immediately observed after 5′, as documented by the central venous pressure.
Conclusion
In our study, we could not find a unique equilibration time for the variables we studied. For oxygenation, the equilibrium was fast after decremental PEEP but unreachable after incremental PEEP. Ventilation-associated variables required a long time to reach their steady state because of the physiological characteristics of CO2 and its different patterns of elimination and retention. Modification of respiratory system mechanics required a long time and, the changes likely reflect a progressive modification of the underlying pulmonary pathology, rather than the achievement of a steady state. Therefore, the different dynamics of the considered variables should be taken into account when evaluating the effects of PEEP changes.
References
Falke KJ, Pontoppidan H, Kumar A, Leith DE, Geffin B, Laver MB (1972) Ventilation with end-expiratory pressure in acute lung disease. J Clin Invest 51:2315–2323
Webb HH, Tierney DF (1974) Experimental pulmonary edema due to intermittent positive pressure ventilation with high inflation pressures. Protection by positive end-expiratory pressure. Am Rev Respir Dis 110:556–565
Dreyfuss D, Saumon G (1998) Ventilator-induced lung injury: lessons from experimental studies. Am J Respir Crit Care Med 157:294–323
Suter PM, Fairley B, Isenberg MD (1975) Optimum end-expiratory airway pressure in patients with acute pulmonary failure. N Engl J Med 292:284–289
Gattinoni L, Caironi P (2008) Refining ventilatory treatment for acute lung injury and acute respiratory distress syndrome. Jama-Journal of the American Medical Association 299:691–693
Girgis K, Hamed H, Khater Y, Kacmarek RM (2006) A decremental PEEP trial identifies the PEEP level that maintains oxygenation after lung recruitment. Respir Care 51:1132–1139
Tugrul S, Cakar N, Akinci O, Ozcan PE, Disci R, Esen F, Telci L, Akpir K (2005) Time required for equilibration of arterial oxygen pressure after setting optimal positive end-expiratory pressure in acute respiratory distress syndrome. Crit Care Med 33:995–1000
Bernard GR, Artigas A, Brigham KL, Carlet J, Falke K, Hudson L, Lamy M, Legall JR, Morris A, Spragg R (1994) The American-European Consensus Conference on ARDS. Definitions, mechanisms, relevant outcomes, and clinical trial coordination. Am J Respir Crit Care Med 149:818–824
Sasse SA, Jaffe MB, Chen PA, Voelker KG, Mahutte CK (1995) Arterial oxygenation time after an Fi(02) increase in mechanically ventilated patients. Am J Respir Crit Care Med 152:148–152
Fildissis G, Katostaras T, Moles A, Katsaros A, Myrianthefs P, Brokalaki H, Tsoumakas K, Baltopoulos G (2010) Oxygenation equilibration time after alteration of inspired oxygen in critically ill patients. Heart Lung 39:147–152
Ivanov SD, Nunn JF (1968) Influence of duration of hyperventilation on rise time of P-CO2 after step reduction of ventilation. Respir Physiol 5:243–249
Ivanov SD, Nunn JF (1968) Methods of elevation of PCO2 after anaesthesia with passive hyperventilation. Br J Anaesth 40:804
Gattinoni L, D’Andrea L, Pelosi P, Vitale G, Pesenti A, Fumagalli R (1993) Regional effects and mechanism of positive end-expiratory pressure in early adult respiratory distress syndrome. JAMA 269:2122–2127
Gattinoni L, Pelosi P, Crotti S, Valenza F (1995) Effects of positive end-expiratory pressure on regional distribution of tidal volume and recruitment in adult respiratory distress syndrome. Am J Respir Crit Care Med 151:1807–1814
Pelosi P, Cadringher P, Bottino N, Panigada M, Carrieri F, Riva E, Lissoni A, Gattinoni L (1999) Sigh in acute respiratory distress syndrome. Am J Respir Crit Care Med 159:872–880
Cressoni M, Caironi P, Polli F, Carlesso E, Chiumello D, Cadringher P, Quintel M, Ranieri VM, Bugedo G, Gattinoni L (2008) Anatomical and functional intrapulmonary shunt in acute respiratory distress syndrome. Crit Care Med 36:669–675
Schuster DP, Anderson C, Kozlowski J, Lange N (2002) Regional pulmonary perfusion in patients with acute pulmonary edema. J Nucl Med 43:863–870
Albert SP, DiRocco J, Allen GB, Bates JHT, Lafollette R, Kubiak BD, Fischer J, Maroney S, Nieman GF (2009) The role of time and pressure on alveolar recruitment. J Appl Physiol 106:757–765
Crotti S, Mascheroni D, Caironi P, Pelosi P, Ronzoni G, Mondino M, Marini JJ, Gattinoni L (2001) Recruitment and derecruitment during acute respiratory failure: a clinical study. Am J Respir Crit Care Med 164:131–140
Pelosi P, Goldner M, McKibben A, Adams A, Eccher G, Caironi P, Losappio S, Gattinoni L, Marini JJ (2001) Recruitment and derecruitment during acute respiratory failure: an experimental study. Am J Respir Crit Care Med 164:122–130
Nunn JF (1993) Carbon dioxide. Nunn’s applied respiratory physiology, 4th edn. Butterworth-Heinemann, Oxford, pp 219–246
Conflicts of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
ClinicalTrials.gov Identifier: NCT00284102.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Chiumello, D., Coppola, S., Froio, S. et al. Time to reach a new steady state after changes of positive end expiratory pressure. Intensive Care Med 39, 1377–1385 (2013). https://doi.org/10.1007/s00134-013-2969-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-013-2969-x