Abstract
Purpose
Although low doses of oxygen (FiO2 <0.50) are considered nontoxic, recent studies have shown that even lower doses increase pulmonary inflammatory mediators. We aimed to evaluate the acute effects of reducing FiO2 on pulmonary inflammation in mechanically ventilated patients without respiratory failure.
Methods
This study was a prospective, single-center crossover study in a medical/surgical intensive care unit at a university hospital. Hemodynamically stable patients under mechanical ventilation for >24 h without severe respiratory failure (PaO2/FiO2 >250). A basal FiO2 of 0.40 was reduced to 0.21 provided SpO2 remained higher than 90 %. Patients who could not tolerate the reduction in FiO2 to 0.21 were excluded.
Results
We screened 40 patients, but only 28 (70 %) tolerated FiO2 0.21. We measured common clinical variables and inflammatory mediators in plasma and in exhaled breath condensate (EBC) at the end of three 4-h periods: (1) basal (FiO2 0.40), (2) after FiO2 reduction to 0.21, and (3) after returning FiO2 0.40. We used one-way ANOVA for repeated measurements with FiO2 as the grouping variable. Median values of inflammatory mediators in EBC showed nonsignificant changes among the three periods: NO2 + NO3 17.1, 14.1 and 11.0 μmol/L (p = 0.2), and 8-isoprostane 4.4, 8.2 and 5.3 pg/ml (p = 0.6) for the three periods, respectively. Plasma levels also showed nonsignificant changes during the period of the study: NO2 + NO3 12.6, 16.3 and 15.0 μmol/L (p = 0.9), TNFα 13.5, 18.0 and 14.5 pg/ml (p = 0.8), IL-4 12.9, 18.7 and 23.9 pg/ml (p = 0.1), IL-6 50.9, 35.1 and 28.3 pg/ml (p = 0.6), and IL-10 15.2, 22.2 and 22.2 pg/ml (p = 0.7) for the three periods, respectively.
Conclusion
FiO2 0.40 in mechanically ventilated patients without severe respiratory failure did not increase systemic or pulmonary inflammation.
Similar content being viewed by others
Introduction
Exposure to hyperoxia has long been recognized as a potential cause of acute lung injury. Prolonged hyperoxia in animal models causes histopathological changes similar to those seen in the acute respiratory distress syndrome (ARDS) and in models of ventilator-induced lung injury, including high-permeability edema, hyaline membrane formation, pulmonary vascular lesions, and eventual pulmonary fibrosis [1]. It is assumed that lung damage caused by hyperoxia is mediated by excess production of reactive oxygen intermediates either through direct damage to tissue constituents or via altered oxidative signaling [1].
Mechanical ventilation in patients without respiratory failure routinely includes low-dose oxygen up to 40 % [2, 3] with the rationale that it increases protection against critical incidents [4]; however, nowadays, pulse oximetry probably provides sufficient warning of these incidents. Although additional oxygen might reduce postsurgical infections [5, 6], resuscitation models have shown deleterious effects of additional oxygen in animals [7] and in humans [8]. Additional oxygen is also associated with worse outcome in patients with mild-to-moderate stroke [9].
Substantial scientific evidence now indicates that supplementary oxygen leading to hyperoxia has potential risks across a wide range of clinical scenarios. Many mechanisms have been proposed to account for the detrimental outcomes associated with excessive oxygen supplementation, including a reduction in cardiac output and coronary blood flow, an increase in systemic vascular resistance and blood pressure, a reduction in cerebral blood flow, increased atelectasis and intrapulmonary shunting, and production of toxic reactive oxygen species. In addition, oxygen therapy can delay clinical recognition of deteriorating respiratory function [10]. Although low doses of oxygen are considered safe [2], a recent report suggests that even minimal doses (FiO2 0.28) increase pulmonary inflammatory mediators in patients with chronic obstructive pulmonary disease (COPD) and in healthy volunteers [11].
We hypothesized that the inflammatory process caused by the low-dose oxygen routinely administered in the ICU could lead to changes in the redox state at the airway surface that may be characterized by an increase in the concentration of oxidants in exhaled breath condensate (EBC) samples. Thus, we evaluated the acute effect of reducing FiO2 from basal 0.40 to 0.21 on pulmonary inflammatory mediators in mechanically ventilated patients without severe respiratory failure.
Materials and methods
We prospectively screened all patients admitted to our medical/surgical ICU undergoing mechanical ventilation. The institutional Ethics Committee approved the study and patients’ next of kin provided written informed consent.
The inclusion criteria were: (1) age >18 years, (2) mechanical ventilation longer than 24 h, and (3) mild or absent respiratory failure defined as PaO2/FiO2 >250. Exclusion criteria were: (1) hemodynamic instability, defined as the need for increases or decreases in vasoactive drugs and/or severe arrhythmias, (2) symptomatic myocardial ischemia, or (3) severe neurocritical illness.
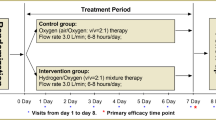
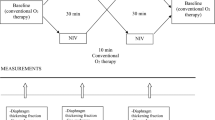
The study period of 12 h was divided in three 4-h periods: (1) basal (FiO2 0.40), (2) after FiO2 reduction to 0.21, provided SpO2 >90 %, and (3) after return to basal FiO2 0.40. Variables were recorded at the end of each period. Clinical variables were heart rate, arterial blood pressure, SpO2, and body temperature. Pulmonary variables were respiratory rate, peak airway pressure, plateau pressure, whereas positive end-expiratory pressure (PEEP) and ventilatory mode remained unchanged during the 12-h period. Blood gases were obtained from indwelling arterial catheters and central venous catheters. Blood samples were also obtained for determination of plasma inflammatory mediators (NO2, NO3, TNFα, IL-4, IL-6, and IL-10). The experiment was aborted at any point if pulse oximetry saturation dropped below 90 % or if severe hemodynamic instability or another emergency (self-extubation, barotrauma, shock) occurred.
During the last 20 min of each period, EBC was collected using an EcoScreen (Jaeger, Wurzburg, Germany) system attached to the expiratory port of the Y-piece. This device collects and freezes the EBC at a median rate of 0.07 ml/min. The samples were stored at −70 °C until final laboratory determination of inflammatory mediators (NO2, NO3, and 8-isoprostane) in a single session.
Interleukins (IL-4, IL-6 and IL-10) and TNFα plasma protein levels were determined using a human multiplex immunoassay kit (MPXHCYTO-60K Milliplex MAP human cytokine panel; Millipore Corporation, Billerica, MA) using a high-throughput multiplex system (Luminex 200; Luminex, Austin, TX). Only the linear portions of the standard curves were used to quantify cytokine concentrations, and in instances where the fluorescence reading exceeded the linear range of the standard curve, the sample was appropriately diluted to ensure that the concentration was in the linear portion of the curve. The assay sensitivities were 0.6 pg/ml for IL-4, 0.3 pg/ml for IL-6, and 0.1 pg/ml for IL-10 and TNFα.
The nitrate/nitrite concentration in EBC samples was determined using a colorimetric assay based on the Griess reaction in which sample duplicates were reacted with Griess reagent (Cayman Chemical, Ann Arbor, MI) and were measured at 540 nm absorbance in a microplate reader. The assay sensitivity was 1 μM/L for nitrite and 2.5 μM/L for nitrate. The EBC 8-isoprostane concentration was determined using a commercially available specific enzyme immunoassay kit (Cayman Chemical, Ann Arbor, MI). The assay sensitivity was 4 pg/ml.
Statistical analysis
In order to target a 30 % reduction in the level of inflammatory mediators with an alpha error of 0.05 and a statistical power of 80 %, the required sample was calculated as 24 patients. We recruited 28 patients to allow for possible losses. Due to the low number of cases, quantitative variables are expressed as medians and interquartile ranges (IQR). One-way ANOVA for repeated measurements with FiO2 as the grouping variable was performed for each variable. Statistical significance was defined as p < 0.05.
Results
We screened 40 patients, but only 28 (70 %) tolerated FiO2 0.21. Table 1 shows the clinical characteristics of the patients included. Patients were studied after a median of 3 days on mechanical ventilation; 80 % were ventilated in assist-control mode and most received low PEEP.
No significant mean changes in heart rate or arterial blood pressure were observed during the study. As expected, exposure to FiO2 0.21 resulted in decreases in PaO2, SaO2, PvO2 and SvO2 (Table 2).
Median (IQR) values of inflammatory mediators in EBC showed nonsignificant changes between the 3 periods (Fig. 1). A nonsignificant trend to a progressive reduction was seen in NO2 + NO3: 17.1 μmol/L (8.5–44.3 μmol/L), 14.1 μmol/L (8.1–33.4 μmol/L) and 11.0 μmol/L (6.5–19.0 μmol/L), respectively (p = 0.2). In contrast, 8-isoprostane showed random variation: 4.4 μmol/L (3.0–9.6 μmol/L), 8.2 μmol/L (4.6–10.7 μmol/L) and 5.3 μmol/L (4.3–8.8 pg/ml), respectively (p = 0.6).
Inflammatory mediators in plasma also showed nonsignificant changes between the three periods: NO2+NO3 12.6 μmol/L (9.3–19.9 μmol/L), 16.3 μmol/L (10.0–20.7 μmol/L) and 15.0 μmol/L (10.8–23.0 μmol/L), respectively (p = 0.9); TNFα 13.5, 18.0 and 14.5 pg/ml (p = 0.8), respectively; IL-4 12.9, 18.7 and 23.9 pg/ml (p = 0.1), respectively; IL-6 50.9, 35.1 and 28.3 pg/ml (p = 0.6), respectively; and IL-10 15.2, 22.2 and 22.2 pg/ml (p = 0.7), respectively (Fig. 2).
Discussion
Our study failed to prove that FiO2 0.40 commonly administered to mechanically ventilated patients without respiratory failure induced any significant inflammatory effects on the lungs.
Pulmonary oxygen toxicity has been demonstrated in a variety of laboratory animals. However, humans seem to be far less susceptible, probably because humans have better defenses against free radicals [12]. Although the production of oxygen-derived free radicals is increased at high levels of PaO2, it seems that tissue defenses against free radicals are usually effective up to a tissue oxygen partial pressure (PO2) of about 450 mmHg [12], a value much higher than that normally obtained in the clinical setting. Moreover, there is compelling evidence that prolonged exposure to FiO2 of 100 % does not result in demonstrable pulmonary oxygen toxicity if the PaO2 is lower than 255 mmHg [12], supporting the hypothesis that oxygen toxicity is related to tissue PO2 rather than to FiO2. This partially explains why very few studies have demonstrated adverse effects of oxygen administration in patients. Some authors suggest that adverse effects of oxygen on the alveolar epithelium are rarely of practical importance in hypoxemic patients and that the lungs of patients with acute respiratory failure exhibit some relative resistance to prolonged oxygen exposure [13].
Jackson et al. [14] compared inflammatory mediators in EBC and bronchoalveolar lavage (BAL) fluid in 49 nonintubated patients, and concluded that EBC sampling cannot be compared directly with information derived from BAL. Although it is tempting to suggest that the discrepancy between EBC and BAL is attributable to the fact that different compartments of the lung are sampled, there are many other factors (volatility, solubility, electric charge, collection technique) that are likely to be involved that EBC biomarkers should probably be conceptualized totally differently from those of BAL, and separately for each individual marker [14]. Unlike BAL, EBC has the advantage that it does not require invasive instrumentation, induce any inflammatory change, or introduce foreign substances into the lung; furthermore, it can be performed repeatedly even in sicker patients.
In the last decade, Barnes has led a series of investigations exploring the usefulness of EBC in detecting subtle features of pulmonary inflammation. One exciting project comparing 23 healthy volunteers with 23 patients with COPD before and after breathing supplementary oxygen for 1 h found higher EBC levels of 8-isoprostane and IL-6 in the patients with COPD than in healthy subjects, but these markers increased homogeneously in both groups after exposure to oxygen [11]. Surprisingly, only 28 % oxygen was sufficient to bring about these increases. We found similar baseline values of 8-isoprostane in our patients; however, we observed no significant changes attributable to exposure to different oxygen concentrations. Moreover, although we used ultrasensitive assays, we were unable to detect any interleukins in our EBC samples at any time. One possible explanation for this difference is that we might have been more successful at avoiding airway contamination.
Romero et al. [15] measured inflammatory markers in EBC in normal individuals without respiratory disease, patients with multilobar pneumonia, patients with superinfected COPD, and mechanically ventilated patients with severe pneumonia. Only the last group had NO2 values similar to those found in our study, but NO3 values were much higher in our study. On the other hand, our 8-isoprostane levels were similar to those obtained by Romero et al. in patients without lung disease. Comparisons are difficult because EBC measurements are highly dependent on the device used for collecting and freezing the exhaled air, the sampling time, and the material of the storage tubes. Our EBC results for NO2, NO3 and 8-isoprostane are also similar to those reported by Cruz et al. [16] in healthy volunteers over a wide range of ages. Thus, our results should not be directly extrapolated to patients outside the specific design of our study, such as those with severe lung damage.
The levels of interleukins found in our patients were suggestive of a mild-to-moderate inflammatory state. In a study of patients with ARDS, Stüber et al. [17] found basal IL-6 and IL-10 levels five times higher than in our patients. These authors found that switching from protective lung ventilation to a nonprotective approach increased interleukin levels up to fourfold.
Our approach to reducing oxygen administration proved safe in terms of hemodynamics and oxygen supply. We found no signs of cardiac deterioration, either arrhythmias or ST changes, despite continuous monitoring. Additionally, very low venous oxygen saturation, a marker of possible tissue harm, was never reached. Classical physiology books suggest that additional oxygen administration increases arterial blood pressure; however, we found no significant relationship between these two factors in our patients. [12] (Figs. E1 and E2, Electronic supplementary material).
Limitations of the study
Although the mean values of clinical variables suggest a stable model, some lack of stability in the model may arise by random oscillations among critically ill patients, as shown by variability in individual arterial blood pressure during the study (Figs. E1 and E2, Electronic supplementary material). Another model-induced bias is the likelihood of a time-related continuous clinical improvement attributable to treatment during the 12-h study period, as suggested by the trend of decreasing proinflammatory interleukins (IL-6) with an associated trend of increasing antiinflammatory interleukins (IL-4 and IL-10) in plasma.
The length of the washout period may always be a limitation in this type of crossover study, but our 4-h interval has proven adequate for the inflammatory markers studied. Stüber et al. [17] demonstrated a reduction in plasma mediators after only 1 h; however, their BAL (not EBC) values actually increased after reducing the exposure to inflammation. In contrast, Caspersen et al. [18] demonstrated changes in healthy volunteers after only 90 min exposure to oxygen, and Modun et al. [19] found inflammatory effects after only 30 min exposure to 100 % oxygen.
Our sample size precludes us from ruling out the possibility that oxygen at this concentration may act differently in different populations. Nevertheless, we failed to find any hint of differences between patients with and without sepsis, or with and without trauma.
Conclusions
In our setting, the FiO2 0.40 commonly administered in mechanically ventilated patients without respiratory failure did not increase inflammation locally (in the lung) or systemically (in plasma).
References
Altemeier WA, Sinclair SE (2007) Hyperoxia in the intensive care unit: why more is not always better. Curr Opin Crit Care 13:73–78
de Graaff AE, Dongelmans DA, Binnekade JM, de Jonge E (2011) Clinicians’ response to hyperoxia in ventilated patients in a Dutch ICU depends on the level of FiO2. Intensive Care Med 37:46–51
de Jonge E, Peelen L, Keijzers PJ, Joore H, de Lange D, van der Voort PH, Bosman RJ, de Waal RA, Wesselink R, de Keizer NF (2008) Association between administered oxygen, arterial partial oxygen pressure and mortality in mechanically ventilated intensive care unit patients. Crit Care 12:R156
Pape A, Meier J, Kertscho H, Steche M, Laout M, Schwerdel F, Wedel M, Zwissler B, Habler O (2006) Hyperoxic ventilation increases the tolerance of acute normovolemic anemia in anesthetized pigs. Crit Care Med 34:1475–1482
Belda FJ, Aguilera L, de García la Asunción J, Alberti J, Vicente R, Ferrándiz L, Rodríguez R, Company R, Sessler DI, Aguilar G, Botello SG, Ortí R; Spanish Reduccion de la Tasa de Infeccion Quirurgica Group (2005) Supplemental perioperative oxygen and the risk of surgical wound infection: a randomized controlled trial. JAMA 294:2035–2042
Meyhoff CS, Wetterslev J, Jorgensen LN, Henneberg SW, Høgdall C, Lundvall L, Svendsen PE, Mollerup H, Lunn TH, Simonsen I, Martinsen KR, Pulawska T, Bundgaard L, Bugge L, Hansen EG, Riber C, Gocht-Jensen P, Walker LR, Bendtsen A, Johansson G, Skovgaard N, Heltø K, Poukinski A, Korshin A, Walli A, Bulut M, Carlsson PS, Rodt SA, Lundbech LB, Rask H, Buch N, Perdawid SK, Reza J, Jensen KV, Carlsen CG, Jensen FS, Rasmussen LS; PROXI Trial Group (2009) Effect of high perioperative oxygen fraction on surgical site infection and pulmonary complications after abdominal surgery: the PROXI randomized clinical trial. JAMA 302:1543–1550
Barth E, Bassi G, Maybauer DM, Simon F, Gröger M, Oter S, Speit G, Nguyen CD, Hasel C, Möller P, Wachter U, Vogt JA, Matejovic M, Radermacher P, Calzia E (2008) Effects of ventilation with 100 % oxygen during early hyperdynamic porcine fecal peritonitis. Crit Care Med 36:495–503
Kilgannon JH, Jones AE, Shapiro NI, Angelos MG, Milcarek B, Hunter K, Parrillo JE, Trzeciak S; Emergency Medicine Shock Research Network (EMShockNet) Investigators (2010) Association between arterial hyperoxia following resuscitation from cardiac arrest and in-hospital mortality. JAMA 303:2165–2171
Rønning OM, Guldvog B (1999) Should stroke victims routinely receive supplemental oxygen? A quasi-randomized controlled trial. Stroke 30:2033–2037
Downs JB, Smith RA (1999) Increased inspired oxygen concentration may delay diagnosis and treatment of significant deterioration in pulmonary function. Crit Care Med 27:2844–2846
Carpagnano GE, Kharitonov SA, Foschino-Barbaro MP, Resta O, Gramiccioni E, Barnes PJ (2004) Supplementary oxygen in healthy subjects and those with COPD increases oxidative stress and airway inflammation. Thorax 59:1016–1019
Lumb AB (2000) Hyperoxia and oxygen toxicity. In: Lumb AB (ed) Nunn’s applied respiratory physiology, 5th edn. Butterworth-Heinemann, Edinburgh, pp 500–507
Capellier G, Beuret P, Clement G, Depardieu F, Ract C, Regnard J, Robert D, Barale F (1998) Oxygen tolerance in patients with acute respiratory failure. Intensive Care Med 24:422–428
Jackson AS, Sandrini A, Campbell Ch, Chow S, Thomas PS, Yates DH (2007) Comparison of biomarkers in exhaled breath condensate and bronchoalveolar lavage. Am J Respir Crit Care Med 175:222–227
Romero PV, Rodríguez B, Martínez S, Cañizares R, Sepulveda D, Manresa F (2006) Analysis of oxidative stress in exhaled breath condensate from patients with severe pulmonary infections. Arch Bronconeumol 42:113–119
Cruz MJ, Sánchez-Vidaurre S, Romero PV, Morell F, Muñoz X (2009) Impact of age on pH, 8-isoprostane, and nitrogen oxides in exhaled breath condensate. Chest 135:462–467
Stüber F, Wrigge H, Schroeder S, Wetegrove S, Zinserling J, Hoeft A, Putensen C (2002) Kinetic and reversibility of mechanical ventilation-associated pulmonary and systemic inflammatory response in patients with acute lung injury. Intensive Care Med 28:834–841
Caspersen C, Stensrud T, Thorsen E (2011) Bronchial nitric oxide flux and alveolar nitric oxide concentration after exposure to hyperoxia. Aviat Space Environ Med 11:946–950
Modun D, Krnic M, Vukovic J, Kokic V, Kukoc-Modun L, Tsikas D, Dujic Z (2012) Plasma nitrite concentration decreases after hyperoxia-induced oxidative stress in healthy humans. Clin Physiol Funct Imaging 32:404–408
Acknowledgments
Research grant PI070019 from FIS (Spanish Ministry of Health).
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Fernandez, R., Gili, G., Villagra, A. et al. Assessment of the inflammatory effect of low-dose oxygen in mechanically ventilated patients. Intensive Care Med 39, 711–716 (2013). https://doi.org/10.1007/s00134-012-2801-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-012-2801-z