Abstract
Purpose
In acute kidney injury patients, metabolic acidosis is common. Its severity, duration, and associated changes in mean arterial pressure (MAP) and vasopressor therapy may be affected by the intensity of continuous renal replacement therapy (CRRT). We aimed to compare key aspects of acidosis and MAP and vasopressor therapy in patients treated with two different CRRT intensities.
Methods
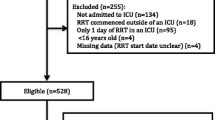
We studied a nested cohort of 115 patients from two tertiary intensive care units (ICUs) within a large multicenter randomized controlled trial treated with lower intensity (LI) or higher intensity (HI) CRRT.
Results
Levels of metabolic acidosis at randomization were similar [base excess (BE) of −8 ± 8 vs. −8 ± 7 mEq/l; p = 0.76]. Speed of BE correction did not differ between the two groups. However, the HI group had a greater increase in MAP from baseline to 24 h (7 ± 3 vs. 0 ± 3 mmHg; p < 0.01) and a greater decrease in norepinephrine dose (from 12.5 to 3.5 vs. 5 to 2.5 μg/min; p < 0.05). The correlation (r) coefficients between absolute change in MAP and norepinephrine (NE) dose versus change in BE were 0.05 and −0.37, respectively.
Conclusions
Overall, LI and HI CRRT have similar acid–base effects in patients with acidosis. However, HI was associated with greater improvements in MAP and vasopressor requirements (clinical trial no. NCT00221013).



Similar content being viewed by others
References
Tresguerres M, Buck J, Levin LR (2010) Physiological carbon dioxide, bicarbonate, and pH sensing. Pflugers Arch 460:953–964
Adrogue HE, Adrogue HJ (2001) Acid-base physiology. Respir Care 46:328–341
Gunnerson KJ (2005) Clinical review: the meaning of acid-base abnormalities in the intensive care unit part I—epidemiology. Crit Care 9:508–516
Bailey JL, Mitch WE (1998) The implications of metabolic acidosis in intensive care unit patients. Nephrol Dial Transplant 13:837–839
Lee SW, Hong YS, Park DW, Choi SH, Moon SW, Park JS, Kim JY, Baek KJ (2008) Lactic acidosis not hyperlactatemia as a predictor of in hospital mortality in septic emergency patients. Emerg Med J 25:659–665
Clermont G, Acker CG, Angus DC, Sirio CA, Pinsky MR, Johnson JP (2002) Renal failure in the ICU: comparison of the impact of acute renal failure and end-stage renal disease on ICU outcomes. Kidney Int 62:986–996
Guth HJ, Zschiesche M, Panzig E, Rudolph PE, Jager B, Kraatz G (1999) Which organic acids does hemofiltrate contain in the presence of acute renal failure? Int J Artif Organs 22:805–810
Naka T, Bellomo R (2004) Bench-to-bedside review: treating acid-base abnormalities in the intensive care unit–the role of renal replacement therapy. Crit Care 8:108–114
Feriani M, Dell’Aquila R (1998) Acid-base balance and replacement solutions in continuous renal replacement therapies. Kidney Int Suppl 66:S156–S159
Nimmo GR, Mackenzie SJ, Walker S, Nicol M, Grant IS (1993) Acid-base responses to high-volume haemofiltration in the critically ill. Nephrol Dial Transplant 8:854–857
Hilton PJ, Taylor J, Forni LG, Treacher DF (1998) Bicarbonate-based haemofiltration in the management of acute renal failure with lactic acidosis. QJM 91:279–283
Davenport A, Will EJ, Davison AM (1989) The effect of lactate-buffered solutions on the acid-base status of patients with renal failure. Nephrol Dial Transplant 4:800–804
Locatelli F, Pontoriero G, Di Filippo S (1998) Electrolyte disorders and substitution fluid in continuous renal replacement therapy. Kidney Int Suppl 66:S151–S155
Evanson JA, Himmelfarb J, Wingard R, Knights S, Shyr Y, Schulman G, Ikizler TA, Hakim RM (1998) Prescribed versus delivered dialysis in acute renal failure patients. Am J Kidney Dis 32:731–738
Bellomo R, Cass A, Cole L, Finfer S, Gallagher M, Lo S, McArthur C, McGuinness S, Myburgh J, Norton R, Scheinkestel C, Su S (2009) Intensity of continuous renal-replacement therapy in critically ill patients. N Engl J Med 361:1627–1638
Kellum JA, Kramer DJ, Pinsky MR (1995) Strong ion gap: a methodology for exploring unexplained anions. J Crit Care 10:51–55
Figge J, Mydosh T, Fencl V (1992) Serum proteins and acid-base equilibria: a follow-up. J Lab Clin Med 120:713–719
Stewart PA (1983) Modern quantitative acid-base chemistry. Can J Physiol Pharmacol 61:1444–1461
Demirjian S, Teo BW, Paganini EP (2008) Alkalemia during continuous renal replacement therapy and mortality in critically ill patients. Crit Care Med 36:1513–1517
Rocktaschel J, Morimatsu H, Uchino S, Ronco C, Bellomo R (2003) Impact of continuous veno-venous hemofiltration on acid-base balance. Int J Artif Organs 26:19–25
Burnell JM, Scribner BH, Uyeno BT, Villamil MF (1956) The effect in humans of extracellular pH change on the relationship between serum potassium concentration and intracellular potassium. J Clin Invest 35:935–939
Bellomo R, Kellum JA, Gandhi CR, Pinsky MR, Ondulik B (2000) The effect of intensive plasma water exchange by hemofiltration on hemodynamics and soluble mediators in canine endotoxemia. Am J Respir Crit Care Med 161:1429–1436
Cole L, Bellomo R, Journois D, Davenport P, Baldwin I, Tipping P (2001) High-volume haemofiltration in human septic shock. Intensive Care Med 27:978–986
Klouche K, Cavadore P, Portales P, Clot J, Canaud B, Beraud JJ (2002) Continuous veno-venous hemofiltration improves hemodynamics in septic shock with acute renal failure without modifying TNFalpha and IL6 plasma concentrations. J Nephrol 15:150–157
Ratanarat R, Brendolan A, Piccinni P, Dan M, Salvatori G, Ricci Z, Ronco C (2005) Pulse high-volume haemofiltration for treatment of severe sepsis: effects on hemodynamics and survival. Crit Care 9:R294–R302
Boussekey N, Chiche A, Faure K, Devos P, Guery B, d’Escrivan T, Georges H, Leroy O (2008) A pilot randomized study comparing high and low volume hemofiltration on vasopressor use in septic shock. Intensive Care Med 34:1646–1653
Huang YG, Wong KC, Yip WH, McJames SW, Pace NL (1995) Cardiovascular responses to graded doses of three catecholamines during lactic and hydrochloric acidosis in dogs. Br J Anaesth 74:583–590
Schulte-Sasse U, Hess W, Schweichel E, Tarnow J, Bruckner JB (1981) Systemic and coronary haemodynamic effects of dobutamine and norepinephrine during metabolic acidosis. Anaesthesist 30:455–460
Peng Z, Pai P, Hong-Bao L, Rong L, Han-Min W, Chen H (2010) The impacts of continuous veno-venous hemofiltration on plasma cytokines and monocyte human leukocyte antigen-DR expression in septic patients. Cytokine 50:186–191
Haase M, Silvester W, Uchino S, Goldsmith D, Davenport P, Tipping P, Boyce N, Bellomo R (2007) A pilot study of high-adsorption hemofiltration in human septic shock. Int J Artif Organs 30:108–117
Ghani RA, Zainudin S, Ctkong N, Rahman AF, Wafa SR, Mohamad M, Manaf MR, Ismail R (2006) Serum IL-6 and IL-1-ra with sequential organ failure assessment scores in septic patients receiving high-volume haemofiltration and continuous veno-venous haemofiltration. Nephrology (Carlton) 11:386–393
Biesheuvel CJ, Vergouwe Y, Oudega R, Hoes AW, Grobbee DE, Moons KG (2008) Advantages of the nested case-control design in diagnostic research. BMC Med Res Methodol 8:48
Vesconi S, Cruz DN, Fumagalli R, Kindgen-Milles D, Monti G, Marinho A, Mariano F, Formica M, Marchesi M, Rene R, Livigni S, Ronco C (2009) Delivered dose of renal replacement therapy and mortality in critically ill patients with acute kidney injury. Crit Care 13:R57
Morris CG, Low J (2008) Metabolic acidosis in the critically ill: part 2. Causes and treatment. Anaesthesia 63:396–411
Oudemans-van Straaten HM, Kellum JA, Bellomo R (2011) Clinical review: anticoagulation for continuous renal replacement therapy—heparin or citrate? Crit Care 15:202
Acknowledgments
We thank the nurses of both participating ICUs (Austin Hospital and Nepean Hospital) for their assistance with the collection of samples and measurements of arterial blood gases. This study was supported by grants from the National Health and Medical Research Council (NHMRC) of Australia (grant no. 352550) and Health Research Council (HRC) of New Zealand (grant no. 06-357).
Conflicts of interest
Professor Cass was supported by a NHMRC Senior Research Fellowship. Professor Bellomo has received consulting fees from Gambro Pty Ltd. Professor Simon Finfer has received travel support to present research results at scientific meetings from Eli Lilly, Cardinal Health, and CSL Bioplasma. The George Institute for International Health, an independent not-for-profit institute affiliated with the University of Sydney, has received reimbursement for Professor Finfer’s time as a steering committee member for studies sponsored by Eli Lilly and Eisai. The George Institute has received research funding from Servier, Novartis, Eisai, Merck, Sharp & Dohme, Pfizer Australia, Fresenius Kabi Deutschland GmbH, and Sanofi Aventis.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
The randomized evaluation of normal versus augmented level (RENAL) Replacement Therapy Study is a collaboration of the Australian and New Zealand Intensive Care Society Clinical Trials Group (ANZICS CTG) and the George Institute for International Health.
The names and affiliations of the RENAL Replacement Therapy Study investigators are listed in the Appendix.
Appendix
Appendix
Writing committee (in alphabetical order): Rinaldo Bellomo (chair), Alan Cass, Louise Cole, Simon Finfer, Martin Gallagher, Serigne N. Lo, Colin McArthur, Shay McGuinness, John Myburgh, Robyn Norton, Carlos Scheinkestel, and Steve Su.
Management committee: (in alphabetical order): Rinaldo Bellomo (chair), David Ali, Alan Cass, Louise Cole, Simon Finfer, Martin Gallagher, Donna Goldsmith, Joanne Lee, John Myburgh, Robyn Norton, and Carlos Scheinkestel.
Steering committee: Rinaldo Bellomo (chair), Ashoke Banerjee Deepak Bhonagiri, David Blythe, John Botha, John Cade, Louise Cole, Geoff Dobb, John Eddington, Simon Finfer, Arthas Flabouris, Craig French, Peter Garrett, Seton Henderson, Benno Ihle, Chris Joyce, Michael Kalkoff, Jeff Lipman, Colin McArthur, Shay McGuinness, David Milliss, Imogen Mitchell, John Morgan, John Myburgh, Priya Nair, Neil Orford, Asif Raza, Carlos Scheinkestel, Yahya Shehabi, Antony Tobin, Richard Totaro, Andrew Turner, and Christopher Wright.
Project management team (in alphabetical order): David Ali, Joanne Lee, Lorraine Little, Alana Morrison, Giovanna Regaglia, and Ravi Shukla
Data safety and monitoring committee (in alphabetical order): Colin Baigent (chair), Jonathan Emberson, David Wheeler, and Duncan Young.
Statistics committee (in alphabetical order): Laurent Billot, Severine Bompoint, Stephane Heritier, Serigne N. Lo, Avinesh Pillai, and Steve Su.
Data management and IT/programming (in alphabetical order): Sameer Pandey, Suzanne Ryan, Manuela Schmidt, Gemma Starzec, and Bala Vijayan
Site investigators and research coordinators (in alphabetical order):
Australian Capital Territory:
Canberra Hospital: Imogen Mitchell, Rebecca Ashley, Jelena Gissane, Katya Malchukova, and Jamie Ranse.
New South Wales:
Blacktown Hospital: Asif Raza, Kiran Nand, and Treena Sara. Concord Hospital: David Millis, Jeff Tan, and Helen Wong. John Hunter Hospital: Peter Harrigan, Elise Crowfoot, and Miranda Hardie. Liverpool Hospital: Deepak Bhonagiri and Sharon Micallef. Mater Calvary Hospital, Newcastle: Jorge Brieva and Melissa Lintott. Nepean Hospital: Louise Cole, Rebecca Gresham, Maria Nikas, and Leonie Weisbrodt. Prince of Wales Hospital: Yahya Shehabi, Frances Bass, Michelle Campbell, and Victoria Stockdale. Royal North Shore Hospital: Simon Finfer, Susan Ankers, Anne O’Connor, and Julie Potter. Royal Prince Alfred Hospital: Richard Totaro and Dorrilyn Rajbhandari. St George Hospital: John Myburgh, Vanessa Dhiacou, Alina Jovanovska, and Francesca Munster. St Vincent’s Hospital: Priya Nair, Jeff Breeding, and Claire Burns. Westmead Hospital: Ashoke Banerjee, Maridy Morrison, Caroline Pfeffercorn, and Anne Ritchie.
New Zealand:
Auckland City Hospital/CVICU: Shay McGuinness, Heidi Buhr, Michelle Eccleston, and Rachael Parke. Auckland City Hospital/DCCM: Colin McArthur, Jeanette Bell, and Lynette Newby. Christchurch Hospital: Seton Henderson and Jan Mehrtens. Whangarei Hospital: Michael Kalkoff and Cathy West
Queensland:
Mater Adult and Mater Private Hospital: John Morgan, Lorraine Rudder, and Joanne Sutton. Nambour General Hospital: Peter Garrett, Nicole Groves, Shona McDonald, and Jennifer Palmer. Princess Alexandra Hospital: Chris Joyce, Meg Harwood, Jean Helyar, and Benjamin Mackie. Royal Brisbane Hospital: Jeff Lipman, Robert Boots, Claire Bertenshaw, Renae Deans, Cheryl Fourie, and Melissa Lassig-Smith.
South Australia:
Royal Adelaide Hospital: Arthas Flabouris, Jason Edwards, Stephanie O’Connor, and Justine Rivett.
Tasmania:
Royal Hobart Hospital: Andrew Turner, Tanya Field, and Kathryn Marsden.
Victoria:
Austin Hospital: Rinaldo Bellomo, Claire Mathlin, Donna Goldsmith, Inga Mercer, and Kim O’Sullivan. Bendigo Hospital: John Edington, Catherine Boschert, and Julie Smith. Epworth Hospital: Benno Ihle, Michael Graan, and Samuel Ho. Frankston Hospital: John Botha, Nina Fowler, Jodi McInness, and Naomi Pratt. Geelong Hospital: Neil Orford, Tania Elderkin, Melissa Fraser, and Anne Kinmonth. Monash Medical Centre: Christopher Wright, Sue Burton, Carly Culhane, Pauline Galt, and Rebecca Rutzou. Royal Melbourne: Megan Roberston, Deborah Barge, Tania Caf, Belinda Howe, and Patzy Low. St Vincent’s Hospital Melbourne: Antony Tobin, Nicole Groves, Jennifer Holmes, and Roger Smith. The Alfred Hospital: Carlos Scheinkestel, Andrew Davies, Lynne Murray, Rachael Nevill, Shirley Vallance, Sue Varley, and Vickie White. Western Hospital: Craig French, Lorraine Little, and Heike Raunow.
Western Australia:
Fremantle Hospital: David Blythe and Anna Palermo. Royal Perth Hospital: Geoff Dobb, Melanie Boardman, Jenny Chamberlain, Andree Gould, Geraldine McEntaggart, Samantha Perryman, and Linda Thomas.
Rights and permissions
About this article
Cite this article
Bellomo, R., Lipcsey, M., Calzavacca, P. et al. Early acid–base and blood pressure effects of continuous renal replacement therapy intensity in patients with metabolic acidosis. Intensive Care Med 39, 429–436 (2013). https://doi.org/10.1007/s00134-012-2800-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-012-2800-0