Abstract
Objective
Candida spp. airway colonization could promote development of ventilator-associated pneumonia (VAP) caused by Pseudomonas aeruginosa, a potentially multidrug-resistant (MDR) bacteria, and worsen the outcome of VAP regardless of pathogen. We therefore address the question of the risk of MDR bacteria isolation within the airway of patients with suspected VAP, whether Candida spp. is present or not.
Design and setting
Prospective observational study in a teaching hospital.
Patients and methods
Consecutive patients with suspected VAP were included. Respiratory tract secretions were seeded on specific medium for yeast isolation in addition to standard culture. Outcome as well as presence of MDR bacteria were assessed according to fungal colonization.
Results
323 suspected VAP were analysed. Among these, 181 (56 %) cases presented with Candida spp. airway colonization. Colonized and noncolonized patients were similar regarding baseline characteristics, prior exposure to antibiotics and VAP severity. However, mortality rate was greater in patients with fungal airway colonization than in those without (44.2 versus 31.0 %, respectively; p = 0.02). In addition, MDR bacteria isolation was 31.5 % in patients with Candida spp. colonization versus 23.2 % in those without (p = 0.13). Moreover, Candida spp. airway colonization was one independent risk factor for MDR bacteria isolation [odds ratio (OR) = 1.79, 95 % confidence interval 1.05–3.05; p = 0.03], in addition to the time elapsed between intensive care unit (ICU) admission and VAP suspicion.
Conclusions
In patients with suspected VAP, Candida spp. airway colonization is frequent and associated with increased risk for MDR bacteria isolation. This could worsen outcome and should therefore be considered when choosing an empiric antibiotic therapy.
Similar content being viewed by others
Introduction
Ventilator-associated pneumonia (VAP) is a great matter of concern in the ICU setting. Accordingly, although VAP’s attributable mortality is still controversial, rates reaching 33 % have been reported [1]. Inappropriate initial antibiotic therapy is clearly associated with poor outcome [2]. However, predicting the risk of difficult-to-treat bacteria including multidrug-resistant (MDR) pathogens is challenging in patients with clinically suspected VAP. The American Thoracic Society guidelines aim at avoiding inappropriate empiric treatment by promoting administration of broad-spectrum antibiotics effective against Pseudomonas aeruginosa in any patient with late-onset VAP or at least one risk factor for carrying such difficult-to-treat pathogen [3].
While the diagnosis of Candida spp. pneumonia should be abandoned in the ICU setting when immunocompetent subjects are considered, fungal airway colonization is a frequent finding in patients submitted to mechanical ventilation (MV) [4–7]. A few retrospective studies have shown that Candida might not be an innocent bystander within the airway. Thus, colonization could promote VAP development, especially if caused by P. aeruginosa, a bacteria likely to become resistant to antimicrobial agents [8]. In addition, retrospective analysis of the data from a large clinical trial that excluded patients with VAP caused by P. aeruginosa showed that higher mortality rates were reported if respiratory secretions grew Candida spp. [9]. Notably, the authors did not consider the appropriateness of the first-line antibiotic therapy. In addition, all these studies were done retrospectively and airway secretion cultures were not performed on specific fungal media, which could have led to underestimation of yeast colonization [10]. In addition, taken together with recent experimental data, these findings suggest that bacteria other than P. aeruginosa could take advantage in the presence of Candida albicans within the airway of patients undergoing MV [11]. We hypothesized that the most resistant species could be thus selected.
We therefore conducted a prospective observational study, whose objective was to unravel the significance of Candida spp. airway colonization in a large cohort of patients with suspected VAP, with special emphasis on survival in the ICU and the potential link with isolation of MDR bacteria.
Methods
Study population
Every patient admitted to our ICU between January 2006 and the end of May 2010 was eligible if submitted to MV for more than 48 h. Each patient with suspected VAP according to physician clinical judgment was included by one of the investigators (P.-E.C., J.-P.Q., S.P. or S.D.B.) throughout the study period. Only the first episode of VAP was considered. In accordance with French law, no informed consent was required since all measurements were part of routine management, as confirmed by our local ethics committee.
Definitions
Bacteria were considered as MDR in the following cases: (1) P. aeruginosa resistant to imipenem and/or antipseudomonal penicillins and one aminoside and/or ciprofloxacine, (2) Enterobacteriaceae if resistant to third-generation cephalosporins and fluoroquinolone and/or an aminoside, (3) Staphylococcus aureus if resistant to oxacillin. Patients with negative tracheal aspirate cultures were considered as free of MDR bacteria.
Ventilator-associated pneumonia was considered as probable if the Clinical Pulmonary Infection Score (CPIS) score was equal to or more than six points.
Data collection
Using a recording form, the “modified” Clinical Pulmonary Infection Score (CPIS) was calculated as previously described [12, 13]. Demographic data and the usually reported risk factors for multidrug-resistant bacteria were also prospectively recorded (i.e. time elapsed between VAP suspicion and ICU admission, previous hospitalization, exposure to antibiotics defined as administration of at least a 2-day antibiotic course within the past 30 days, nursing-home residency, underlying chronic obstructive pulmonary disease). In addition, procalcitonin (PCT) measurement was usually performed in every patient with suspected sepsis as a reliable tool to improve diagnosis and antimicrobial management [14]. Tracheal aspirate sampling was performed in every patient within a 24-h period following the clinical suspicion. Both bacteriological and mycological cultures on specific media for yeast isolation were performed. Results of bacterial cultures were used to calculate the “day 3 CPIS”, since 1 point was added to the value obtained at day 1 if at least ×106 colony-forming units (CFU)/mL were recovered. One point was then added if the direct examination showed the same germ. Finally, the patient was classified as colonized by Candida spp. if airway specimen culture was positive, regardless of the yeast count.
VAP management
Antibiotic therapy management relied on guidelines based on knowledge of the local susceptibility patterns of the most frequently isolated bacteria, as well on the clinical judgment of the attending physician. The first-line treatment (i.e. the one delivered within the first 24 h following clinical suspicion of VAP) was considered as appropriate if the isolated pathogen(s) was (were) susceptible to at least one drug administered at onset of sepsis according to the corresponding susceptibility testing report. When no antibiotic was given within the first 24 h of management, the treatment was considered as inappropriate regardless of the subsequently isolated pathogen.
Statistical analysis
Values are expressed as mean ± standard deviation (SD) unless otherwise stated. In a first set of analysis, patients with suspected VAP were compared according to Candida spp. airway colonization. Continuous variables were compared using the Mann–Whitney U test. Categorical variables were compared using the χ 2 test. We then examined the independent contribution of factors that had been associated with Candida spp. airway colonization through univariate analysis. The candidate variables were manually entered into a logistical regression model if the associated regression coefficient had p value <0.20 on univariate analysis, and then removed if a p value more than 0.05 was obtained on multivariate analysis. The validity of the model was assessed with the Hosmer–Lemeshow test for goodness of fit.
In a second set of analyses, a survival study was performed. Survival of patients regarding Candida spp. airway colonization was analysed by construction of the corresponding Kaplan–Meier curves compared by the log-rank test. In addition, every variable associated with death in the ICU on univariate analysis was then entered into a logistical regression model using the same rule as described above.
Finally, patients in whom a MDR bacteria was isolated within the airway were compared with those without. Univariate analysis was followed by construction of a logistic regression model as described above.
A p value <0.05 was considered as statistically significant for all analyses. STATA software was used for all analyses (College Station, TX, USA).
Results
Patients’ characteristics
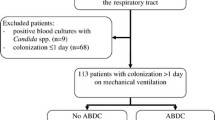
Between 1 January 2006 and 1 April 2010, 354 clinically suspected VAP were recorded. Thirty-one episodes were excluded because of missing data (i.e. no culture on specific medium for yeast isolation available). The remaining 323 were kept for final analysis. The main baseline characteristics of the included patients are presented in Table 1. It is worth noting that the excluded patients were not different from the analysed ones regarding baseline characteristics but presented more frequently with septic shock and had worse outcome (data not shown).
Among the included patients, Candida spp. airway colonization was found in 181 cases (56 %). C. albicans was the most frequently isolated yeast (56 %) (Fig. 1). The baseline characteristics including demographic data and severity score on admission were not different between the two groups (i.e. colonized and not colonized by Candida spp.).
Description of suspected VAP episodes
Among the 323 recorded suspected VAP episodes, 63.5 % were considered as probable according to the CPIS calculation. Those cases were equally distributed between colonized and noncolonized patients (65.7 versus 60.5 %, respectively; p = 0.40). A positive bacterial culture was obtained in around two-thirds of the cases of clinically suspected VAP in each group. Enterobacteriaceae were the most frequently (25.1 %) isolated pathogen when the whole population was considered (Table 1). This proportion reached 28.2 % in the colonized patients and 21.1 % in the patients without Candida spp. airway colonization (p = 0.19). Gram-positive bacteria other than S. aureus were more frequently encountered in the noncolonized patients (10.8 versus 3.9 %, respectively; p = 0.03). However, it is worth noting that P. aeruginosa was found in the same proportions in both groups (17.7 versus 15.5 %, respectively; p = 0.71).
Notably, the isolation of MDR bacteria as defined above was 31.5 % in the patients with concomitant Candida spp. airway colonization and 23.2 % in those without (p = 0.13). The rate of appropriate first-line antibiotic therapy was similar in the two groups (73.3 versus 73.0 %; p = 0.99).
Regarding the severity of the suspected VAP, the colonized patients were not found to be different from the noncolonized ones, since the occurrence of shock (30.4 versus 25.4 %, respectively; p = 0.38) on day 1 was similar, as were the CPIS values (i.e. both day 1 and day 3 values), whose prognosis value has been shown previously [15]. Similar conclusions can be drawn from the PCT measurements obtained on day 1, since no significant difference could be demonstrated (4.7 ± 12.3 versus 3.1 ± 7.6 ng/mL, in colonized and noncolonized patients, respectively; p = 0.24) [16].
Survival analysis
Despite such apparent comparable severity of the disease as well as underlying condition, the ICU mortality of the patients with VAP was found to be significantly greater if Candida spp. airway colonization occurred (44.2 versus 31.0 %, respectively; p = 0.02; Table 2). A time-dependent mortality analysis was also conducted. First, a Kaplan–Meier curve was constructed and confirmed our previous findings, although the log-rank test result was at our limit of statistical significance (p = 0.05) (Fig. 2).
In addition, Candida spp. airway colonization was found to be an independent predictor of death [odds ratio 1.721; 95 % confidence interval (CI) 1.054–2.810; p = 0.030] in addition to age and SAPS II value (Table 3).
Of note, no correlation was found between Candida spp. airway colonization density and outcome (data not shown).
Candida spp. airway colonization as a risk factor for isolation of MDR bacteria
We examined thereafter in our population of patients with clinically suspected VAP the potential link between Candida spp. airway colonization and isolation of MDR bacteria. Almost one-third of the included patients (27.9 %) had a tracheal aspirate culture positive for MDR bacteria. First, patients with MDR were compared with those without using univariate analysis (Table 4). As expected, MDR bacteria were far more likely in patients with hospitalization prior to ICU admission, in those with previous antibiotic exposure as well as in those with prolonged ICU stay or MV duration before clinical suspicion of VAP.
Obviously, antibiotic resistance was mostly encountered among Gram-negative bacilli including Enterobacteriaceae and P. aeruginosa (41.1 and 35.6 % of MDR strains, respectively).
Candida spp. airway colonization was found in 63.3 % of the patients harbouring MDR pathogens and in 53.2 % of the others (p = 0.13). However, it is worth noting that the MDR isolation rate was the same, whether Candida spp. airway colonization was high (i.e. more than ×103 CFU/L) or low. Likewise, among the colonized patients, the proportion of Candida albicans was the same regardless of MDR bacteria isolation (not shown).
In addition, unexpectedly, the suspected VAP episodes could be considered as less severe when MDR bacteria were isolated, since CPIS day 1 value was lower (4.8 ± 1.9 versus 5.2 ± 1.7; p = 0.04). As expected, the rate of appropriate first-line antibiotic therapy was significantly lower in the MDR group (46.7 versus 83.8 %; p < 0.01). ICU mortality was however similar in the two groups (38.9 versus 38.2 %, respectively; p = 0.99).
In an attempt to delineate the role of each risk factor for MDR bacteria isolation, we performed multivariate analysis based on a logistic regression model as described in the “Methods” section. Surprisingly, the only independent predictors of MDR isolation in our model were the time elapsed between ICU admission and VAP suspicion [odds ratio (OR) = 1.04; 95 % confidence interval (CI) 1.02–1.06; p < 0.001] and Candida spp. airway colonization [OR = 1.79; 95 % CI 1.05–3.05; p = 0.03] (Table 5).
Discussion
We report herein that Candida spp. airway colonization is a frequent finding in patients with clinically suspected VAP. Moreover, we show that it is an independent predictor of death in these patients. In addition, to the best of our knowledge, we report for the first time that isolation of MDR bacteria within their airway could be more likely if Candida spp. is present.
It has been shown previously that Candida spp. airway colonization was associated with the risk of developing P. aeruginosa VAP [8]. Similarly, a case–control study has shown that antifungal therapy was likely to prevent such event in one ICU [17]. In addition, a growing body of evidence supports the strong interplay between C. albicans and P. aeruginosa when coexisting within a biofilm environment such as the endotracheal tube or the airway. Finally, defences against P. aeruginosa are altered if the lung has been previously exposed to yeast in a rat model [11]. Altogether, these data emphasize the relationship between Candida spp. airway colonization and P. aeruginosa VAP and provide plausible pathophysiological explanations. However, our results suggest that, beyond P. aeruginosa per se, antibiotic-resistant bacterial strains rather than a single pathogen are more likely to arise from the airway of patients with fungal colonization than from those without. Accordingly it has been shown that S. aureus could acquire one resistant phenotype when growing within mixed culture with Candida spp. [18]. Actually, it is known that biofilm-embedded bacteria are more prone to develop antibiotic-resistant patterns [19]. In addition, the presence of yeast prior to airway bacterial challenge in the rat model of pneumonia described above is likely to promote lung growth of bacteria other than P. aeruginosa, i.e. S. aureus and Escherichia coli [11, 20]. Altogether, these findings suggest that presence of Candida spp. within the respiratory tract facilitates bacterial growth and thereby pneumonia development. Biofilm formation resulting from interactions between the two pathogens could allow bacteria to escape from host immunity as well as antimicrobial agents [21, 22]. This could result in selection of resistant strains and local immunity impairment, leading to treatment failure and worse outcome. Accordingly, as expected, the rate of inappropriate first-line antibiotic therapy was greater if MDR bacteria caused VAP. We failed, however, to demonstrate any relationship between isolation of MDR and outcome. The lower severity of the disease in the group of patients with MDR bacteria could account for this discrepant finding.
The significance of Candida spp. airway colonization is, however, difficult to determine, since it is frequently associated with multifocal colonization, i.e. growth of yeasts elsewhere on the body surface [6, 23]. Accordingly, one cannot exclude that the worse outcome of our patients with clinically suspected VAP and Candida spp. within the airway is related to development of invasive candidiasis, since multifocal colonization is considered as a major risk factor. It is, however, worth noting that no candidaemia was diagnosed among the patients in our cohort. In addition, since gut colonization frequently develops prior to airway colonization, presence of Candida spp. within tracheal aspirate cultures is rarely an isolated finding. Moreover, it has been previously found in large series of patients that occurrence of invasive candidiasis was poorly predicted by presence of yeast within the respiratory tract, since a positive predictive value of 8 % and relative risk of 1.55 [(0.89–2.72); p = 0.119] have been published [6, 23, 24]. We cannot, however, definitively conclude about this point, since fungal culture from multiple sites was not performed in every patient.
Finally, although PCT levels were found to be greater in colonized patients than in the others on the day VAP was clinically suspected, we failed to demonstrate any statistically significant difference. It is therefore hazardous to postulate that colonizing Candida spp. within the respiratory tract could generate systemic inflammation and in turn worsen outcome as suggested elsewhere [25].
Some limitations of our study should be mentioned. It is a single-centre study, and any extrapolation to other ICUs is hazardous. In addition, since we cannot exclude potential but not analysed confounder variables, any causality link between Candida spp. airway colonization, outcome and MDR bacteria isolation should be drawn very cautiously. Finally, since colonization was not assessed routinely before VAP occurred, no temporal relationship between fungal growth and resistant pathogen selection can be concluded.
Conclusions
Candida spp. is frequently retrieved in patients with clinically suspected VAP. This could account for their worse outcome and add some new data to the growing body of evidence supporting the deleterious effect of yeasts in this setting. However, only a clinical trial assessing the impact of antifungal drugs in such patients would be able to answer this issue. The possible increased risk of MDR bacteria isolation from the respiratory tract culture in the presence of yeast remains unexplained. Further studies are therefore needed to confirm our findings and to determine the extent to which Candida spp. airway colonization should be considered when selecting an empiric antibiotic treatment for VAP.
References
Heyland DK, Cook DJ, Griffith L, Keenan SP, Brun-Buisson C (1999) The attributable morbidity and mortality of ventilator-associated pneumonia in the critically ill patient. The Canadian critical trials group. Am J Respir Crit Care Med 159:1249–1256
Luna CM, Aruj P, Niederman MS, Garzon J, Violi D, Prignoni A, Rios F, Baquero S, Gando S (2006) Appropriateness and delay to initiate therapy in ventilator-associated pneumonia. Eur Respir J 27:158–164
American Thoracic Society, Infectious Diseases Society of America (2005) Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med 171:388–416
Meersseman W, Lagrou K, Spriet I, Maertens J, Verbeken E, Peetermans WE, Van Wijngaerden E (2009) Significance of the isolation of Candida species from airway samples in critically ill patients: a prospective, autopsy study. Intensive Care Med 35:1526–1531
Durairaj L, Mohamad Z, Launspach JL, Ashare A, Choi JY, Rajagopal S, Doern GV, Zabner J (2009) Patterns and density of early tracheal colonization in intensive care unit patients. J Crit Care 24:114–121
Magill SS, Swoboda SM, Johnson EA, Merz WG, Pelz RK, Lipsett PA, Hendrix CW (2006) The association between anatomic site of Candida colonization, invasive candidiasis, and mortality in critically ill surgical patients. Diagn Microbiol Infect Dis 55:293–301
Charles PE, Dalle F, Aube H, Doise JM, Quenot JP, Aho LS, Chavanet P, Blettery B (2005) Candida spp. colonization significance in critically ill medical patients: a prospective study. Intensive Care Med 31:393–400
Azoulay E, Timsit JF, Tafflet M, de Lassence A, Darmon M, Zahar JR, Adrie C, Garrouste-Orgeas M, Cohen Y, Mourvillier B, Schlemmer B (2006) Candida colonization of the respiratory tract and subsequent pseudomonas ventilator-associated pneumonia. Chest 129:110–117
Delisle MS, Williamson DR, Perreault MM, Albert M, Jiang X, Heyland DK (2008) The clinical significance of Candida colonization of respiratory tract secretions in critically ill patients. J Crit Care 23:11–17
Arendrup MC, Chryssanthou E, Gaustad P, Koskela M, Sandven P, Fernandez V (2007) Diagnostics of fungal infections in the Nordic countries: we still need to improve! Scand J Infect Dis 39:337–343
Roux D, Gaudry S, Dreyfuss D, El-Benna J, de Prost N, Denamur E, Saumon G, Ricard JD (2009) Candida albicans impairs macrophage function and facilitates Pseudomonas aeruginosa pneumonia in rat. Crit Care Med 37:1062–1067
Fartoukh M, Maitre B, Honore S, Cerf C, Zahar JR, Brun-Buisson C (2003) Diagnosing pneumonia during mechanical ventilation: the clinical pulmonary infection score revisited. Am J Respir Crit Care Med 168:173–179
Singh N, Rogers P, Atwood CW, Wagener MM, Yu VL (2000) Short-course empiric antibiotic therapy for patients with pulmonary infiltrates in the intensive care unit: a proposed solution for indiscriminate antibiotic prescription. Am J Respir Crit Care Med 162:505–511
O’Grady NP, Barie PS, Bartlett JG, Bleck T, Carroll K, Kalil AC, Linden P, Maki DG, Nierman D, Pasculle W, Masur H (2008) Guidelines for evaluation of new fever in critically ill adult patients: 2008 update from the American college of critical care medicine and the infectious diseases society of America. Crit Care Med 36:1330–1349
Luna CM, Blanzaco D, Niederman MS, Matarucco W, Baredes NC, Desmery P, Palizas F, Menga G, Rios F, Apezteguia C (2003) Resolution of ventilator-associated pneumonia: prospective evaluation of the clinical pulmonary infection score as an early clinical predictor of outcome. Crit Care Med 31:676–682
Luyt CE, Guerin V, Combes A, Trouillet JL, Ayed SB, Bernard M, Gibert C, Chastre J (2005) Procalcitonin kinetics as a prognostic marker of ventilator-associated pneumonia. Am J Respir Crit Care Med 171:48–53
Nseir S, Jozefowicz E, Cavestri B, Sendid B, Di Pompeo C, Dewavrin F, Favory R, Roussel-Delvallez M, Durocher A (2007) Impact of antifungal treatment on Candida-Pseudomonas interaction: a preliminary retrospective case-control study. Intensive Care Med 33:137–142
Harriott MM, Noverr MC (2009) Candida albicans and Staphylococcus aureus form polymicrobial biofilms: effects on antimicrobial resistance. Antimicrob Agents Chemother 53:3914–3922
Peters BM, Jabra-Rizk MA, Scheper MA, Leid JG, Costerton JW, Shirtliff ME (2010) Microbial interactions and differential protein expression in Staphylococcus aureus-Candida albicans dual-species biofilms. FEMS Immunol Med Microbiol 59:493–503
Roux D, Gaudry S, Dreyfuss D, El-Benna J, de Prost N, Denamur E, Saumon G, Ricard JD (2009) Candida albicans airway colonization favors bacterial pneumonia. Am J Respir Crit Care Med 179
Morales DK, Hogan DA (2010) Candida albicans interactions with bacteria in the context of human health and disease. PLoS Pathog 6:e1000886
Chandra J, McCormick TS, Imamura Y, Mukherjee PK, Ghannoum MA (2007) Interaction of Candida albicans with adherent human peripheral blood mononuclear cells increases C. albicans biofilm formation and results in differential expression of pro- and anti-inflammatory cytokines. Infect Immun 75:2612–2620
Leon C, Ruiz-Santana S, Saavedra P, Almirante B, Nolla-Salas J, Alvarez-Lerma F, Garnacho-Montero J, Leon MA (2006) A bedside scoring system (“Candida score”) for early antifungal treatment in nonneutropenic critically ill patients with Candida colonization. Crit Care Med 34:730–737
Leon C, Ruiz-Santana S, Saavedra P, Galvan B, Blanco A, Castro C, Balasini C, Utande-Vazquez A, Gonzalez de Molina FJ, Blasco-Navalproto MA, Lopez MJ, Charles PE, Martin E, Hernandez-Viera MA (2009) Usefulness of the “Candida score” for discriminating between Candida colonization and invasive candidiasis in non-neutropenic critically ill patients: a prospective multicenter study. Crit Care Med 37:1624–1633
Williamson DR, Albert M, Perreault MM, Delisle MS, Muscedere J, Rotstein C, Jiang X, Heyland DK (2011) The relationship between Candida species cultured from the respiratory tract and systemic inflammation in critically ill patients with ventilator-associated pneumonia. Can J Anaesth 58:275–284
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is discussed in the editorial available at: doi:10.1007/s00134-012-2587-z.
Rights and permissions
About this article
Cite this article
Hamet, M., Pavon, A., Dalle, F. et al. Candida spp. airway colonization could promote antibiotic-resistant bacteria selection in patients with suspected ventilator-associated pneumonia. Intensive Care Med 38, 1272–1279 (2012). https://doi.org/10.1007/s00134-012-2584-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-012-2584-2