Abstract
Purpose
The sublingual microcirculation can be visualised in real time using sidestream dark-field (SDF) imaging. Endothelial activation mediated through adhesion molecules may alter flow patterns in the microcirculation. We studied sublingual microcirculatory disturbances in children with meningococcal disease (MCD) and simultaneously measured plasma levels of adhesion molecules.
Method
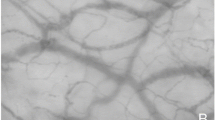
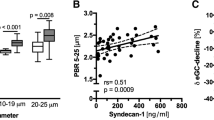
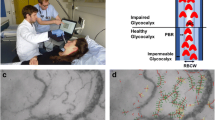
Twenty children admitted to the paediatric intensive care unit (PICU) with MCD were studied. Forty healthy children were controls. The sublingual microcirculation was assessed at admission and at timed intervals until extubation. The microvascular flow index (MFI), capillary density (CD), proportion of perfused vessels (PPV) and perfused vessel density (PVD) were measured using SDF imaging. Plasma intercellular adhesion molecule-1 (ICAM-1), vascular cell adhesion molecule-1 (VCAM-1), E-selectin and P-selectin were measured at admission and at timed intervals during the course of PICU treatment.
Results
Significant reductions in MFI, CD, PPV and PVD were found in children with MCD compared with controls (p < 0.005). These differences had resolved prior to extubation. Initial MFI values predicted the duration of mechanical ventilation, irrespective of the stage of illness at the time of presentation to PICU. There were negative correlations between the ICAM-1, VCAM-1 and E-selectin levels and the microcirculatory MFI and PPV values at the time of admission to PICU (p < 0.005).
Conclusions
Microcirculatory dysfunction is present in children with severe MCD with improvement alongside clinical recovery. Microcirculatory dysfunction correlated with markers of endothelial activation. Sublingual SDF imaging is feasible in children ventilated on PICU for severe sepsis and may prove useful in studies assessing illness severity and therapy.


Similar content being viewed by others
References
Aird WC (2003) The role of the endothelium in severe sepsis and multiple organ dysfunction syndrome. Blood 101:3765–3777
Ince C (2005) Sidestream dark field imaging: an improved technique to observe sublingual microcirculation. Crit Care 9 (Suppl 1) :72
Goedhart PT, Khalilzada M, Bezemer R, Merza J, Ince C (2007) Sidestream dark field (SDF) imaging: a novel stroboscopic LED ring-based imaging modality for clinical assessment of the microcirculation. Opt Exp 15:15101–15114
De Backer D, Creteur J, Preiser JC, Dubois MJ, Vincent JL (2002) Microvascular blood flow is altered in patients with sepsis. Am J Respir Crit Care Med 166:98–104
Trzeciak S, Rivers EP (2005) Clinical manifestations of disordered microcirculatory perfusion in severe sepsis. Critical care (London, England) 9 (Suppl 4):S20–S26
Arnold RC, Parrillo JE, Phillip Dellinger R, Chansky ME, Shapiro NI, Lundy DJ, Trzeciak S, Hollenberg SM (2009) Point-of-care assessment of microvascular blood flow in critically ill patients. Intensive Care Med 35:1761–1766
Boerma EC, Mathura KR, van der Voort PH, Spronk PE, Ince C (2005) Quantifying bedside-derived imaging of microcirculatory abnormalities in septic patients: a prospective validation study. Crit care (London, England) 9:R601–R606
Boerma EC, Koopmans M, Konijn A, Kaiferova K, Bakker AJ, van Roon EN, Buter H, Bruins N, Egbers PH, Gerritsen RT, Koetsier PM, Kingma WP, Kuiper MA, Ince C (2010) Effects of nitroglycerin on sublingual microcirculatory blood flow in patients with severe sepsis/septic shock after a strict resuscitation protocol: a double-blind randomized placebo controlled trial. Crit Care Med 38:93–100
Trzeciak S, Dellinger RP, Parrillo JE, Guglielmi M, Bajaj J, Abate NL, Arnold RC, Colilla S, Zanotti S, Hollenberg SM (2007) Early microcirculatory perfusion derangements in patients with severe sepsis and septic shock: relationship to hemodynamics, oxygen transport, and survival. Ann Emerg Med 49:88–98, 98 e81–e82
Top A, Ince C, De Meij N, van Dijk M, Tibboel D (2011) Persistent low microcirculatory vessel density in nonsurvivors of sepsis in pediatric intensive care. Crit Care Med 39:8–13
Top AP, van Dijk M, van Velzen JE, Ince C, Tibboel D (2011) Functional capillary density decreases after the first week of life in term neonates. Neonatology 99:73–77
Heyderman RS, Ben-Shlomo Y, Brennan CA, Somerset M (2004) The incidence and mortality for meningococcal disease associated with area deprivation: an ecological study of hospital episode statistics. Arch Dis Child 89:1064–1068
Fellick JM, Sills JA, Marzouk O, Hart CA, Cooke RW, Thomson AP (2001) Neurodevelopmental outcome in meningococcal disease: a case-control study. Arch Dis Child 85:6–11
Slack R, Hawkins KC, Gilhooley L, Addison GM, Lewis MA, Webb NJ (2005) Long-term outcome of meningococcal sepsis-associated acute renal failure. Pediatr Crit Care Med 6:477–479
Belthur MV, Bradish CF, Gibbons PJ (2005) Late orthopaedic sequelae following meningococcal septicaemia. A multicentre study. J Bone Joint Surg Br 87:236–240
Stuart JM, Monk PN, Lewis DA, Constantine C, Kaczmarski EB, Cartwright KA (1997) Management of clusters of meningococcal disease. PHIS Meningococcus Working Group and Public Health Medicine Environmental Group. Commun Dis Rep 7:R3–R5
Brilli RJ, Goldstein B (2005) Pediatric sepsis definitions: past, present, and future. Pediatr Crit Care Med 6:S6–S8
Pollack MM, Patel KM, Ruttimann UE (1996) PRISM III: an updated pediatric risk of mortality score. Crit Care Med 24:743–752
Leteurtre S, Martinot A, Duhamel A, Proulx F, Grandbastien B, Cotting J, Gottesman R, Joffe A, Pfenninger J, Hubert P, Lacroix J, Leclerc F (2003) Validation of the paediatric logistic organ dysfunction (PELOD) score: prospective, observational, multicentre study. Lancet 362:192–197
Riordan FA, Marzouk O, Thomson AP, Sills JA, Hart CA (2002) Prospective validation of the Glasgow meningococcal septicaemia prognostic score. comparison with other scoring methods. Eur J Pediatr 161:531–537
Skippen PW, Krahn GE (2005) Acute renal failure in children undergoing cardiopulmonary bypass. Crit Care Resusc 7:286–291
De Backer D, Hollenberg S, Boerma C, Goedhart P, Buchele G, Ospina-Tascon G, Dobbe I, Ince C (2007) How to evaluate the microcirculation: report of a round table conference. Crit care (London, England) 11:R101
Spronk PE, Ince C, Gardien MJ, Mathura KR, Oudemans-van Straaten HM, Zandstra DF (2002) Nitroglycerin in septic shock after intravascular volume resuscitation. Lancet 360:1395–1396
Sakr Y, Dubois MJ, De Backer D, Creteur J, Vincent JL (2004) Persistent microcirculatory alterations are associated with organ failure and death in patients with septic shock. Crit Care Med 32:1825–1831
Spanos A, Jhanji S, Vivian-Smith A, Harris T, Pearse R (2010) Early microvascular changes in sepsis and severe sepsis. Shock (Augusta GA) 33:387–391
Baines PB, Marzouk O, Thomson AP, Sills JA, Riordan FA, Hart CA (1999) Endothelial cell adhesion molecules in meningococcal disease. Arch Dis Child 80:74–76
Pearson JD (2000) Normal endothelial cell function. Lupus 9:183–188
Lampugnani MG, Caveda L, Breviario F, Del MA, Dejana E (1993) Endothelial cell-to-cell junctions. Structural characteristics and functional role in the regulation of vascular permeability and leukocyte extravasation. Baillieres Clin Haematol 6:539–558
Faust SN, Levin M, Harrison OB, Goldin RD, Lockhart MS, Kondaveeti S, Laszik Z, Esmon CT, Heyderman RS (2001) Dysfunction of endothelial protein C activation in severe meningococcal sepsis. N Engl J Med 345:408–416
Singer M, Brealey D (1999) Mitochondrial dysfunction in sepsis. Biochem Soc Symp 66:149–166
Parthasarathi K, Lipowsky HH (1999) Capillary recruitment in response to tissue hypoxia and its dependence on red blood cell deformability. Am J Physiol 277:H2145–H2157
Marechal X, Favory R, Joulin O, Montaigne D, Hassoun S, Decoster B, Zerimech F, Neviere R (2008) Endothelial glycocalyx damage during endotoxemia coincides with microcirculatory dysfunction and vascular oxidative stress. Shock (Augusta Ga) 29:572–576
Goedhart PKM, Bezemer R, Merza J, Ince C (2007) Sidestream Dark Field (SDF) imaging: a novel stroboscopic LED ring-based imaging modality for clinical assessment of the microcirculation. Opt Soc Am 15:15101–15114
Dubin A, Pozo MO, Casabella CA, Murias G, Palizas F, Jr., Moseinco MC, Kanoore Edul VS, Palizas F, Estenssoro E, Ince C (2010) Comparison of 6% hydroxyethyl starch 130/0.4 and saline solution for resuscitation of the microcirculation during the early goal-directed therapy of septic patients. J Crit Care 25:659 e651–e658
Morelli A, Donati A, Ertmer C, Rehberg S, Lange M, Orecchioni A, Cecchini V, Landoni G, Pelaia P, Pietropaoli P, Van Aken H, Teboul JL, Ince C, Westphal M (2010) Levosimendan for resuscitating the microcirculation in patients with septic shock: a randomized controlled study. Crit Care 14:R232
Ospina-Tascon G, Neves AP, Occhipinti G, Donadello K, Buchele G, Simion D, Chierego ML, Silva TO, Fonseca A, Vincent JL, De Backer D (2010) Effects of fluids on microvascular perfusion in patients with severe sepsis. Intensive Care Med 36:949–955
Brierley J, Peters MJ (2008) Distinct hemodynamic patterns of septic shock at presentation to pediatric intensive care. Pediatrics 122:752–759
Koch M, De Backer D, Vincent JL, Barvais L, Hennart D, Schmartz D (2008) Effects of propofol on human microcirculation. Br J Anaesth 101:473–478
Boerma C, van der Voort P, Spronk P, Ince C (2007) Relationship between sublingual and intestinal microcirculatory perfusion in patients with abdominal sepsis. Crit Care Med 35:1055–1060
Verdant CL, De Backer D, Bruhn A, Clausi CM, Su F, Wang Z, Rodriguez H, Pries AR, Vincent JL (2009) Evaluation of sublingual and gut mucosal microcirculation in sepsis: a quantitative analysis. Crit Care Med 37:2875–2881
Acknowledgments
We thank the medical and nursing staff of the Paediatric Intensive Care Units in Liverpool and Manchester for their contribution to the management of these children, and to the parents and children for consenting to be included in the study. We also thank the Meningitis Research Foundation for funding the project. F.P. was supported by a grant from the Meningitis Research Foundation, UK (grant no. 0605.1).
Conflicts of interest
All authors declare that there are no potential, perceived, or real conflicts of interest in the preparation of this manuscript. The authors have full control of all primary data and agree to allow the journal to review their data if requested. The study sponsor was not involved in study design, the collection, analysis, and interpretation of data, the writing of the report or the decision to submit the paper for publication.
Ethical standards
This study has been approved by the local ethics committee and has therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki. All persons gave their informed consent prior to their inclusion in the study.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary material 1 (2,071 M4V)
Supplementary material 2 (1,982 M4V)
Appendix
Appendix
Anaesthesia technique
Children aged 6 years or less were recruited from a non-syndromic population undergoing cosmetic cranioplasty for single-suture synostosis or surgery for spinal dysraphism. They were otherwise healthy and had no evidence of raised intracranial pressure. Anaesthesia was induced with either intravenous propofol (3–4 mg/kg) or sevoflurane by inhalation. They were then paralysed with atracurium (0.6 mg/kg), intubated and ventilated. Ventilation was adjusted to maintain normocapnia and an end-tidal sevoflurane value of 1.3 times the minimal alveolar concentration (MAC). Core temperature was maintained with a forced air-warming device (The Bair Hugger; Arizant Healthcare, Inc.).
Sublingual images and standard vital sign measurements were then obtained in the anaesthetic room before giving any further intravenous drugs or fluids and preparing the patient for surgery.
Rights and permissions
About this article
Cite this article
Paize, F., Sarginson, R., Makwana, N. et al. Changes in the sublingual microcirculation and endothelial adhesion molecules during the course of severe meningococcal disease treated in the paediatric intensive care unit. Intensive Care Med 38, 863–871 (2012). https://doi.org/10.1007/s00134-012-2476-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-012-2476-5