Abstract
Purpose
More than a disorder of macrocirculation, sepsis is a disease affecting the microcirculation and the tissue metabolism. In vivo microdialysis (MD) is a bedside technique that can monitor tissue metabolic changes. We conducted this study aiming (1) to assess whether patients at different sepsis stages present with different MD-assessed tissue metabolic profiles and (2) to determine if different underlying types of infections and implicated pathogens are associated with dissimilar metabolic alterations.
Methods
We studied 90 mechanically ventilated patients, 65 with septic shock and 25 with severe sepsis. An MD catheter was inserted in the subcutaneous adipose tissue of the upper thigh and interstitial fluid samples were collected along with arterial blood samples every 4 h for a maximum of 6 days. Lactate, pyruvate, glycerol, and glucose concentrations were measured.
Results
During the study period, patients with septic shock had higher MD-assessed glycerol (P = 0.009), glycerol gradient (P = 0.016), and glucose (P = 0.004) than patients with severe sepsis, whereas tissue lactate, lactate gradient, and pyruvate dropped significantly with time (P = 0.007, <0.001, and <0.001, respectively) in both patient groups without any observed between-group difference. In addition, there was no between-group difference in their tissue lactate/pyruvate ratio on any day, nor did the ratio decrease significantly with time. Compared with pneumonia patients, and despite similar baseline clinical characteristics, those suffering from intra-abdominal infections showed a pattern of higher and progressively increasing tissue levels of glucose (P = 0.001) and glycerol (P = 0.001). Finally, patients harboring Gram-positive infections had higher tissue levels of glycerol (P = 0.027) and glycerol gradient (P = 0.029) than patients with Gram-negative infections.
Conclusions
MD can detect tissue metabolic abnormalities that differ in relation to the sepsis stage and the type of underlying infection or responsible pathogen. Some of the MD-assessed abnormalities are not reflected by conventional blood measurements and possess prognostic potential. It remains to be determined if this type of metabolic monitoring can find clinical applications in the wide population of septic critically ill patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
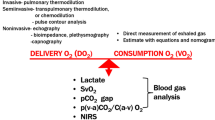
Clinicians are trained to manage sepsis by focusing on its macrocirculatory effects (i.e., restoration of blood pressure drop); however, sepsis is also a disorder of the microcirculation [1] and the cellular metabolism [2]. Even though the bedside evaluation of these less obvious derangements has been historically considered difficult and not clinically useful, recently the diagnostic and therapeutic targeting of the microcirculation distinct from the macrocirculation has been shown to improve outcome in sepsis [3, 4].
The microdialysis (MD) technique was developed 35 years ago [5] and proved its value in several preclinical and clinical applications [6]. Even though MD is widely used in neurointensive care [7], its application in the intensive care setting has focused either on subpopulations of critically ill patients [8, 9] or measurement of tissue antibiotic levels [10]. In a recently published review [11], MD was the technique with the smallest evidence base. However, MD has been lately attracted renewed interest. Specifically, MD-measured lactate at the quadriceps muscle has been proposed to be an important metabolic signal in septic shock patients [12], whereas an increased muscle-to-serum lactate gradient in patients with severe sepsis may be a beacon of progression to septic shock [13].
Subcutaneous adipose tissue (SAT), a probably more convenient site to place an MD device than the muscle [13] or the rectal lumen [14], has been historically viewed as an inert tissue merely storing energy. Nevertheless, it was lately recognized that adipose tissue alterations may be important during the course of critical illness [15]. Until recently, the sepsis-induced metabolic alterations at the SAT level had been studied by means of the MD technique only in small-scale investigations [16]. Our research group showed in a pilot study that MD could be safely applied at the bedside and detect metabolic perturbations in the SAT of septic patients [17].
In order to further expand our experience with microdialysis in septic patients, we conducted this study aiming (1) to assess whether patients at different sepsis stages present with different MD-assessed metabolic profiles, (2) to examine whether different infections have various effects on MD-monitored tissue parameters, and (3) to determine if Gram-positive infections are associated with different metabolic profiles than Gram-negative infections. As a secondary aim of this research project, we investigated if MD-derived parameters may serve as mortality predictors.
Methods
Study population
The study was approved by the hospital’s ethics committee and informed consent was obtained from patients’ relatives. This prospective, observational study included a convenience sample of critically ill, septic patients admitted to the 25-bed mixed adult ICU of a university hospital between March 2008 and October 2010. A patient was included in the study if he/she met the inclusion criteria and the operators (MT and AD) for MD catheter placement were present in the ICU in the first 24 h of the septic syndrome. There were no exclusion criteria.
Microdialysis technique
A microdialysis catheter (CMA 60, CMA Microdialysis AB, Stockholm, Sweden) was inserted upon sepsis onset (defined as day 1) into the upper thigh’s SAT. Sampling was performed six times per day for a maximum of 6 days after sepsis onset and samples were analyzed for lactate, pyruvate, glycerol, and glucose by an automatic analyzer. The physicians responsible for patients’ care were unaware of the MD results.
Data collection: definitions
Upon study entry, we recorded for each patient relevant demographic and physiologic data and employed established metrics and definitions [18–20].
Statistical analysis
Results are presented as means ± standard deviation (SD), medians (interquartile range, IQR), and counts (percentages), as appropriate. Group comparisons were performed by the Fisher’s exact test or Mann–Whitney test, as appropriate. All statistics were two-tailed and P < 0.05 was considered statistically significant in all analyses.
Mixed model analysis was performed using SPSS 15.0 (SPSS Inc., Chicago, IL, USA) and the rest of the statistical analysis was performed with SigmaPlot 11.0 (Systat, San Jose, CA, USA). Figures were created using GraphPad Prism 5.00 for Windows (GraphPad Software, San Diego, CA, USA).
Additional information on the study population, microdialysis technique and measurements, data collection and definitions, statistical analysis, and results and discussion is given in the electronic supplementary material (ESM).
Results
Study population
We studied 90 septic patients. The details of their baseline characteristics are depicted in Table 1 and the ESM. Ten nonseptic/uninfected ICU patients meeting only systemic inflammatory response syndrome (SIRS) criteria were added in a post hoc analysis and served as the control group.
Comparison between patients with septic shock and severe sepsis
Lactate
Mixed model analysis showed that tissue lactate level did not differ when comparing patients with septic shock with those experiencing severe sepsis, whereas it dropped significantly with time (P = 0.007) in both groups (Fig. 1a). On the contrary, blood lactate differed between the two groups for the whole study period (P = 0.014) (Fig. 1b).
The adipose tissue–blood lactate gradient was not different between the two septic groups, whereas it decreased significantly with time (P < 0.001) (Fig. 2a). Additional information on the results regarding the tissue–blood lactate gradient is given in the ESM.
On day 1, there was a significant correlation between tissue lactate and blood lactate (r = 0.48, P < 0.001), tissue glucose (r = 0.32, P < 0.05), and norepinephrine infusion rate (r = 0.28, P < 0.05). On days 2–6, correlation between tissue and blood lactate slightly improved (r = 0.52–0.60, P < 0.001). There was no correlation with SOFA, APACHE II, and mean arterial pressure (MAP).
Pyruvate
Patients with septic shock had numerically higher MD-assessed tissue pyruvate than patients with severe sepsis during each one of the six study days. Mixed model analysis showed that tissue pyruvate dropped significantly with time (P < 0.001) in both groups without any observed between-group difference.
On day 1, tissue pyruvate had a significant correlation with tissue lactate (r = 0.74, P < 0.001), tissue glucose (r = 0.43, P < 0.001), and tissue glycerol (r = 0.44, P < 0.001). It also correlated with the norepinephrine infusion rate (r = 0.23, P < 0.05) but not with the MAP (r = 0.05, P = 0.64).
Lactate/pyruvate (L/P) ratio
There was no difference between patients with septic shock and severe sepsis regarding their tissue L/P ratio on any day, nor did the ratio decrease significantly with time. The L/P ratio for the whole study cohort was 20.46 (15.57–26.63) on day 1 and decreased nonsignificantly until the end of the study. There was no correlation of L/P ratio with SOFA, APACHE II, MAP, and norepinephrine infusion rate.
Glycerol
Patients with septic shock had higher MD-assessed tissue glycerol than patients with severe sepsis during each one of the six days of the study (Fig. 3). Mixed model analysis revealed that in septic shock patients MD glycerol increased throughout the study period, whereas it remained stable in severe sepsis; the difference was statistically significant (P = 0.009). There was also a trend for higher blood glycerol levels among septic shock patients but this did not reach statistical significance (P = 0.075).
Tissue glycerol showed a weak correlation with blood glycerol (r = 0.29, P = 0.008), norepinephrine infusion dose (r = 0.39, P < 0.001), and APACHE II score (r = 0.27, P = 0.01) on day 1 and a trend to correlation with SOFA on day 1 (r = 0.18, P = 0.08) that became significant on day 2 (r = 0.23, P = 0.029). It also correlated with tissue glucose (r = 0.43, P < 0.001), tissue lactate (r = 0.43, P < 0.001), and tissue pyruvate (r = 0.44, P < 0.001).
Mixed model analysis showed that the tissue–blood glycerol gradient was significantly higher (P = 0.016) in the septic shock group throughout the study (Fig. 2b). Additional information on the results regarding the tissue–blood glycerol gradient is given in the ESM.
Glucose
Tissue glucose was significantly higher among septic shock patients compared with the severe sepsis patients (P = 0.004) throughout the study period (Fig. 4). Blood glucose was also higher in septic shock patients but the difference was not statistically significant. MD-assessed glucose correlated with the administered insulin dose and the blood glucose throughout the study period. Specifically, tissue glucose was lower than blood glucose on each one of the study days. Finally, on day 1 it showed significant correlation with each one of the MD-measured parameters.
Comparison between septic patients with or without bacteremia
Compared with nonbacteremic patients (n = 67), patients with bacteremia (n = 23) had higher SOFA (9.35 ± 2.12 vs. 7.19 ± 3.05; P = 0.002) and APACHE II scores (21.61 ± 3.58 vs. 18.76 ± 5.47; P = 0.022) on day 1. There was no appreciable difference in any of the MD-assessed markers except for a slight increase in the blood lactate levels [1.42 (1.16–2.84) vs. 1.23 (0.87–2.13) mmol/l; P = 0.042] in the bacteremic group. Interestingly, bacteremic patients with pneumonia (n = 10) had significantly higher tissue glycerol levels [421.00 (231.00–513.60) vs. 191.67 (134.80–341.23) μmol/l; P = 0.049] than nonbacteremic pneumonia patients (n = 37) on day 1, even though they did not differ either in blood glycerol levels or in SOFA/APACHE II scores.
Comparison between septic patients with different underlying infections
Even though there was no between-groups difference, intra-abdominal infection (IAI) patients showed a pattern of progressively increasing tissue levels of glucose and glycerol compared with a pattern of stable values in pneumonia patients (Fig. 5a, b). This pattern mirrored the evolution of blood glucose and glycerol levels in the first days of the septic syndrome. Mixed model analysis revealed that IAI versus pneumonia infections were associated with higher blood lactate levels throughout the study (P = 0.045). Overall, IAI patients were in a more severe condition; more IAI patients presented with septic shock than pneumonia patients (93.3 vs. 62.5%, P = 0.026) even though they did not differ in age (63.06 ± 16.80 vs. 65.60 ± 15.60 years; P = 0.60), gender (males 60 vs. 72.9%; P = 0.35), APACHE II (21.27 ± 4.30 vs. 19.44 ± 5.70; P = 0.26), and SOFA scores (8.80 ± 3.47 vs. 7.17 ± 2.76; P = 0.07).
The comparison between patients with CAP versus those with HCAP/HAP/VAP did not reveal any difference either in clinical characteristics or in tissue or blood metabolic parameters.
Comparison between septic patients harboring Gram (+) versus Gram (−) infections
There were 34 microbiologically confirmed Gram (−) and 10 Gram (+) infections. Even though there were no between-group differences in clinical characteristics (namely, age, gender, SOFA, and APACHE II scores) on day 1, patients with Gram (+) infections demonstrated higher tissue glycerol levels (422.76 ± 240.76 vs. 256.86 ± 188.39 μmol/l; P = 0.027) and glycerol gradient (397.16 ± 236.87 vs. 232.07 ± 191.56 μmol/l; P = 0.029) than those with Gram (−) infections. Of note, blood glycerol levels did not differ between the two groups.
Comparison between survivors and nonsurvivors
Univariate analysis showed that among all clinical variables, SOFA (P = 0.0001) and APACHE II (P = 0.003) scores, septic shock (P = 0.034), infection type (pneumonia), and norepinephrine infusion rate (P = 0.003) were associated with 28-day mortality; the same was true for the following metabolic markers: MD-derived L/P ratio (P = 0.025), glycerol (P = 0.10), and blood glycerol (P = 0.049) (all performed on day 1) (Table 2). In two multiple logistic regression analyses, we separately included SOFA and APACHE II scores in combination with the relevant variables emerging from the univariate analysis. There was no appreciable collinearity (with tolerance ranging from 0.522 to 0.944 and variance inflation factor ranging from 1.058 to 1.915). The backward elimination technique revealed that the MD L/P ratio remained significant in both multivariate analyses. Specifically, model 1 included MD L/P ratio (OR = 1.042; 95% CI 1.002–1.082) and norepinephrine infusion rate (OR = 1.105; 95% CI 1.033–1.182) and model 2 included MD L/P ratio (OR = 1.040; 95% CI 1.003–1.079) and SOFA score (OR = 1.450; 95% CI 1.168–1.800). Nevertheless, neither model was associated with a significantly larger area under the curve (AUC) than SOFA score alone (Fig. 1 in ESM).
Comparison between patients with severe sepsis/septic shock versus patients with SIRS
The relevant data are presented in the ESM.
Discussion
Our study demonstrated that critically ill patients with septic shock differed from those with severe sepsis in MD-assessed SAT glycerol, glycerol gradient, and glucose, whereas lactate, lactate gradient, pyruvate, and L/P ratio were quite similar. Moreover, compared with the whole cohort of pneumonia patients, and despite similar baseline clinical characteristics, those suffering from IAI or bacteremic pneumonia had different tissue metabolic profiles. This was also the case for the comparison between patients with Gram-positive versus Gram-negative infections. Finally, tissue-derived L/P ratio was an independent predictor for 28-day mortality.
We found that MD-monitored lactate and pyruvate levels were higher—albeit in a not statistically significant way—in patients with septic shock compared with those with severe sepsis. These two tissue biochemical markers showed a good correlation with each other and changed in parallel which is not surprising considering that lactate production is biochemically associated tightly with pyruvate changes. In cases of insufficient oxygen supply, pyruvate is preferentially converted to lactate; this is why lactate is generally viewed as a marker of tissue ischemia and hypoxia. However, lactate can also be produced by overactivation of the glycolytic pathway that leads to proportional increases of pyruvate and lactate in patients with septic shock [12]. We should additionally note that although adipose tissue is considered to contribute significantly to lactate production in healthy subjects [21], there is some controversy regarding the site of increased lactate production in sepsis. For example, Martinez et al. [16] found a tissue–blood lactate gradient that was essentially zero and concluded that adipose tissue does not play a role in the development of hyperlactatemia in critically ill septic patients. That study included only five septic patients and is not in accordance with our findings.
It is known that lipolysis releases glycerol and free fatty acids, a biochemical process that is under the control not only of the sympathetic system and insulin [22] but also of cytokines [23]. In our study, glycerol was found to be the most consistently elevated tissue marker and, thus, clearly differed between patients with septic shock and severe sepsis. Lind and Lithell [24] studied a heterogeneous population of 44 ICU patients and showed that blood glycerol level correlated with disease severity. In addition, it was significantly elevated in septic patients compared with nonseptic ones and improved the predictive ability of the APACHE II score. Less is known about tissue glycerol in septic patients. In the study by Martinez et al. [16], septic patients had higher tissue glycerol levels as well as tissue–blood glycerol gradients than healthy subjects. This is in keeping with the results of this study and our previous research project [17]. In that study, we additionally found that tissue glycerol was higher compared with blood glycerol during the whole study period. This may probably be attributed to ongoing lipolysis. Another interpretation of the increased tissue glycerol levels might be widespread cell membrane disintegration because glycerol is a component of cell membranes. Regardless of the underlying mechanisms, tissue glycerol seems to be a stress response marker. It is noteworthy that—contrary to the lactate gradient—glycerol tissue-to-blood gradient was almost always positive and increased during the 6-day study period. This suggests that a decrease in the lactate recovery rate is not an explanation for the diminution over time of lactate gradient and also implies that the glycerol gradient is an interesting marker of in vivo lipolysis.
Previous epidemiological studies conducted in the ICU setting have shown that although respiratory tract infections are more common, IAIs may be more severe [25]. Our study corroborates these findings because more patients with IAI had septic shock upon study entry. In addition, our data provide the first indirect evidence that the underlying type of infection and the implicating pathogen may be associated not only with different stimulation patterns of the immune system [26, 27] but also with various metabolic alterations.
The limitations of our study should be acknowledged. First, we did not perform any direct measurements of blood flow or substrate kinetics. Second, we did not perform arterial and microdialysis urea measurements as a check for the MD probe recovery function. Therefore, we cannot exclude the possibility that occasional probe dysfunction might be responsible for the negative gradients observed in some patients. However, the glycerol gradient was found to be negative only once. In addition, the L/P ratio calculation from the simultaneous sampling and measurement of lactate and pyruvate would not be expected to be changed by probe dysfunction as both metabolites would be affected to a similar degree. Third, for obvious logistic and cost concerns, we placed only one MD catheter per patient in the SAT of the upper thigh and cannot be certain if the same metabolic alterations would be evident in other body sites. Fourth, the choice of a 4-h sampling schedule, even though more convenient for routine monitoring, might not have detected the effects of short-term interventions (escalation of a vasopressor agent [28], fluid challenge [29], etc.) on microcirculatory and tissue metabolism functions; however, the detection of these effects was not among our study goals. Fifth, we included both lean and obese patients with potentially different patterns of adipose tissue blood flow and metabolism. Finally, we cannot extrapolate our findings to other subpopulations of critically ill patients because we restricted our analysis to the septic patients and did not use a control group of sufficient sample size.
Conclusions
Our data suggest that among septic ICU patients in vivo microdialysis detects tissue metabolic abnormalities that might differ in relation to the sepsis stage and the type of underlying infection or responsible pathogen. Because microdialysis has not been sufficiently studied in sepsis, we consider it at present useful only as a research tool. Additional work will be necessary to determine if microdialysis can find clinical applications in the management of septic patients.
References
Ince C (2005) The microcirculation is the motor of sepsis. Crit Care 9:S13–S19
Brealey D, Singer M (2003) Mitochondrial dysfunction in sepsis. Curr Infect Dis Rep 5:365–371
Trzeciak S, McCoy JV, Phillip Dellinger R, Arnold RC, Rizzuto M, Abate NL, Shapiro NI, Parrillo JE, Hollenberg SM (2008) Early increases in microcirculatory perfusion during protocol-directed resuscitation are associated with reduced multi-organ failure at 24 h in patients with sepsis. Intensive Care Med 34:2210–2217
Hollenberg SM (2010) Think locally: evaluation of the microcirculation in sepsis. Intensive Care Med 36:1807–1809
Ungerstedt U, Pycock C (1974) Functional correlates of dopamine neurotransmission. Bull Schweiz Akad Med Wiss 30:44–55
Muller M (2002) Science, medicine, and the future: microdialysis. BMJ 324:588–591
Ungerstedt U, Rostami E (2004) Microdialysis in neurointensive care. Curr Pharm Des 10:2145–2152
Samuelsson A, Steinvall I, Sjöberg F (2006) Microdialysis shows metabolic effects in skin during fluid resuscitation in burn-injured patients. Crit Care 10:R172
Verdant CL, Chierego M, De Moor V, Chamlou R, Creteur J, de Dieu Mutijima J, Loi P, Gelin M, Gullo A, Vincent JL, De Backer D (2006) Prediction of postoperative complications after urgent laparotomy by intraperitoneal microdialysis: a pilot study. Ann Surg 244:994–1002
Joukhadar C, Frossard M, Mayer BX, Brunner M, Klein N, Siostrzonek P, Eichler HG, Müller M (2001) Impaired target site penetration of beta-lactams may account for therapeutic failure in patients with septic shock. Crit Care Med 29:385–391
De Backer D, Ospina-Tascon G, Salgado D, Favory R, Creteur J, Vincent JL (2010) Monitoring the microcirculation in the critically ill patient: current methods and future approaches. Intensive Care Med 36:1813–1825
Levy B, Gibot S, Franck P, Cravoisy A, Bollaert PE (2005) Relation between muscle Na+K+ ATPase activity and raised lactate concentrations in septic shock: a prospective study. Lancet 365:871–875
Levy B, Perez P, Gibot S, Gerard A (2010) Increased muscle-to-serum lactate gradient predicts progression towards septic shock in septic patients. Intensive Care Med 36:1703–1709
Ibsen M, Tenhunen J, Wiis J, Waldau T, Lauritsen AØ, Thornberg K, Joensen H, Perner A (2010) Lactate concentrations in the rectal lumen in patients in early septic shock. Acta Anaesthesiol Scand 54:827–832
Langouche L, Perre SV, Thiessen S, Gunst J, Hermans G, D’Hoore A, Kola B, Korbonits M, Van den Berghe G (2010) Alterations in adipose tissue during critical illness: an adaptive and protective response? Am J Respir Crit Care Med 182:507–516
Martinez A, Chiolero R, Bollman M, Revelly JP, Berger M, Cayeux C, Tappy L (2003) Assessment of adipose tissue metabolism by means of subcutaneous microdialysis in patients with sepsis or circulatory failure. Clin Physiol Funct Imaging 23:286–292
Dimopoulou I, Nikitas N, Orfanos SE, Theodorakopoulou M, Vassiliadi D, Ilias I, Ikonomidis I, Boutati E, Maratou I, Tsangaris I, Karkouli G, Tsafou E, Diamantakis A, Kopterides P, Maniatis N, Kotanidou A, Armaganidis A, Ungerstedt U (2011) Kinetics of adipose tissue microdialysis-derived metabolites in critically ill septic patients: associations with sepsis severity and clinical outcome. Shock 35:343–348
Knaus WA, Draper EA, Wagner DP, Zimmerman JE (1985) APACHE II: a severity of disease classification system. Crit Care Med 13:818–829
Vincent JL, de Mendonça A, Cantraine F, Moreno R, Takala J, Suter PM, Sprung CL, Colardyn F, Blecher S (1998) Use of the SOFA score to assess the incidence of organ dysfunction/failure in intensive care units: results of a multicenter, prospective study. Working group on “sepsis-related problems” of the European Society of Intensive Care Medicine. Crit Care Med 26:1793–1800
Gogos C, Kotsaki A, Pelekanou A, Giannikopoulos G, Vaki I, Maravitsa P, Adamis S, Alexiou Z, Andrianopoulos G, Antonopoulou A, Athanassia S, Baziaka F, Charalambous A, Christodoulou S, Dimopoulou I, Floros I, Giannitsioti E, Gkanas P, Ioakeimidou A, Kanellakopoulou K, Karabela N, Karagianni V, Katsarolis I, Kontopithari G, Kopterides P, Koutelidakis I, Koutoukas P, Kranidioti H, Lignos M, Louis K, Lymberopoulou K, Mainas E, Marioli A, Massouras C, Mavrou I, Mpalla M, Michalia M, Mylona H, Mytas V, Papanikolaou I, Papanikolaou K, Patrani M, Perdios I, Plachouras D, Pistiki A, Protopapas K, Rigaki K, Sakka V, Sartzi M, Skouras V, Souli M, Spyridaki A, Strouvalis I, Tsaganos T, Zografos G, Mandragos K, Klouva-Molyvdas P, Maggina N, Giamarellou H, Armaganidis A, Giamarellos-Bourboulis EJ (2010) Early alterations of the innate and adaptive immune statuses in sepsis according to the type of underlying infection. Crit Care 14:R96
Hagström-Toft E, Enoksson S, Moberg E, Bolinder J, Arner P (1997) Absolute concentrations of glycerol and lactate in human skeletal muscle, adipose tissue, and blood. Am J Physiol 273:E584–E592
Large V, Arner P (1998) Regulation of lipolysis in humans. Pathophysiological modulation in obesity, diabetes, and hyperlipidaemia. Diabetes Metab 24:409–418
Plomgaard P, Fischer CP, Ibfelt T, Pedersen BK, van Hall G (2008) Tumor necrosis factor-alpha modulates human in vivo lipolysis. J Clin Endocrinol Metab 93:543–549
Lind L, Lithell H (1994) Impaired glucose and lipid metabolism seen in intensive care patients is related to severity of illness and survival. Clin Intensive Care 5:100–105
Volakli E, Spies C, Michalopoulos A, Groeneveld AB, Sakr Y, Vincent JL (2010) Infections of respiratory or abdominal origin in ICU patients: what are the differences? Critical Care 14:R32
Holub M, Klučková Z, Helcl M, Přihodov J, Rokyta R, Beran O (2003) Lymphocyte subset numbers depend on the bacterial origin of sepsis. Clin Microbiol Infect 9:202–211
Cavaillon JM, Adib-Conquy M (2010) Immune status in sepsis: the bug, the site of infection and the severity can make the difference. Crit Care 14:167
Boerma EC, Ince C (2010) The role of vasoactive agents in the resuscitation of microvascular perfusion and tissue oxygenation in critically ill patients. Intensive Care Med 36:2004–2018
Ospina-Tascon G, Neves AP, Occhipinti G, Donadello K, Buchele G, Simion D, Chierego ML, Silva TO, Fonseca A, Vincent JL, De Backer D (2010) Effects of fluids on microvascular perfusion in patients with severe sepsis. Intensive Care Med 36:949–955
Acknowledgments
The authors gratefully acknowledge the contribution to the completion of this study of the medical and nursing staff of the Second Department of Critical Care Medicine in “Attiko” University Hospital.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kopterides, P., Nikitas, N., Vassiliadi, D. et al. Microdialysis-assessed interstitium alterations during sepsis: relationship to stage, infection, and pathogen. Intensive Care Med 37, 1756–1764 (2011). https://doi.org/10.1007/s00134-011-2336-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-011-2336-8