Abstract
Objective
To determine if neurally adjusted ventilatory assist (NAVA) that delivers pressure in proportion to diaphragm electrical activity is as protective to acutely injured lungs (ALI) and non-pulmonary organs as volume controlled (VC), low tidal volume (Vt), high positive end-expiratory pressure (PEEP) ventilation.
Design
Prospective, randomized, laboratory animal study.
Subjects
Twenty-seven male New Zealand white rabbits.
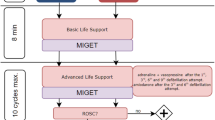
Interventions
Anesthetized rabbits with hydrochloric acid-induced ALI were randomized (n = 9 per group) to 5.5 h NAVA (non-paralyzed), VC (paralyzed; Vt 6-ml/kg), or VC (paralyzed; Vt 15-ml/kg). PEEP was adjusted to hemodynamic goals in NAVA and VC6-ml/kg, and was 1 cmH2O in VC15-ml/kg.
Measurements and main results
PaO2/FiO2; lung wet-to-dry ratio; lung histology; interleukin-8 (IL-8) concentrations in broncho-alveolar-lavage (BAL) fluid, plasma, and non-pulmonary organs; plasminogen activator inhibitor type-1 and tissue factor in BAL fluid and plasma; non-pulmonary organ apoptosis rate; creatinine clearance; echocardiography. PEEP was similar in NAVA and VC6-ml/kg. During NAVA, Vt was lower (3.1 ± 0.9 ml/kg), whereas PaO2/FiO2, respiratory rate, and PaCO2 were higher compared to VC6-ml/kg (p < 0.05 for all). Variables assessing ventilator-induced lung injury (VILI), IL-8 levels, non-pulmonary organ apoptosis rate, and kidney as well as cardiac performance were similar in NAVA compared to VC6-ml/kg. VILI and non-pulmonary organ dysfunction was attenuated in both groups compared to VC15-ml/kg.
Conclusions
In anesthetized rabbits with early experimental ALI, NAVA is as effective as VC6-ml/kg in preventing VILI, in attenuating excessive systemic and remote organ inflammation, and in preserving cardiac and kidney function.
Similar content being viewed by others
Introduction
Mechanical ventilation can cause ventilator-induced lung injury (VILI) [1–3] because of alveolar overdistension (volutrauma) and/or cyclic collapse/re-opening of lung units (atelectrauma). The implications of VILI are not simply limited to structural damage to the lungs, but also encompass the activation of systemic inflammatory cascades (biotrauma) [1, 3–5], which may be involved in propagating injury to non-pulmonary organs, potentially resulting in multiple organ failure [6–8]. A number of studies have demonstrated that ventilatory strategies that minimize VILI can decrease mortality in patients with acute lung injury (ALI) [9, 10]. However, these strategies have been criticized on the grounds that they only minimally tailor the mechanical ventilation to the individual patient. A ventilatory strategy that takes into account the inter-patient and temporal differences in pulmonary pathophysiology may further improve outcome.
Neurally adjusted ventilatory assist (NAVA) delivers pressure to the airways (Paw) proportional to inspiratory diaphragmatic electrical activity (EAdi) [11]; the proportionality factor is set on the ventilator by the clinician. The EAdi is influenced by facilitatory and inhibitory, dominantly vagally mediated feedback loops that integrate information from mechano- and chemo-receptors that “sense” the degree of lung stretch, as well as chemical stimuli [12–14]. The EAdi is reflexively up-regulated if the delivered tidal volume (Vt) is below the subject’s respiratory demand; down-regulation of EAdi occurs when assist is greater than the subject’s demand [12–16]. When the assist level with NAVA satisfies the subject’s respiratory demand, Vt remains virtually unchanged despite increases in the proportionality factor [12–16].
Hence, NAVA provides assist on a breath-by-breath basis in synchrony with and in proportion to respiratory demand. Studies in animals and humans demonstrate that NAVA prevents excessive lung distension, efficiently unloads respiratory muscles, and improves patient-ventilator synchrony [12, 13, 15–17].
To test the hypothesis that allowing the animals to “control” their intra-breath assist profile using NAVA would be at least as lung protective as a conventional low Vt strategy, we compared NAVA and two ventilation strategies, one known to be injurious (high Vt with low PEEP) and one known to be protective (low Vt with high PEEP), in an established ALI model.
Methods
The protocol was approved by the local Animal Care and Use Committee of St. Michael’s Hospital. For details see the online supplement.
Animal preparation
Thirty adult male New Zealand white rabbits (3.6–4.6 kg) were anesthetized, tracheotomized, and ventilated with a Servo 300 ventilator (Maquet Critical Care, Solna, Sweden) modified for NAVA. Intravenous anesthesia (ketamine hydrochloride 40 mg/kg/h; xylazine 4 mg/kg/h) and fluid (Ringer’s lactated solution; 5 ml/kg/h) administration remained constant throughout the experiment. Pulse oxymetry, heart rate, and arterial pressure were continuously monitored.
After induction of neuromuscular paralysis (pancuronium bromide 0.02 mg/kg), hydrochloric acid (pH 1.5) was instilled intratracheally with the rabbit in the lateral position (0.75 ml/kg each side), followed by a ventilation pause at Paw 25 cmH2O. The procedure was repeated after 5 min. Thirty minutes thereafter, the 27 animals that reached a predefined PaO2/FiO2 ratio of 80–200 (on FiO2 0.5) were randomized (n = 9 per group) to 5.5 h ventilation with one of the following strategies:
Experimental protocol
NAVA
No paralysis. NAVA was used as previously described [12, 15, 18]. Briefly, the EAdi derived from an array of electrodes on an esophageal catheter was processed, multiplied by a proportionality factor, and used to control inspiratory assist (Paw = EAdi × NAVA level) [19, 20]. A NAVA level of 0.5 cmH2O/unit EAdi was used throughout the study based on our previous findings using the same animal model [15].
VC6-ml/kg or 15-ml/kg
Continuous paralysis (pancuronium; 0.25 mg/kg/h). An additional dead space of 25 ml was used with VC15-ml/kg, and the ventilatory rate was adjusted to maintain PaCO2 between 35 and 45 mmHg at similar ventilatory rates in both VC groups.
PEEP was adjusted in NAVA and VC6-ml/kg, aiming to use the highest PEEP possible while maintaining mean arterial pressure (MAP) >60 mmHg. PEEP was lowered in 1 cmH2O steps if MAP decreased below 60 mmHg. Additional fluid was not administered. PEEP was 1 cmH2O in VC15-ml/kg. FiO2 was 0.5 and increased, if needed, to maintain SaO2 above 90%. Recruitment maneuvers and tracheal suctioning were not performed.
Measurements
Cardio-respiratory parameters were recorded every 30 min; arterial blood gases, lactate, and hemoglobin concentrations were measured hourly. Plasma was collected before ALI induction, 3 h thereafter, and at the end of the protocol. Broncho-alveolar lavage (BAL) fluid, and lung, heart, liver, small intestines, kidney, and spleen tissues were collected after killing the animals. Echocardiography was performed before ALI and hourly thereafter. Oxygen delivery, plasma creatinine clearance, and dynamic respiratory system compliance (CRSdyn) were calculated.
In plasma: interleukin 8 (IL-8), plasminogen activator inhibitor type-1 (PAI-1), tissue factor (TF), and creatinine. In lung tissue: wet-to-dry ratio, histological lung injury score, IL-8, PAI-1, and TF concentrations. In non-pulmonary organs: IL-8 levels and apoptosis rate.
Analysis of lung histology, of inflammatory and coagulation parameters, and of apoptosis in non-pulmonary organs was only performed in animals in which complete sets of material were available (VC15-ml/kg, n = 5; VC6-ml/kg, n = 7; NAVA, n = 7).
IL-8, PAI-1, TF (plasma, BAL), and lung wet-to-dry ratios were measured in four healthy control animals killed immediately after tracheotomy.
Data and statistical analysis
SigmaStatTM (3.10, Systat Software Inc., San Jose, CA) was used. Data are presented as mean ± SD or median (quartiles) as appropriate. Kolmogorov–Smirnov test was used to assess normal distribution of data. Differences among groups were analyzed using one-way analysis of variance (ANOVA). Repeated measurements were analyzed using either ANOVA on ranks (Friedman test) or two-way ANOVA with the ventilatory mode as the between-group factor and time after randomization as the repeated-measures factor. Holm-Sidak method was used for post-test comparison. Wilcoxon signed rank or t test was used to compare groups with paired data. Level of significance was p < 0.05.
Results
The protocol was completed in all except for three VC15-ml/kg animals that were killed when MAP decreased <60 mmHg after 4 h. For statistical purposes, the last available values were used in these animals.
The infusion rates of sedative drugs and fluids were equal in all groups. Hemodynamic parameters, arterial lactate and hemoglobin concentrations, and body temperature were not different among groups (Table 1). Arterial lactate concentrations remained unchanged in NAVA, whereas it progressively increased in both VC groups (p < 0.05 for NAVA vs. VC15-ml/kg).
Ventilatory pattern
Average Vt during NAVA was 2.7 ± 0.9 ml/kg [coefficient of variation (CV) 33%] during the initial 3 h and increased to 3.4 ± 0.8 ml/kg (p < 0.001; CV 23%) during the final 2.5 h (Fig. 1a). Early after ALI induction, the respiratory rate in NAVA was up to three times higher than the ventilatory rate in both VC groups, and thereafter decreased towards values in the VC6-ml/kg group (Fig. 1b). PEEP was decreased from 8.1 ± 2.0 to 4.2 ± 1.6 cmH2O in NAVA and from 7.0 ± 1.6 to 4.6 ± 1.2 cmH2O in VC6-ml/kg (p = n.s.; Fig. 1c).
Ventilatory pattern. PEEP levels, adjusted to maintain mean arterial pressure ≥60 mmHg in NAVA and VC6-ml/kg, were not different between NAVA and VC6-ml/kg. Ventilatory rate was higher in NAVA compared to both VC groups during the first 3 h, but was not different thereafter. Symbols represent group mean; error bars indicate standard deviation. t–g time–group interaction (two-way ANOVA). Post hoc pairwise comparison procedure between groups: † p < 0.05 NAVA versus VC6-ml/kg; ‡ p < 0.05 NAVA versus VC15-ml/kg; § p < 0.05 VC6-ml/kg versus VC15-ml/kg
Mean Paw during NAVA was lower compared to both VC6-ml/kg and VC15-ml/kg groups (p < 0.05 for both comparisons), while it was not different between VC6-ml/kg and VC15-ml/kg groups (Table 1). Early during NAVA, PaCO2 increased to 57 ± 7 mmHg; arterial pH decreased to 7.29 ± 0.04. Both variables remained unchanged throughout the study. PaCO2 was lower in VC6-ml/kg and VC15-ml/kg (p < 0.05 vs. NAVA; Table 1). At the end of the protocol, FiO2 was unchanged at 0.5 ± 0.0 in NAVA and was 0.6 ± 0.2 in VC6-ml/kg, whereas it was 0.9 ± 0.2 in VC15-ml/kg (p < 0.001 vs. NAVA and VC6-ml/kg).
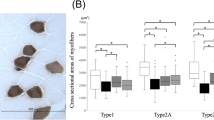
VILI
During the first hours after ALI, the PaO2/FiO2 ratio was higher during NAVA than during VC6-ml/kg, whereas no difference was observed later in the protocol (Fig. 2a). SaO2 remained >93% with NAVA and VC6-ml/kg, while it progressively decreased in VC15-ml/kg (Table 1) despite increasing FiO2. Lung wet-to-dry ratio was increased for both dependent and non-dependent regions of the right lower lobe in all groups compared to healthy controls. Wet-to-dry ratio during NAVA was lower for both dependent and non-dependent regions compared to VC15-ml/kg, whereas it was only lower for the dependent but not for the non-dependent lung with VC6-ml/kg compared to VC15-ml/kg (Fig. 2b). Thirty minutes after induction of ALI, CRSdyn had decreased by about 50% in all groups (p < 0.05 vs. before ALI for all groups). At the end of the protocol CRSdyn had recovered partially during NAVA, whereas it remained unchanged in VC6-ml/kg and VC15-ml/kg (Table 1).
Parameters indicating ventilation-induced lung injury (VILI). There were no differences in PaO2/FiO2 among groups before and 30 min after induction of ALI. The increase in PaO2/FiO2 early after switching to the assigned (i.e. before randomization into the treatment groups) ventilation mode was more pronounced in NAVA compared to VC6-ml/kg (p < 0.05 in post hoc analysis); however, there were no differences in PaO2/FiO2 between NAVA and VC6-ml/kg at the end of the protocol. With VC15-ml/kg, the PaO2/FiO2 remained below 200. All PaO2 values were measured at FiO2 0.5 and were corrected for body temperature. The lung wet-to-dry ratio in NAVA and in the VC6-ml/kg was lower compared to VC15-ml/kg (albeit not significantly for the dependent lung in VC6-ml/kg animals). Interleukin 8 (IL-8), tissue factor, and plasminogen activator inhibitor type 1 (PAI-1), and concentration in bronco-alveolar (BAL) fluid was higher in all study groups compared to healthy controls and was always higher in VC15-ml/kg compared to the other two groups (except for PAI-1 in VC6-ml/kg). Lung tissue IL-8 concentration was increased in all groups as compared to non-ventilated controls and was highest in the non-dependent lung regions of VC15-ml/kg. In the VC6-ml/kg and NAVA, lung tissue IL-8 concentration was lower compared to VC15-ml/kg (albeit not significant for the dependent lung region). Groups are shown as mean ± SD for a and b, or as median (quartiles) for c and d. Symbols and abbreviations are the same as in Fig. 1. ¶ p < 0.05 versus healthy control
Cumulative lung injury scores as well as average scores for each component were lower, albeit not always significantly so, in NAVA and VC6-ml/kg as compared to VC15-ml/kg (Table 2).
IL-8, tissue factor, and PAI-1 concentration
IL-8 concentrations in BAL and in lung tissue of the non-dependent lobe were lower in NAVA and VC6-ml/kg compared to VC15-ml/kg (p < 0.05). There was no difference in IL-8 tissue concentration between groups in the dependent regions. Tissue factor in BAL was lower during both NAVA and VC6-ml/kg, whereas PAI-1 concentration in BAL fluid was lower only during NAVA but not during VC6-ml/kg compared to VC15-ml/kg (Fig. 2c/d). Tissue factor and PAI-1 concentrations in lung tissue did not differ from non-ventilated controls.
Plasma IL-8 concentration was increased after 3 h in all groups and continued to increase at the end of the protocol in VC15-ml/kg, whereas it returned to pre-injury levels at the end of the protocol in both NAVA and VC6-ml/kg (Fig. 3a). Compared to VC15-ml/kg, IL-8 concentrations in the spleen and kidney were lower in NAVA but not in VC6-ml/kg. IL-8 concentration in the heart was lower in NAVA and VC6-ml/kg compared to VC15-ml/kg. No difference among groups was found for small intestines and liver (Fig. 3b). Plasma PAI-1 concentration remained elevated until the end of the protocol in both VC groups and tended to decrease in NAVA (Fig. 3c). Plasma tissue factor concentration did not differ from non-ventilated controls before induction of ALI and did not change over time in all groups.
Plasma and non-pulmonary organ IL-8 levels. Plasma PAI-1 levels. Plasma IL-8 concentration was similarly increased in all groups after 3 h and further increased in VC15-ml/kg, while returning to baseline values in VC6-ml/kg and NAVA at the end of the protocol. Tissue IL-8 concentration was highest in spleen, followed by kidney, heart, small intestines, and liver. While tissue IL-8 concentration was higher in VC15-ml/kg as compared to NAVA and VC6-ml/kg for all organs, the difference was not always statistically significant. Before induction of ALI, plasma levels of PAI-1 were not different from those of non-ventilated controls in all groups, and there was no difference among the study groups. PAI-1 concentrations in plasma were increased 3 h after induction of ALI in all groups and remained elevated until the end of the protocol in both VC groups, whereas it tended to decrease in NAVA. Groups are shown as median (quartiles). Symbols and abbreviations are the same as in Fig. 1. ¶ p < 0.05 versus healthy control. *p < 0.05 versus before induction of ALI
Parameters of non-pulmonary organ function
Cardiac output decreased from before ALI induction to the end of the protocol by 16 ± 23% in VC6-ml/kg and by 36 ± 11% in VC15-ml/kg (p < 0.05 vs. before induction of ALI for both), while the decrease in NAVA by 7 ± 16% was not significant (Table 1). Global DO2 decreased by 21 ± 24% during VC6-ml/kg, by 46 ± 17% during VC15-ml/kg, and by 17 ± 11% during NAVA (p < 0.05 vs. before ALI induction ALI for all). Urine output was higher in NAVA and VC6-ml/kg compared to VC15-ml/kg. Plasma creatinine clearance was higher in NAVA compared to VC15-ml/kg, while there was no difference between VC groups. Plasma concentrations for creatinine and urea nitrogen, urine osmolarity, transtubular gradient for potassium, and fractional excretion of sodium were not different among groups.
Apoptosis rate and histological alterations of non-pulmonary organs
The percentage of apoptotic cells was not different among groups for the heart, liver, and the crypts of the small intestines (Table 3). The kidney cortex had a higher percentage of apoptotic cells in VC6-ml/kg compared to VC15-ml/kg (p < 0.05). The villi of small intestines had a higher percentage of apoptotic cells in NAVA compared to VC15-ml/kg (p < 0.05).
Histological examination of the heart, kidney, liver, and small intestines of all animals revealed no relevant alterations of the tissue (specifically, no necrosis and intravascular thromboemboli).
Discussion
This is the first study to demonstrate that allowing anesthetized, spontaneously breathing animals with acute lung injury to “control” their ventilatory pattern in synchrony and proportional to their EAdi is at least as protective to the lungs and to non-pulmonary organs as a conventional, low Vt strategy [4, 6, 21, 22]. Similar to previous studies in rabbits with ALI [12, 15], animals in the present study “chose” tidal volumes with NAVA that were approximately half of those frequently described as lung protective in experimental studies exploring the pathophysiology of VILI [4, 6, 21, 22].
Our protocol was designed to compare assisted spontaneous breathing with conventional, lung protective ventilation in the absence of spontaneous breathing. The VC15-ml/kg group acted as a positive control demonstrating the increase in VILI with large Vt. Although a number of factors (i.e., level of anesthesia, fluid administration, PEEP, and FiO2) were controlled using the same protocols in both NAVA and VC6-ml/kg, we did not match the ventilatory patterns of NAVA and VC, as our hypothesis was that VILI would be minimized if animals “chose” their ventilatory pattern (i.e., Vt, intra-breath assist profile, ventilatory rate, including their variability) on a breath-by-breath basis.
Limitations
Based on our previous experience with the same model and to avoid a lengthy titration procedure, we used a single NAVA level [12, 15]. Using higher NAVA levels would have likely resulted in similar Vt and respiratory rates as we previously demonstrated that at higher NAVA levels Vt and respiratory rate reach a plateau due to progressive down-regulation of EAdi once a satisfactory level of respiratory muscle unloading is reached [13–16]. Of note, a uniform NAVA level does not necessarily result in a uniform ventilatory pattern, since the EAdi is continuously adjusted by vagally mediated feedback loops and behavioral inputs [12, 16].
We cannot exclude that the assist with the NAVA level we used was insufficient. However, in previous experiments using the same rabbit ALI model, we showed that the NAVA level used reduced the transdiaphragmatic pressure time product by more than 50% [15]. Although PaCO2 was elevated and pH was lower during NAVA compared to the VC groups, both parameters remained stable during NAVA, suggesting that there was no progression to respiratory failure due to inadequate low assist.
VC animals were paralyzed to ensure absence of spontaneous breathing and lung recruitment by tonic EAdi [12], a strategy frequently employed in animal research on VILI [6, 23], but used less often in clinical practice. Although unlikely, we cannot exclude the possibility that pancuronium affected the degree of VILI.
One has to be cautious when extrapolating from our short-term experimental ALI model performed under controlled laboratory conditions to much more complex clinical scenarios. Our model may only reflect the very first hours of an acute pulmonary insult such as aspiration of gastric content, but not the fundamentally different processes involved when ALI/ARDS results from an other cause.
Implications
Despite lower mean Paw and Vt with NAVA, we found that lung injury scores, lung wet-to-dry ratio, and lung and systemic biomarkers indicating VILI were similar to VC6-ml/kg, whereas other parameters (i.e., PaO2/FiO2 ratio, cardiac output, arterial lactate concentration, and CRSdyn) reflecting functional aspects of the cardiopulmonary system were less affected with NAVA compared to VC6-ml/kg. We cannot exclude that the seemingly lung protective effects of lower Paw and Vt on VILI might have been negated by the high respiratory rate with NAVA, while the positive effects of preserved diaphragmatic contraction on cardiopulmonary function were still detectable [24–27]. Our results are comparable to previous reports suggesting an association between preserved spontaneous breathing and better cardiac performance [27, 28].
The NAVA animals’ breathing pattern response can be explained by vagally controlled reflexes [12] and seems physiologically plausible [29–33]. The high respiratory rate in combination with a high variability in Vt (partially due to frequent sighs) early after ALI induction may have led to some intrinsic PEEP with lung recruitment. The initially higher PaO2/FiO2 ratio with NAVA compared to VC6-ml/kg despite similar levels of extrinsic PEEP would support this speculation. However, measurement of intrinsic PEEP under these conditions is very difficult, and the current study did not address this possibility.
The method of applying PEEP to a level that did not reduce mean arterial pressure below 60 mmHg in the present study differs from the approach normally used for ALI/ARDS. Our previous work has shown that ALI increases tonic EAdi and reduces phasic EAdi, while recruitment of the lungs with PEEP reduces tonic EAdi and restores phasic EAdi [12]. The approach used in the present study represents a compromise among suppressing tonic EAdi, promoting phasic EAdi, and preventing excessive hemodynamic side effects.
The NAVA group had higher PaCO2 levels than the VC groups. Previous studies have suggested that acute, hypercapnic respiratory acidosis may attenuate VILI and increase cardiac output [34–36]. Of note, our protocol did not specifically control PaCO2 in NAVA animals; PaCO2 levels resulted from the effect of the animals’ respiratory drive on the delivered Vt and minute ventilation. It was not the goal of the present study to ascertain which component (i.e., Vt, respiratory rate including their variability, and PaCO2) led to a decrease in VILI. Whether a lung protective VC strategy with even lower Vt and/or permissive hypercapnia, or whether different sedation levels in NAVA animals would have affected our measures of VILI remains speculative and requires further investigation.
Although there were few statistically significant differences between NAVA and VC6-ml/kg with regards to variables indicating VILI, the group’s average or median values as well as the variability (as evidenced by the group’s SD or the inter-quartile range) of most of these variables was consistently lower with NAVA compared to VC6-ml/kg. This is in accord with our hypothesis that NAVA tailors the ventilatory pattern to the specific physiology/biology of the subject.
The higher concentrations of biomarkers involved in coagulation (e.g., TF and PAI-1) in BAL fluid of VC15-ml/kg compared to NAVA and VC6-ml/kg, as well as increased plasma PAI-1 levels early after induction of ALI are compatible with previous studies [37, 38]. Nevertheless, the significance of these findings is unclear. We were unable to detect histological evidence of increased intravascular coagulation in any non-pulmonary organ.
Our data support previous studies with respect to the development of biotrauma [5, 6, 10]. There was a profound increase in plasma IL-8 levels as well as in tissue IL-8 concentration in spleen, kidney, and heart, but not in the liver and small intestines. Whether spill-over from the lungs and/or local production accounts for the IL-8 concentrations in tissue of non-pulmonary organs remains unclear. Although IL-8 concentrations may indicate the extent of a pro-inflammatory response in the various compartments and organs studied, a causal relationship between VILI, plasma, or local IL-8 concentrations, and non-pulmonary organ injury cannot be determined from our data.
In our model, kidney function was impaired with VC15-ml/kg and, consistent with the lowest tissue IL-8 levels, was best preserved with NAVA. How an injurious ventilation strategy ultimately translates into dysfunction of non-pulmonary organs is not fully understood. Kidneys are very susceptible to blood flow restriction. Even small decreases in renal blood flow as well as blood flow redistribution within the kidneys can affect kidney function [39, 40]. In the present study, we suggest that combined effects of impaired perfusion and oxygen delivery to the kidneys along with upregulation of a systemic and local inflammatory response accounted for the more pronounced reduction in kidney function in the injuriously ventilated animals.
Our results are different from those we observed in a previous study in which an injurious ventilatory strategy led to epithelial cell apoptosis in non-pulmonary organs such as the kidney [6]. We are unsure of the exact reason(s) for the difference in results, but it may be related to differences in length of the experiments and/or severity of injury in the two studies. In the study by Imai et al. the animals were ventilated for 8 h prior to sacrifice, compared to 5.5 h or less in the present study. In addition, the PaO2/FiO2 ratio in the high Vt group was less than 100 in the Imai study and 100–200 in the present study. Finally, BAL levels of IL-8 in the study by Imai et al. were about 40 times greater than in the present study. Of note, the assay used does not definitively allow discrimination between apoptotic and necrotic cells.
Conclusions
We present evidence suggesting that allowing animals with lung injury to choose their respiratory pattern is at least as effective in preventing various manifestations of VILI as conventional, volume-controlled ventilation using a Vt of 6-ml/kg in an experimental model of early ARDS. Both strategies similarly prevent VILI, attenuate excessive systemic as well as extra-pulmonary organ inflammation and injury, and preserve cardiac and kidney function.
References
Dreyfuss D, Saumon G (1998) Ventilator-induced lung injury: lessons from experimental studies. Am J Respir Crit Care Med 157:294–323
Slutsky AS (1999) Lung injury caused by mechanical ventilation. Chest 116:9S–15S
dos Santos CC, Slutsky AS (2006) The contribution of biophysical lung injury to the development of biotrauma. Annu Rev Physiol 68:585–618
Tremblay L, Valenza F, Ribeiro SP, Li J, Slutsky AS (1997) Injurious ventilatory strategies increase cytokines and c-fos m-RNA expression in an isolated rat lung model. J Clin Invest 99:944–952
Ranieri VM, Suter PM, Tortorella C, De Tullio R, Dayer JM, Brienza A, Bruno F, Slutsky AS (1999) Effect of mechanical ventilation on inflammatory mediators in patients with acute respiratory distress syndrome: a randomized controlled trial. JAMA 282:54–61
Imai Y, Parodo J, Kajikawa O, de Perrot M, Fischer S, Edwards V, Cutz E, Liu M, Keshavjee S, Martin TR, Marshall JC, Ranieri VM, Slutsky AS (2003) Injurious mechanical ventilation and end-organ epithelial cell apoptosis and organ dysfunction in an experimental model of acute respiratory distress syndrome. JAMA 289:2104–2112
Ranieri VM, Giunta F, Suter PM, Slutsky AS (2000) Mechanical ventilation as a mediator of multisystem organ failure in acute respiratory distress syndrome. JAMA 284:43–44
Slutsky AS, Tremblay LN (1998) Multiple system organ failure. Is mechanical ventilation a contributing factor? Am J Respir Crit Care Med 157:1721–1725
Amato MB, Barbas CS, Medeiros DM, Magaldi RB, Schettino GP, Lorenzi-Filho G, Kairalla RA, Deheinzelin D, Munoz C, Oliveira R, Takagaki TY, Carvalho CR (1998) Effect of a protective-ventilation strategy on mortality in the acute respiratory distress syndrome. N Engl J Med 338:347–354
The Acute Respiratory Distress Syndrome Network (2000) Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med 342:1301–1308
Sinderby C, Navalesi P, Beck J, Skrobik Y, Comtois N, Friberg S, Gottfried SB, Lindstrom L (1999) Neural control of mechanical ventilation in respiratory failure. Nat Med 5:1433–1436
Allo JC, Beck JC, Brander L, Brunet F, Slutsky AS, Sinderby CA (2006) Influence of neurally adjusted ventilatory assist and positive end-expiratory pressure on breathing pattern in rabbits with acute lung injury. Crit Care Med 34:2997–3004
Brander L, Leong-Poi H, Beck J, Brunet F, Hutchison SJ, Slutsky AS, Sinderby C (2008) Titration and implementation of neurally adjusted ventilatory assist in critically Ill patients. Chest 135:695–703
Lecomte F, Brander L, Jalde F, Beck J, Qui H, Elie C, Slutsky AS, Brunet F, Sinderby C (2009) Physiological response to increasing levels of neurally adjusted ventilatory assist (NAVA). Respir Physiol Neurobiol 166(2):117–124
Beck J, Campoccia F, Allo JC, Brander L, Brunet F, Slutsky AS, Sinderby C (2007) Improved synchrony and respiratory unloading by neurally adjusted ventilatory assist (NAVA) in lung-injured rabbits. Pediatr Res 61:289–294
Sinderby C, Beck J, Spahija J, de MM, Lacroix J, Navalesi P, Slutsky AS (2007) Inspiratory muscle unloading by neurally adjusted ventilatory assist during maximal inspiratory efforts in healthy subjects. Chest 131:711–717
Colombo D, Cammarota G, Bergamaschi V, De LM, Corte FD, Navalesi P (2008) Physiologic response to varying levels of pressure support and neurally adjusted ventilatory assist in patients with acute respiratory failure. Intensive Care Med 34:2010–2018
Spahija J, Beck J, de Marchie M, Comtois A, Sinderby C (2005) Closed-loop control of respiratory drive using pressure-support ventilation: target drive ventilation. Am J Respir Crit Care Med 171:1009–1014
Beck J, Tucci M, Emeriaud G, Lacroix J, Sinderby C (2004) Prolonged neural expiratory time induced by mechanical ventilation in infants. Pediatr Res 55:747–754
Sinderby C, Spahija J, Beck J (2001) Changes in respiratory effort sensation over time are linked to the frequency content of diaphragm electrical activity. Am J Respir Crit Care Med 163:905–910
Crimi E, Zhang H, Han RN, Del Sorbo L, Ranieri VM, Slutsky AS (2006) Ischemia and reperfusion increases susceptibility to ventilator-induced lung injury in rats. Am J Respir Crit Care Med 174:178–186
Hirsch J, Hansen KC, Sapru A, Frank JA, Chalkley RJ, Fang X, Trinidad JC, Baker P, Burlingame AL, Matthay MA (2007) Impact of low and high tidal volumes on the rat alveolar epithelial type II cell proteome. Am J Respir Crit Care Med 175:1006–1013
Frank JA, Gutierrez JA, Jones KD, Allen L, Dobbs L, Matthay MA (2002) Low tidal volume reduces epithelial and endothelial injury in acid-injured rat lungs. Am J Respir Crit Care Med 165:242–249
Froese AB, Bryan AC (1974) Effects of anesthesia and paralysis on diaphragmatic mechanics in man. Anesthesiology 41:242–255
Neumann P, Wrigge H, Zinserling J, Hinz J, Maripuu E, Andersson LG, Putensen C, Hedenstierna G (2005) Spontaneous breathing affects the spatial ventilation and perfusion distribution during mechanical ventilatory support. Crit Care Med 33:1090–1095
Putensen C, Rasanen J, Lopez FA (1994) Ventilation-perfusion distributions during mechanical ventilation with superimposed spontaneous breathing in canine lung injury. Am J Respir Crit Care Med 150:101–108
Putensen C, Mutz NJ, Putensen-Himmer G, Zinserling J (1999) Spontaneous breathing during ventilatory support improves ventilation-perfusion distributions in patients with acute respiratory distress syndrome. Am J Respir Crit Care Med 159:1241–1248
Putensen C, Zech S, Wrigge H, Zinserling J, Stuber F, von Spiegel T, Mutz N (2001) Long-term effects of spontaneous breathing during ventilatory support in patients with acute lung injury. Am J Respir Crit Care Med 164:43–49
Gunawardena S, Ravi K, Longhurst JC, Kaufman MP, Ma A, Bravo M, Kappagoda CT (2002) Responses of C fiber afferents of the rabbit airways and lungs to changes in extra-vascular fluid volume. Respir Physiol Neurobiol 132:239–251
Ma A, Bravo M, Kappagoda CT (2003) Responses of bronchial C-fiber afferents of the rabbit to changes in lung compliance. Respir Physiol Neurobiol 138:155–163
Trippenbach T, Kelly G, Marlot D (1985) Effects of tonic vagal input on breathing pattern in newborn rabbits. J Appl Physiol 59:223–228
Tsubone H (1986) Characteristics of vagal afferent activity in rats: three types of pulmonary receptors responding to collapse, inflation, and deflation of the lung. Exp Neurol 92:541–552
Wang AL, Blackford TL, Lee LY (1996) Vagal bronchopulmonary C-fibers and acute ventilatory response to inhaled irritants. Respir Physiol 104:231–239
Broccard AF, Hotchkiss JR, Vannay C, Markert M, Sauty A, Feihl F, Schaller MD (2001) Protective effects of hypercapnic acidosis on ventilator-induced lung injury. Am J Respir Crit Care Med 164:802–806
Kregenow DA, Rubenfeld GD, Hudson LD, Swenson ER (2006) Hypercapnic acidosis and mortality in acute lung injury. Crit Care Med 34:1–7
Sinclair SE, Kregenow DA, Lamm WJ, Starr IR, Chi EY, Hlastala MP (2002) Hypercapnic acidosis is protective in an in vivo model of ventilator-induced lung injury. Am J Respir Crit Care Med 166:403–408
Dahlem P, Bos AP, Haitsma JJ, Schultz MJ, Meijers JC, Lachmann B (2005) Alveolar fibrinolytic capacity suppressed by injurious mechanical ventilation. Intensive Care Med 31:724–732
Dahlem P, Bos AP, Haitsma JJ, Schultz MJ, Wolthuis EK, Meijers JC, Lachmann B (2006) Mechanical ventilation affects alveolar fibrinolysis in LPS-induced lung injury. Eur Respir J 28:992–998
Hall SV, Johnson EE, Hedley-Whyte J (1974) Renal hemodynamics and function with continuous positive-pressure ventilation in dogs. Anesthesiology 41:452–461
Moore ES, Galvez MB, Paton JB, Fisher DE, Behrman RE (1974) Effects of positive pressure ventilation on intrarenal blood flow in infant primates. Pediatr Res 8:792–796
Acknowledgments
We are indebted to Norman Comtois for his excellent technical assistance, to Jenna Ekborn for her invaluable help, and to the staff of the research vivarium at St. Michael’s Hospital, Toronto, for their support. The study was supported in part by the Canadian Institutes of Health Research (CIHR), the Ontario Thoracic Society (OTS), and the R. Samuel McLaughlin Foundation. Lukas Brander held postdoctoral fellowships from the Swiss National Science Foundation (SNF)/Swiss Foundation for Fellowships in Medicine and Biology (SSMBS) provided by Novartis AG (grant no. 1130) and from the Division of Respirology at the University of Toronto provided by Merck-Frosst. Marcus Schultz is supported by The Netherlands Organization for Health Research and Development (ZonMW), NWO-VENI grant 2004 (project no. 016.056.001).
Author information
Authors and Affiliations
Corresponding author
Additional information
The Department of Intensive Care Medicine at the University Hospital Bern has a research and development collaboration contract with Maquet Critical Care AB. None of the authors received any personal financial gain from this collaboration. Dr. Sinderby and Dr. Beck have made inventions related to neural control of mechanical ventilation that are patented. The license for these patents belongs to Maquet Critical Care. Future commercial uses of this technology may provide financial benefit to Dr. Sinderby and Dr. Beck through royalties. Dr. Sinderby and Dr. Beck each own 50% of Neurovent Research, Inc. Neurovent Research is a research and development company that builds the equipment and catheters for research studies. Neurovent Research has a consulting agreement with Maquet Critical Care. Dr. Slutsky consults for Maquet Critical Care, and is compensated for these consultations. The remaining authors have not disclosed any potential conflict of interest with the subject of the present manuscript.
The work was performed at St. Michael’s Hospital and the University of Toronto, Toronto, Canada.
This article is discussed in the editorial available at: doi:10.1007/s00134-009-1632-z.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Brander, L., Sinderby, C., Lecomte, F. et al. Neurally adjusted ventilatory assist decreases ventilator-induced lung injury and non-pulmonary organ dysfunction in rabbits with acute lung injury. Intensive Care Med 35, 1979–1989 (2009). https://doi.org/10.1007/s00134-009-1626-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-009-1626-x