Abstract
Purpose
To compare patients’ psychological distress and memories from intensive care unit (ICU) treatment 4–6 weeks after ICU discharge with expectations of their relatives. Further, to explore the relationship between personality traits and ICU memories with psychological distress.
Methods
A cross-sectional study of 255 patients and 298 relatives. The questionnaire included: hospital anxiety and depression scale (HADS), impact of event scale (IES), life orientation test, ICU memory tool and memory of ICU; technical procedures, pain, lack of control and inability to express needs. Relatives were assessed for their expectations of the patients’ memories and psychological distress.
Results
Twenty-five percent of the patients reported severe posttraumatic stress symptoms, IES-total ≥ 35. The levels of anxiety and depression were significantly higher than in the general population, mean anxiety was 5.6 versus 4.2 (p < 0.001), and mean depression was 4.8 versus 3.5 (p < 0.001). Relatives expected more psychological distress and the relatives thought the patient was less able to express needs than the patients reported (p < 0.001). Higher age, unemployment, respirator treatment, pessimism, memory of pain, lack of control and inability to express needs were independent predictors of posttraumatic stress symptoms (p < 0.01).
Conclusions
Psychological distress symptoms were frequent among ICU survivors. Relatives expected the patients to be more distressed after ICU treatment than the patients reported. The strongest predictors of posttraumatic stress symptoms from the ICU were memoris about pain, lack of control and inability to express needs. Pessimism may be a reason for psychological distress and should be addressed during follow up, as pessimistic patients may need more motivation and support.
Similar content being viewed by others
Introduction
Patients suffer from psychological distress during and following an ICU stay [1–4] and about 15% develop posttraumatic stress disorder (PTSD) [5–7], a serious psychiatric disorder that follows the experience of a traumatic event and causes significant impairment in daily life. Studies have also shown that relatives may suffer from substantial psychological distress during and following the patient's ICU treatment [8, 9]. There may be several reasons for relatives’ psychological distress. They experience a real threat of death of a close person and they may suffer from the idea that the patient has pain and discomfort. The ICU environment may be very frightening due to equipment, noises and personnel, and relatives may have substantial worries about the future. We wanted to focus on how relatives expect the patient to experience the ICU treatment and found no recent studies that have explored this phenomenon [10].
Several predictors for the development of PTSD-related symptoms in medical-ICU patients have been identified, including longer hospital and ICU stay, longer duration of mechanical ventilation (MV), greater levels of sedation, female gender, younger age, pre-existing psychiatric history, delusional memories and greater number of traumatic memories [11–13]. However, the literature is not consistent according to memories, as others have found fewer PTSD-related symptoms with the presence of factual recall [14].
Knowledge is limited on how other ICU experiences, such as awareness during painful procedures, difficulties in expressing one’s needs and lack of control, influence patients’ PTSD-related symptoms. Optimistic patients differ from pessimists in coping with serious disease; they recover more rapidly, have less psychological distress and have a better quality of life [15, 16]. We are not aware of previous studies that have investigated the association between patient’s personality traits (optimism/pessimism) and psychological distress after ICU treatment.
The primary aims of this study were to assess patients’ ICU memories and psychological distress 4–6 weeks after ICU discharge compared with the relatives’ expectations and to study personality traits and ICU memories as possible predictors of psychological distress symptoms.
A secondary aim was to explore demographic and clinical patient characteristics related to different kinds of memories.
Methods
Oslo University Hospital, Ulleval, is an academic, tertiary-care centre with an 11-bed general ICU, a six-bed medical-ICU and a coronary unit with three beds for mechanically ventilated coronary patients. The ICUs have no fixed time for visits or telephone calls. During the patient’s stay, one physician and one team of nurses are assigned to the patient. Physical restraint is not used. During MV, the patients are treated with sedatives and analgesics. The simplified acute physiology score 2 (SAPS-2) [17] and the nine equivalents of nursing manpower use score (NEMS) [18] were used to characterise the patient population and nurses’ work load. The patients were divided into three main diagnostic groups: medical, surgical and trauma. In addition it was noted if the patients had a minor/moderate head injury/disease.
In this prospective study patients and relatives were consecutively invited to participate by completing a questionnaire. For patients who remained at the hospital, written information, consent letter and a questionnaire were sent by mail to the rehabilitation hospital or sent home to the patients about 4 weeks after ICU discharge. For those transferred to other hospital ICUs, a questionnaire was sent after about 6 weeks. We assumed that at this time they were able to read the information letter and decide whether they wanted to participate or not.
The relatives, one per patient, were asked to participate in this study. The staff chose the closest relative for each patient. If they accepted, they received written information about the study during the ICU period and signed a consent letter. Four weeks after ICU discharge a questionnaire was mailed. Patients’ and relatives’ answers were not anonymous. One reminder letter was sent if necessary. The Norwegian Data Inspectorate and The Regional Ethics Committee approved the study.
Inclusion and exclusion criteria
Patients 18–75 years who had stayed at least 24 h in the ICU were included. Patients with language difficulties, serious psychiatric problems, severe head injury (not capable of completing a questionnaire 4–6 weeks after injury) or cognitive failure were excluded (Fig. 1). Relatives 18 years or older were eligible. Relatives unable to understand and read Norwegian (n = 44), or who for other reasons, i.e., medical/alcohol abuse (n = 2), cognitive impairment (n = 1) were incapable of completing the questionnaire were excluded.
Assessments
Patients and relatives questionnaire about memory and psychological distress
We asked the patients if they had memories about technical procedures (equipment, ventilator, venipuncture, invasive procedures and medical examinations) and how they remembered these procedures. Four items about psychological distress (anxiety, depression, insomnia, concentration problems) constructed in an earlier study were also used [8, 19]. These 13 questions, given to patients and relatives, were analysed in a factor analysis revealing three factors: (1) memory for technical procedures, (2) frightening memories and (3) psychological distress. Additional detail regarding these questions is provided in the online supplement.
The patients and relatives also received questions about memories of pain, to what degree lack of control was distressing and if they felt unable to express needs. Response options were rated on a 5-point-Likert-scale from 0 (not at all) to 4 (to a very high degree). We asked the relatives to answer in the way they expected the patient would answer.
Patient questionnaire
The hospital anxiety and depression scale (HADS) [20] is a reliable and valid instrument for assessing anxiety and depression in medical patients [21]. The questionnaire consists of 14 items, seven for anxiety and seven for depression. Each item is scored from 0 to 3, with a maximum score of 21 on each of the HADS subscales. For severe disorder, most probably in need of treatment, a cut-off level >11 for both subscales is used. Normative data from the general Norwegian population on HADS are available from the Nord-Trøndelag Health Study (HUNT-2) [22]. In the analyses, these data are gender and age adjusted to fit our patient population.
The impact of event scale (IES) is found to be a useful measure of stress reactions after a range of traumatic events and is valuable for detecting individuals who require treatment [23]. The IES has two subscales (seven items on intrusion and eight items on avoidance) [24]. In the Norwegian translation, each item is scored on a 6-point-Likert-scale rated from 0 to 5, with a total range from 0 to 75. Higher scores indicate more severe PTSD-related symptoms. A score above 35 indicates severe symptoms with high probability for diagnosing PTSD [25].
The revised life orientation test (LOT) is a scale measuring dispositional optimism versus degree of pessimism reflecting generalized outcome expectancies [26]. The dispositional perspective is based on the idea that people have relatively stable qualities. The LOT score was used previously among cancer patients in Norway and was found to be stable over time [27]. Ten items compose the revised LOT; four of the items are filler items and are not used in the scoring. The six remaining items are summed to compute an overall personality trait score, which can range from 0 to 24, where a high score indicates optimism.
The ICU memory tool [28] has been used in previous studies [29–31] to measure various aspects of memory after intensive care in an interview situation. Although created for an interview situation, the tool has also been used as a self-administered questionnaire [12, 31, 32]. It consists of items about amnesia on admission to hospital and amnesia for the ICU stay. Memories from ICU stay are divided into having (a) memories of feelings (being uncomfortable, feeling confused, feeling down, feeling anxious/frightened, panic, pain), (b) delusional memories (feeling that people were trying to hurt them, hallucination, nightmares, dreams) and, (c) factual recall (family, alarms, voices, lights, faces, breathing tube, suctioning, darkness, clock, tube in the nose, and ward round).
Statistical methods
Statistical analyses were performed with SPSS for Windows Version 15.0. Continuous variables are presented as mean scores with 95% CI. The significance level was set at p < 0.05. Independent sample t-tests and paired sample t-tests were used when comparing two groups on normally distributed variables. Our decision regarding choice of t-test or Wilcoxon–Mann–Whitney-test was based on results from a recent statistical publication [33]. For categorical variables Pearson’s Chi-square test was used. Correlations between pairs of continuous variables were calculated using Spearman’s correlation coefficients. When the aim was to identify variables independently and significantly associated with IES, HADS anxiety or HADS depression, linear regression analysis was used. In these analyses we also adjusted for patient characteristics (age, gender, employment status, respirator treatment). Variables that were associated with the dependent variable in the univariate analyses (p < 0.2) were included in a multivariate linear regression model, using backward stepwise variable selection.
Results
During the study period, from February 2005 to December 2006, 810 patients, age 18–75, were admitted and had an ICU stay of at least 24 h. The mortality among these was 14.1% (n = 114). Among the 482 eligible patients discharged from the ICU 14.3% (69) died within 6 weeks. A total of 255 (61.7%) completed the questionnaire (Fig. 1). A total of 298 (83%) recruited relatives of survivors answered the questionnaire. The relatives’ mean age was 50.3 years (12.2 SD) and 69% female. The relatives’ relationship to the patient was spouse/cohabitant (49%), child (29%), parent (13%), sibling (7%) or other relative/close person (2%). We received answers from 134 pairs of patients and relatives. Some patients had no relative or the relative refused to participate. Among relatives, some patients were not included due to impaired recovery (Table 1).
Comparison of patients and relatives with regards to memory and psychological distress
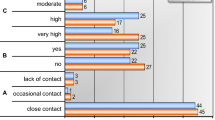
In the analysis with pairs of patients and relatives (n = 134), the relatives expected significantly more psychological distress and thought the patient was less able to express needs than the patient reported (Fig. 2). In pairs of patients and relatives no differences were seen in memory of frightening experiences, memory of technical procedures or lack of control. When comparing mean scores of all patients and relatives, similar results as with pairs of patients and relatives were found, except that the relatives expected memory of technical procedures to be more frightening than the patients reported (2.5 vs. 2.2, p < 0.001).
Level of PTSD-related symptoms, anxiety and depression symptoms
The mean score for the IES-total after ICU stay was 22.6 (95% CI 20.5–24.6), and 26.9% (64 of 238) of the patients had high scores, i.e., above the cut-off value IES-total >35. Compared with the general Norwegian population from the HUNT-2 study [22], our ICU survivors had significantly more anxiety and depression symptoms 4 weeks after ICU discharge. HADS-anxiety in the patients was 5.6 (95% CI: 5.1–6.2) versus population 4.2 (4.1–4.3), p < 0.001, and HADS-depression in the patients was 4.8 (4.2–5.3) versus population 3.5 (3.4–3.6), p < 0.001 (HUNT data age and gender adjusted to fit our data). For HADS-anxiety 15% of the patients (37/250) had high scores (>11) and 12% (29/252) >11 for HADS-depression.
Predictive factors for PTSD-related symptoms, anxiety and depression symptoms
In the univariate analysis variables found to be significantly associated with IES-total, HADS-anxiety and HADS-depression are presented in Table 2. The multivariate analyses identified several statistically significant independent variables explaining the variance of IES, HADS-anxiety and HADS-depression symptom levels, respectively. The IES-total increased significantly with higher age, unemployment, respirator treatment, lower LOT scores, more pain memories, less control and less ability to express needs. HADS-anxiety increased significantly with lower employment status, lower LOT scores, more pain memories, less control and less ability to express needs. HADS-depression increased significantly with lower employment status, lower LOT scores, less ability to express needs and lower educational status.
Personality trait
The LOT mean score was 15.7 (95% CI 15.1–16.3). Personality trait (pessimism/optimism) was found to be a strong independent variable, as pessimism predicted more PTSD-related symptoms, anxiety and depression (all p < 0.001). Thus, personality trait was not associated with age or gender. High level of education was correlated positively with optimism (r = 0.20, p = 0.002), and patients being unemployed had significantly lower personality trait scores (13.5 vs. 16.4, p < 0.001), whereas personality trait was not associated with severity of illness (head injury, trauma, medical/surgical, MV, MV duration, LOS ICU, SAPS, NEMS).
Patient characteristics related to memories from the ICU
To simplify comparison with earlier publications using the ICU memory tool, patients were divided into those with no memory of events and those with memory, and we further compared this with patient characteristics (Tables 3, 4). There were no significant differences in memory according to demographic variables (sex, age, educational level, employment status). Memories of feelings occurred in 56% of the patients. Patients transferred to local hospitals or patients with head injury had significantly less memory of feelings than patients not transferred or without head injury.
Significantly fewer patients on mechanical ventilation (MV) had factual recall, memory before and during ICU stay, but significantly more patients had delusional memories compared to patients without MV. Among trauma patients, significantly fewer patients had factual recall, memory before and during stay, but not significantly different delusional memories compared to patients without trauma. Higher SAPS and NEMS were seen in patients with no factual recall or no memory before/during ICU stay compared to patients with such memories.
Patients with delusional memories (46%) had longer duration of MV than patients without delusional memories. However, longer duration of MV was not associated with more factual recall, memory before or memory during ICU stay.
Discussion
This cross-sectional study is the first to show that relatives expected more psychological distress after ICU treatment than the patients reported. Further, it shows that the ICU survivors’ psychological distress is associated with a pessimistic personality trait.
The relatives’ overestimation of psychological distress may be due to the substantial distress they experience. However, the relatives did not overestimate the memory of pain or the distress regarding lack of control. Impaired communication between relative and patient may feel worse for the relative than the patient. The effort made by the staff to assure the relatives that the treatment for pain and sleeplessness was good may be one reason for the relatives’ accurate expectancy on this point. Knowledge of the relatives’ reactions during ICU stay is important, since many relatives suffer from substantial psychological distress following the patient’s ICU treatment [8, 9]. Information and communication about the patient’s condition may reduce relatives’ thoughts about the suffering patient and thus reduce the relatives’ psychological distress. The results of this study enhance the knowledge to help relatives in such difficult situations.
To our knowledge this study is the first to show that personality traits are strongly associated with psychological distress symptoms after trauma or critical illness in ICU patients, as optimistic patients have significantly less anxiety, depression and PTSD-related symptoms post-ICU discharge. Consequently the ICU staff should therefore be more attentive to the patients’ personality traits in order to alleviate their strain. We propose that the development of psychological distress may be related to patient pessimism. However, stability of personality trait (optimism/pessimism) in ICU survivors has not been established.
We found, like others, that the level of psychological distress among ICU patients post-ICU discharge was high [2, 5, 11, 14]. The ICU survivors’ mean value for anxiety is 30% above the population mean value and with an assumption that 5% of the population was >11 versus 15% among the ICU survivors, we consider this to be clinically significant. The need for psychological intervention is significant, as a large proportion of the patients (26.9%) had severe PTSD-related symptoms; future studies should address whether new supportive routines may help reduce these symptoms. We have no reasonable explanation for the discrepancy in finding that higher age was a predictor for PTSD-related symptoms rather than younger age reported previously [11]. Unemployed patients may perceive less social support, which is found to be associated with PTSD-symptoms [34], and unemployment have been associated with more psychological problems [35].
In accordance with previous studies, two-thirds of the patients had memories of the ICU stay and half of the patients had experienced delusional memories [4, 29, 32, 36]. Patients with more serious conditions remembered less, both before and during the ICU stay. The proportion of patients with delusional memories among severely ill patients did not differ from patients with less serious conditions, which supports other studies [37, 38]. However, other studies have found that patients with severe organ failure have more delusional memories [32].
Some studies report that factual recall protects against developing posttraumatic stress symptoms in patients with delusional memories [6, 14], while our study, as well as other studies, did not [39, 40]. This study found that delusional memories, factual recall and memory of feelings were all positively associated with psychological distress symptoms. Amnesia for the time in hospital before ICU admission has been positively associated with the level of PTSD-related symptoms [12, 14]. However, no such association was found in our patients.
Strengths and limitations
The questionnaire was competed by 255 (62%) of the ICU patients, which is an acceptable number, and a high proportion of relatives (83%) participated. A limitation in our study is that we used a self-administered questionnaire with no possibility of clarifying questions if there was any confusion. The IES and HADS are screening tools rather than diagnostic tools and provide information only about symptom levels. The associations described may be confounded by variables that are not measured, and as in any multiple regression models, used to identify risk factors; this procedure may produce biased coefficients. We did not measure somatic or psychological disease prior to the ICU stay nor delirium during ICU stay, which may influence the level of psychological distress symptoms after trauma. Neither did we measure use of hypnotic and analgesic drugs during the ICU stay, which may influence both the retention of memory and the level of psychological distress. These measurements would have been incomplete, due to the single centre study design, as half of our patients were transferred to other hospitals. However, we asked the patients if they had more anxiety, depression, insomnia and concentration problems after the ICU stay than before.
Conclusion
Even though psychological distress symptoms were frequent, relatives overestimated the patients’ psychological distress and expected them to be more distressed during intensive treatment than the patients reported. Information about this may reduce relatives’ worries. Important predictors for developing PTSD-related symptoms were memory of pain, lack of control, inability to express needs, pessimism, respirator treatment, employment status and age. Improved communication may help patients to express their needs, treat pain and enhance their feelings of control. Pessimism may be a reason for psychological distress and should be addressed during follow up.
References
Szokol JW, Vender JS (2001) Anxiety, delirium, and pain in the intensive care unit. Crit Care Clin 17:821–842
Scragg P, Jones A, Fauvel N (2001) Psychological problems following ICU treatment. Anaesthesia 56:9–14
Jones C, Backman C, Capuzzo M, Flaatten H, Rylander C, Griffiths RD (2007) Precipitants of post-traumatic stress disorder following intensive care: a hypothesis generating study of diversity in care. Intensive Care Med 33:978–985
Jones C, Skirrow P, Griffiths RD, Humphris GH, Ingleby S, Eddleston J, Waldmann C, Gager M (2003) Rehabilitation after critical illness: a randomized, controlled trial. Crit Care Med 31:2456–2461
Cuthbertson BH, Hull A, Strachan M, Scott J (2004) Post-traumatic stress disorder after critical illness requiring general intensive care. Intensive Care Med 30:450–455
Capuzzo M, Valpondi V, Cingolani E, Gianstefani G, De LS, Grassi L, Alvisi R (2005) Post-traumatic stress disorder-related symptoms after intensive care. Minerva Anestesiol 71:167–179
Schelling G, Stoll C, Haller M, Briegel J, Manert W, Hummel T, Lenhart A, Heyduck M, Polasek J, Meier M, Preuss U, Bullinger M, Schuffel W, Peter K (1998) Health-related quality of life and posttraumatic stress disorder in survivors of the acute respiratory distress syndrome. Crit Care Med 26:651–659
Myhren H, Ekeberg O, Langen I, Stokland O (2004) Emotional strain, communication, and satisfaction of family members in the intensive care unit compared with expectations of the medical staff: experiences from a Norwegian University Hospital. Intensive Care Med 30:1791–1798
Azoulay E, Pochard F, Kentish-Barnes N, Chevret S, Aboab J, Adrie C, Annane D, Bleichner G, Bollaert PE, Darmon M, Fassier T, Galliot R, Garrouste-Org, Goulenok C, Goldgran-Toledano D, Hayon J, Jourdain M, Kaidomar M, Laplace C, Larche J, Liotier J, Papazian L, Poisson C, Reignier J, Saidi F, Schlemmer B (2005) Risk of post-traumatic stress symptoms in family members of intensive care unit patients. Am J Respir Crit Care Med 171:987–994
Riggio RE, Singer RD, Hartman K, Sneider R (1982) Psychological issues in the care of critically ill respirator patients: differential perceptions of patients, relatives, and staff. Psychol Rep 51:363–369
Jackson JC, Hart RP, Gordon SM, Hopkins RO, Girard TD, Ely EW (2007) Post-traumatic stress disorder and post-traumatic stress symptoms following critical illness in medical intensive care unit patients: assessing the magnitude of the problem. Crit Care 11:R27
Granja C, Gomes E, Amaro A, Ribeiro O, Jones C, Carneiro A, Costa-Pereira A (2008) Understanding posttraumatic stress disorder-related symptoms after critical care: the early illness amnesia hypothesis. Crit Care Med 36:2801–2809
Gil S, Caspi Y, Ben-Ari IZ, Koren D, Klein E (2005) Does memory of a traumatic event increase the risk for posttraumatic stress disorder in patients with traumatic brain injury? A prospective study. Am J Psychiatry 162:963–969
Jones C, Griffiths RD, Humphris G, Skirrow PM (2001) Memory, delusions, and the development of acute posttraumatic stress disorder-related symptoms after intensive care. Crit Care Med 29:573–580
Scheier MF, Matthews KA, Owens JF, Schulz R, Bridges MW, Magovern GJ, Carver CS (1999) Optimism and rehospitalization after coronary artery bypass graft surgery. Arch Intern Med 159:829–835
Schou I, Ekeberg O, Ruland CM, Sandvik L, Karesen R (2004) Pessimism as a predictor of emotional morbidity one year following breast cancer surgery. Psychooncology 13:309–320
Le G Jr, Lemeshow S, Saulnier F (1993) A new Simplified Acute Physiology Score (SAPS II) based on a European/North American multicenter study. JAMA 270:2957–2963
Reis MD, Moreno R, Iapichino G (1997) Nine equivalents of nursing manpower use score (NEMS). Intensive Care Med 23:760–765
Langen I, Myhren H, Ekeberg O, Stokland O (2006) Patient’s satisfaction and distress compared with expectations of the medical staff. Patient Educ Couns 63:118–125
Zigmond AS, Snaith RP (1983) The hospital anxiety and depression scale. Acta Psychiatr Scand 67:361–370
Herrmann C (1997) International experiences with the hospital anxiety and depression scale—a review of validation data and clinical results. J Psychosom Res 42:17–41
Bjelland I (2004) Anxiety and depression in the general population: issues related to assessment, comorbidity, and risk factors. Doctoral dissertation. University og Bergen, Bergen, Norway
Sundin EC, Horowitz MJ (2002) Impact of event scale: psychometric properties. Br J Psychiatry 180:205–209
Horowitz M, Wilner N, Alvarez W (1979) Impact of event scale: a measure of subjective stress. Psychosom Med 41:209–218
Johansen VA, Wahl AK, Eilertsen DE, Weisaeth L (2007) Prevalence and predictors of post-traumatic stress disorder (PTSD) in physically injured victims of non-domestic violence. A longitudinal study. Soc Psychiatry Psychiatr Epidemiol 42:583–593
Scheier MF, Carver CS, Bridges MW (1994) Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): a reevaluation of the life orientation test. J Pers Soc Psychol 67:1063–1078
Schou I, Ekeberg O, Sandvik L, Ruland CM (2005) Stability in optimism–pessimism in relation to bad news: a study of women with breast cancer. J Pers Assess 84:148–154
Jones C, Humphris G, Griffiths RD (2000) Preliminary validation of the ICUM tool: a tool for assessing memory of the intensive care experience. Clin Intensive Care 11:251–255
Capuzzo M, Valpondi V, Cingolani E, De LS, Gianstefani G, Grassi L, Alvisi R (2004) Application of the Italian version of the Intensive Care Unit Memory tool in the clinical setting. Crit Care 8:R48–R55
Kvale R, Ulvik A, Flaatten H (2003) Follow-up after intensive care: a single center study. Intensive Care Med 29:2149–2156
Ringdal M, Plos K, Lundberg D, Johansson L, Bergbom I (2009) Outcome after injury: memories, health-related quality of life, anxiety, and symptoms of depression after intensive care. J Trauma 66:1226–1233
Ringdal M, Johansson L, Lundberg D, Bergbom I (2006) Delusional memories from the intensive care unit—experienced by patients with physical trauma. Intensive Crit Care Nurs 22:346–354
Skovlund E, Fenstad GU (2001) Should we always choose a nonparametric test when comparing two apparently nonnormal distributions? J Clin Epidemiol 54:86–92
Brewin CR, Andrews B, Valentine JD (2000) Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. J Consult Clin Psychol 68:748–766
Jin RL, Shah CP, Svoboda TJ (1995) The impact of unemployment on health: a review of the evidence. CMAJ 153:529–540
Capuzzo M, Pinamonti A, Cingolani E, Grassi L, Bianconi M, Contu P, Gritti G, Alvisi R (2001) Analgesia, sedation, and memory of intensive care. J Crit Care 16:83–89
Knaus WA, Draper EA, Wagner DP, Zimmerman JE (1986) An evaluation of outcome from intensive care in major medical centers. Ann Intern Med 104:410–418
Rotondi AJ, Chelluri L, Sirio C, Mendelsohn A, Schulz R, Belle S, Im K, Donahoe M, Pinsky MR (2002) Patients’ recollections of stressful experiences while receiving prolonged mechanical ventilation in an intensive care unit. Crit Care Med 30:746–752
Samuelson K, Lundberg D, Fridlund B (2006) Memory in relation to depth of sedation in adult mechanically ventilated intensive care patients. Intensive Care Med 32:660–667
Weinert CR, Sprenkle M (2008) Post-ICU consequences of patient wakefulness and sedative exposure during mechanical ventilation. Intensive Care Med 34:82–90
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Myhren, H., Tøien, K., Ekeberg, Ø. et al. Patients’ memory and psychological distress after ICU stay compared with expectations of the relatives. Intensive Care Med 35, 2078–2086 (2009). https://doi.org/10.1007/s00134-009-1614-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-009-1614-1