Abstract
Purpose
Monitoring end-expiratory lung volume (EELV) is a valuable tool to optimize respiratory settings that could be of particular importance in mechanically ventilated pediatric patients. We evaluated the feasibility and precision of an intensive care unit (ICU) ventilator with an in-built nitrogen washout/washin technique in mechanically ventilated pediatric patients.
Methods
Duplicate EELV measurements were performed in 30 patients between 5 kg and 43 kg after cardiac surgery (age, median + range: 26, 3–141 months). All measurements were taken during pressure-controlled ventilation at 0 cm H2O of positive end-expiratory pressure (PEEP).
Results
Linear regression between duplicate measurements was excellent (R 2 = 0.99). Also, there was good agreement between duplicate measurements, bias ± SD: −0.3% (−1.5 mL) ± 5.9% (19.2 mL). Mean EELV ± SD was 19.6 ± 5.1 mL/kg at 0 cm H2O PEEP. EELV correlated with age (p < 0.001, r = 0.92, R 2 = 0.78), body weight (p < 0.001, r = 0.91, R 2 = 0.82) and height (p < 0.001, r = 0.94, R 2 = 0.75).
Conclusion
This ICU ventilator with an in-built nitrogen washout/washin EELV technique can measure EELV with precision, and can easily be used for mechanically ventilated pediatric patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Monitoring end-expiratory lung volume (EELV) might be a valuable tool to optimize respiratory settings in anesthetized ventilated patients [1]. General anesthesia is known to promote lung volume reduction, which promotes atelectasis, lung compliance, and arterial oxygenation [2]. In children, decreased lung volume is of special importance because of the lower elastic retraction forces and a lower relaxation volume, which makes them more prone to airway collapse [3, 4]. Furthermore, EELV has been described as one of the variables known to adequately assess mechanical characteristics of the ventilated lung [5].
However, determining EELV in ventilated patients is not without difficulty. EELV can be measured with computer tomography [6, 7], but this technique is not available for routine measurements. Traditionally, EELV measurement techniques are based on dilution of tracer gases, like sulfur hexafluoride washout [8, 9], closed-circuit helium dilution [10], or open-circuit multibreath nitrogen washout [11–13]. All these techniques require expensive and/or complex instrumentation, and are generally not suitable for routine EELV measurements during surgery and in the intensive care unit (ICU). An alternative is the simplified helium dilution method, using a re-breathing bag with a helium mixture. However, an important disadvantage of this latter technique is the interruption of mechanical ventilation for a short period of time [14].
Recently, Stenqvist et al. [15] introduced a novel method to measure EELV without interruption of mechanical ventilation, based on a simplified and modified multiple Breath nitrogen washout (MBNW) technique, which is integrated within a mechanical ventilator. This method requires a step change in the inspired oxygen fraction (FiO2), without the need for supplementary tracer gases or specialized additional monitoring equipment [15]. Although this method has been successfully applied in adult ventilated patients at the ICU and whilst undergoing surgery [15–17], no data regarding feasibility and precision exist for mechanically ventilated pediatric patients.
Therefore, we evaluated the feasibility and precision of this MBNW device to measure EELV during mechanical ventilation of pediatric patients after cardiac surgery.
Methods
After approval of the local institutional human investigations committee, 30 mechanically ventilated children were enrolled in the study. All patients underwent cardiac surgery for congenital heart repair, and received postoperative mechanical ventilatory support in the ICU. Exclusion criteria were: severe cardiovascular instability, thoracic deformations, and residual intracardiac shunt postoperatively evaluated by transesophageal echocardiography (TEE).
EELV measurements were carried out with the COVX module (GE Healthcare, Helsinki, Finland) integrated within the ventilator. This module has been described in detail earlier [15]. Briefly, O2 and CO2 are measured with standard clinical sensors and the residual N2 as remaining ventilator air is calculated. A step change in the N2 concentration is induced by changing the FiO2. The N2 volume change and N2 fraction change is measured with the COVX module integrated in the Engström Carestation ventilator and EELV is calculated.
Patients were nasotracheally intubated with a cuffed Hi-Contour pediatric endotracheal tube (Mallinckrodt) and anesthesia was maintained with midazolam 0.1 mg/(kg h) and sufentanil 1 mcg/(kg h). During the operation, patients were ventilated in pressure-controlled mode at the following settings: tidal volume of 6–8 mL/kg, frequency adjusted to maintain a PaCO2 level between 4.5 and 5.5 kPa, positive end-expiratory pressure (PEEP) of 8 cm H2O, I/E ratio of 1:1 and FiO2 of 0.5. After weaning from cardiopulmonary bypass (CPB), the lungs were routinely re-expanded by a recruitment maneuver (RCM) and mechanical ventilation was continued with the same settings as before CPB. Once admitted to the ICU, mechanical ventilation was continued with the same settings as before transportation except for the FiO2, which was set at 0.40 or 0.45. FiO2 was decreased because the measurement requires a FiO2 step change and becomes less precise at a FiO2 above 0.65, according to manufacturer's specifications. Patients were sedated by midazolam intravenously [0.1 mg/(kg h)] and morphine [10 mcg/(kg h)].
After stabilization at the ICU, EELV was measured twice (washout and washin) with the COVX module by nitrogen washout/washin with first an incremental and second a decremental FiO2 step of 0.2 at a PEEP of 0 cm H2O. This measurement was repeated after 10 min. Before measurements, hemodynamic and ventilatory parameters were recorded and arterial blood gas analysis was performed.
Statistical analysis
Statistical analysis was performed with Graphpad software package (version 5.0, Graphpad Software Inc., San Diego, USA). Results are expressed as mean ± SD for normally distributed data and median and interquartile range (IQR) for not normally distributed data. The Shapiro–Wilk normality test was used to evaluate the distribution of all data. Agreement between duplicate measurements was analyzed using Spearman correlation and Bland–Altman’s analysis [18]. For all comparisons, p < 0.05 was considered significant.
Results
In the present study, 30 mechanically ventilated patients were examined; Table 1 presents demographic data and the main physiologic characteristics. All patients were studied after congenital cardiothoracic surgery and tolerated the procedure well. Repairs included closure of ventricular septal defect (7), closure of atrial septal defect (8), correction of tetralogy of Fallot (3), repair of subpulmonary stenosis (3) and subaortal stenosis (2), pacemaker implantation (1), and total cavopulmonary connection (6). The hemodynamic and ventilatory parameters before the measurements at 0 cm H2O PEEP are provided in Table 2.
Linear regression between duplicate EELV measurements (as average of washin/washout) measured with the nitrogen washin/washout technique was performed. Duplicate measurements were highly correlated (p < 0.001, r = 0.99, R 2 = 0.99). To assess the difference between the duplicate measurements a Bland–Altmann analysis was performed (Fig. 1). Bias ± SD was −0.3% (−1.5 mL) ± 5.9% (19.2 mL).
Bland–Altman analysis. Comparison of duplicate end-expiratory lung volume (EELV) measurements with the multibreath nitrogen washout technique. Measurements were performed in the supine position at 0 cm H2O positive end-expiratory pressure (PEEP) in mechanically ventilated pediatric patients after cardiac surgery
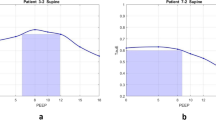
Mean EELV ± SD was 19.6 ± 5.1 mL/kg at a PEEP level of 0 cm H2O. Figure 2 shows the relation between EELV and patient characteristics. EELV was highly correlated with age (p < 0.001, r = 0.92, R 2 = 0.78), body weight (p < 0.001, r = 0.91, R 2 = 0.82) and height (p < 0.001, r = 0.94, R 2 = 0.75).
Relation between EELV (average of duplicates) and height or body weight. Measurements were performed in the supine position at 0 cm H2O PEEP in mechanically ventilated pediatric patients after cardiac surgery. The lines represent non-linear regression equations from non-intubated children, Stocks and Quanjer [26] and intubated children at 0 cm H2O PEEP, Thorsteinsson et al. [23] and Bar-Yishay et al. [21]
Discussion
The present study shows that, in sedated mechanically ventilated pediatric patients, this noninvasive MBNW technique can easily measure EELV with good precision. We confirmed that EELV is highly correlated with the patient’s height and body weight (Fig. 2).
Precise and easily performable measurements of EELV are essential in order to use this parameter to optimize respiratory settings. Although accurate and precise methods to measure EELV are available for ventilated pediatric patients, these older methods require complex equipment or tracer gases that limit their use in clinical practice [8, 19]. In this study, we used an ICU ventilator with an in-built MBNW technique to measure EELV during mechanical ventilation; a good agreement was found between duplicate measurements with this device. Chiumello et al. [20] recently compared this technique with computed tomography and helium dilution in adult ICU patients and described high reproducibility between duplicate measurements (bias ± SD 48 ± 165 mL). In our pediatric patients an even better level of precision was found: bias ± SD 1.0% (−1.7 mL) ± 5.7% (15.5 mL).
Although accuracy was not evaluated in the present study, measured EELV was comparable to that reported in other studies [21–24]. Ungern-Sternberg et al. [24] described the effect of CPB and aortic clamping on EELV in children during mechanical ventilation with 3 cm H2O PEEP; in their study EELV increased from 22 ± 5 to 27 ± 6 mL/kg after opening of the chest and decreased markedly to 16 ± 5 mL/kg after closing the chest and was still reduced to 18 ± 5 mL/kg during the following 90 min. These values are comparable with our measured EELV (mean ± SD) of 19.6 ± 5.1 mL/kg. Moreover, our values are similar to those of pediatric patients during nitrous-oxide-halothane anesthesia, in which an EELV (mean ± SD) of 19 ± 6 mL/kg was found during mechanical ventilation and 22 ± 7 mL/kg during spontaneous breathing [22].
Schibler et al. [25] investigated the effect of different levels of PEEP on EELV in 22 mechanically ventilated children. At 0 cm H2O PEEP, EELV was 20 ± 7 mL/kg, which is comparable to our results. At a PEEP of 5 and 10 EELV increased to 24 ± 8 and 28 ± 6 mL/kg, respectively. In the present study, we did not use PEEP during the measurements to allow comparison to studies in which EELV was measured without PEEP [21, 23, 26]. The application of PEEP is known to increase EELV and to prevent the formation of atelectasis. If higher PEEP levels were used, the EELV could be restored to above the normal values displayed in Fig. 2.
Among our patients, characteristics such as age, height, and body weight were highly correlated with measured EELV (Fig. 2). Our data are comparable with data from two previous studies [21, 23] in which children were ventilated without the application of PEEP. Below 1 m of height or below 15 kg body weight, the agreement was excellent, but above 1 m of height most of our values were slightly below their regression equations. The reason for this is unknown. Thorsteinsson et al. [23], measured EELV directly after induction of anesthesia in healthy children and in children with cardiac anomalies, whereas we measured EELV after cardiac surgery with CPB. It is known that cardiac surgery and CBP may lower EELV [24, 27]. Bar-Yishay et al. [21], measured EELV in awake children in the supine position or during ketamine anesthesia. Ketamine anesthesia is known to preserve lung function [28].
A potential limitation of the present study is that accuracy was not evaluated. However, measured values with this technique were close to those of previous studies. Another potential limitation of the used technique is the measurement of EELV in patients requiring a FiO2 >65%. It has been suggested in the manufacturer's specifications that the accuracy error increases from 10% to 15% at a FiO2 >0.65 in adult patients. However, in the present study we only measured at a FiO2 <65%. An important advantage of this method is that no tracer gases and no expensive or specialized equipment are required, bringing this parameter closer to clinical practice.
Therefore, we conclude that this nitrogen washout EELV technique can measure EELV with good precision. Especially below a height of 1 m or 15 kg body weight, our data are in good agreement with earlier comparable studies. Furthermore, this device can easily be used in mechanically ventilated pediatric patients without a tracer gas and without interruption of mechanical ventilation.
Abbreviations
- CPB:
-
Cardiopulmonary bypass
- EELV:
-
End-expiratory lung volume
- FiO2 :
-
Fraction of inspired oxygen
- ICU:
-
Intensive care unit
- NMBW:
-
Multiple breath nitrogen washout
- PEEP:
-
Positive end-expiratory pressure
- RCM:
-
Recruitment maneuver
- TEE:
-
Transesophageal echocardiography
References
Hedenstierna G (1993) The recording of FRC—is it of importance and can it be made simple? Intensive Care Med 19:365–366
Hedenstierna G, Edmark L (2005) The effects of anesthesia and muscle paralysis on the respiratory system. Intensive Care Med 31:1327–1335
Lumb AB (2005) Nunn’s applied respiratory physiology, 6th edn. Elsevier, Philadelphia
Mansell A, Bryan C, Levison H (1972) Airway closure in children. J Appl Physiol 33:711–714
Schibler A, Frey U (2002) Role of lung function testing in the management of mechanically ventilated infants. Arch Dis Child Fetal Neonatal Ed 87:F7–F10
Drummond GB (1998) Computed tomography and pulmonary measurements. Br J Anaesth 80:665–671
Gattinoni L, Caironi P, Pelosi P, Goodman LR (2001) What has computed tomography taught us about the acute respiratory distress syndrome? Am J Respir Crit Care Med 164:1701–1711
Fuchs SI, Buess C, Lum S, Kozlowska W, Stocks J, Gappa M (2006) Multiple breath washout with a sidestream ultrasonic flow sensor and mass spectrometry: a comparative study. Pediatr Pulmonol 41:1218–1225
Ungern-Sternberg BS, Hammer J, Frei FJ, Jordi Ritz EM, Schibler A, Erb TO (2007) Prone equals prone? Impact of positioning techniques on respiratory function in anesthetized and paralyzed healthy children. Intensive Care Med 33:1771–1777
Di Marco F, Rota SL, Milan B, Stucchi R, Centanni S, Brochard L, Fumagalli R (2007) Measurement of functional residual capacity by helium dilution during partial support ventilation: in vitro accuracy and in vivo precision of the method. Intensive Care Med 33:2109–2115
Fretschner R, Deusch H, Weitnauer A, Brunner JX (1993) A simple method to estimate functional residual capacity in mechanically ventilated patients. Intensive Care Med 19:372–376
Hammer J, Numa A, Newth CJ (1998) Total lung capacity by N2 washout from high and low lung volumes in ventilated infants and children. Am J Respir Crit Care Med 158:526–531
Sivan Y, Deakers TW, Newth CJ (1990) An automated bedside method for measuring functional residual capacity by N2 washout in mechanically ventilated children. Pediatr Res 28:446–450
Patroniti N, Bellani G, Manfio A, Maggioni E, Giuffrida A, Foti G, Pesenti A (2004) Lung volume in mechanically ventilated patients: measurement by simplified helium dilution compared to quantitative CT scan. Intensive Care Med 30:282–289
Olegard C, Sondergaard S, Houltz E, Lundin S, Stenqvist O (2005) Estimation of functional residual capacity at the bedside using standard monitoring equipment: a modified nitrogen washout/washin technique requiring a small change of the inspired oxygen fraction. Anesth Analg 101:206–212
Bikker IG, van Bommel J, Dos Reis MD, Bakker J, Gommers D (2008) End-expiratory lung volume during mechanical ventilation: a comparison to reference values and the effect of PEEP in ICU patients with different lung conditions. Crit Care 12:R145
Erlandsson K, Odenstedt H, Lundin S, Stenqvist O (2006) Positive end-expiratory pressure optimization using electric impedance tomography in morbidly obese patients during laparoscopic gastric bypass surgery. Acta Anaesthesiol Scand 50:833–839
Bland JM, Altman DG (1986) Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1:307–310
Ungern-Sternberg BS, Regli A, Frei FJ, Hammer J, Jordi Ritz EM, Erb TO (2007) Decrease in functional residual capacity and ventilation homogeneity after neuromuscular blockade in anesthetized preschool children in the lateral position. Paediatr Anaesth 17:841–845
Chiumello D, Cressoni M, Chierichetti M, Tallarini F, Botticelli M, Berto V, Mietto C, Gattinoni L (2008) Nitrogen washout/washin, helium dilution and computed tomography in the assessment of end expiratory lung volume. Crit Care 12:R150
Bar-Yishay E, Shulman DL, Beardsmore CS, Godfrey S (1987) Functional residual capacity in healthy preschool children lying supine. Am Rev Respir Dis 135:954–956
Larsson A, Jonmarker C, Lindahl SG, Werner O (1989) Lung function in the supine and lateral decubitus positions in anaesthetized infants and children. Br J Anaesth 62:378–384
Thorsteinsson A, Jonmarker C, Larsson A, Vilstrup C, Werner O (1990) Functional residual capacity in anesthetized children: normal values and values in children with cardiac anomalies. Anesthesiology 73:876–881
Ungern-Sternberg BS, Petak F, Saudan S, Pellegrini M, Erb TO, Habre W (2007) Effect of cardiopulmonary bypass and aortic clamping on functional residual capacity and ventilation distribution in children. J Thorac Cardiovasc Surg 134:1193–1198
Schibler A, Henning R (2002) Positive end-expiratory pressure and ventilation inhomogeneity in mechanically ventilated children. Pediatr Crit Care Med 3:124–128
Stocks J, Quanjer PH (1995) Reference values for residual volume, functional residual capacity and total lung capacity. ATS Workshop on Lung Volume Measurements. Official Statement of The European Respiratory Society. Eur Respir J 8:492–506
Gilliland HE, Armstrong MA, McMurray TJ (1999) The inflammatory response to pediatric cardiac surgery: correlation of granulocyte adhesion molecule expression with postoperative oxygenation. Anesth Analg 89:1188–1191
Ungern-Sternberg BS, Regli A, Frei FJ, Ritz EM, Hammer J, Schibler A, Erb TO (2007) A deeper level of ketamine anesthesia does not affect functional residual capacity and ventilation distribution in healthy preschool children. Paediatr Anaesth 17:1150–1155
Acknowledgments
The authors thank Laraine Visser-Isles for English language editing.
Conflict of interest statement
The department of Intensive Care, Erasmus MC, received an unrestricted grant from GE Healthcare.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Bikker, I.G., Scohy, T.V., Ad J. J. C. Bogers et al. Measurement of end-expiratory lung volume in intubated children without interruption of mechanical ventilation. Intensive Care Med 35, 1749–1753 (2009). https://doi.org/10.1007/s00134-009-1579-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-009-1579-0