Abstract
Background
Inappropriate selection of tidal volume and rate on mechanical ventilators in patients with reduced lung volume may cause lung damage. In spite of this rather recent insight, the optimal breath pattern and the relative importance of elevating end-expiratory lung volume (EELV) are still debated. A recent hypothesis is that lung injury is caused by excessive stress and strain. This paper elaborates on that hypothesis and proposes a new approach to optimizing the breath pattern.
Methods
An index to quantify the impact of positive pressure ventilation on the lungs is defined (Stress–Strain Index, SSI) and calculated as a function of the breath pattern (tidal volume V t and respiratory rate f) for five different levels of EELV. The breath pattern at which SSI is minimal (mSSI strategy) was compared with three other strategies: the “6 ml/kg V t,” minimal work of breathing and minimal force to breathe, for the different EELV levels.
Results
In the mathematical analysis, SSI was mainly determined by EELV and was much higher with low EELV. For each EELV level, a distinct minimum of SSI was found, defined by a particular V t − f combination. The mSSI strategy yielded lower V t and higher f (0.252 l and 39 b/min) as compared to the “6 ml/kg V t” strategy (0.420 l and 17 b/min).
Conclusion
The EELV is the main determinant of the SSI. For a given EELV, the SSI can be minimized by an optimal V t − f combination.
Similar content being viewed by others
Introduction
Mammals select their breath pattern to minimize energy [1] or muscular force [2] in order to produce adequate alveolar ventilation. Conversely, the breath pattern of passively ventilated patients is governed by caregivers. In the 1970s, the tidal volume (V t) was set to 12–15 ml per kg body weight [3], and rate (f) was adjusted to meet expectations for PaCO2, even for patients with acute respiratory distress syndrome (ARDS). It is now widely accepted that mechanical ventilation with excessive V t and plateau airway pressure (P pla) can cause lung injury, and this recipe has been modified to 6 ml per kg of predicted ideal body weight [4].
While the actual approach to ventilate patients with ARDS is to reduce V t and P pla, a recent study [5] found that both are inadequate surrogates for the stress and strain within the lungs: excessive stress and strain can be produced whatever the V t and P pla. The stress is equivalent to the trans-pulmonary pressure, and the strain to the V t changes relative to the end expiratory lung volume (EELV) [6]. The product of both, can be viewed as the energy delivered by the ventilator within the lungs and an estimate of much the ventilator can damage the lungs. Therefore, a plausible ventilation strategy to minimize lung injury is to minimize both, the trans-pulmonary pressure (stress) and the V t to EELV ratio (strain).
This paper explores the possibilities to minimize stress and strain by finding an optimal combination of V t and f. A Stress–Strain Index (SSI) is defined, and the optimal V t and f combination, i.e., the one minimizing SSI, is calculated for different EELVs. This optimal V t and f combination is compared with the “6 ml/kg V t” strategy [4] and the previously published optimization strategies “minimal work of breathing” [1] and “the minimal force to breathe” [2].
Methods
Derivation of the Stress–Strain Index (SSI)
The full computations and equations can be found in the electronic supplementary material (ESM).
Fundamental description of strain and stress and the premise of their product, i.e., the energy delivered within the lungs by the ventilator estimates the potential for lung injury, can be found elsewhere [6, 7]. The relative contribution of stress and strain in the SSI was expressed by weighting stress and strain with α and β coefficients, both being between 0 and 1. Thus, the SSI per minute can be defined as
with strain being the V t to EELV ratio and stress being the change in trans-pulmonary pressure (dP L); Eq. 1 becomes
and is in unit of mbar/min or mJ/s per l.
Introducing the specific elastance of the lung (E L,sp) with E L being the elastance,
dP L can be expressed as:
and Eq. 2 becomes:
To find the least injurious V t − f combination, i.e., V t and f at which SSI is minimal, the first derivative of Eq. 5 with respect to f needs to be set to zero and be solved for the following boundary conditions: (B1) alveolar ventilation (V′A) is constant; (B2) expiratory time is longer than two times the time constant of the respiratory system; (B3) E L does not change with f and is linear within the tidal pressure–volume ranges; (B4) EELV and stress and strain are stable from breath to breath.
According to B1, V ′A remains constant:
where V d is dead space (anatomical dead space or series dead space).Substituting V ′A by the expression of Eq. 6, the SSI becomes:
The first derivative of this function with respect to f and set to zero yields f at which SSI is minimal (mSSI):
and V t at which SSI is minimal follows from Eq. 6:
Note that α and β coefficients dropped out by derivation of Eq. 7, meaning that f and V t at mSSI are not depending on the weight assigned to stress and strain in the SSI calculation.
Numerical simulations
The SSI was calculated for different levels of EELV, different mechanical properties (Table 1) and all possible V t and f combinations to achieve a pre-set alveolar ventilation.
In a next step, and for each EELV value, the f − V t combinations resulting in mSSI (mSSI strategy) were calculated and compared with SSI obtained with the “6 ml/kg V t” strategy, as well as with “minimal Work of Breathing” (mWOB) and “minimal Force to breathe” (mForce) strategies.
All calculations were made using MS-EXCEL 2003. Any deviations from the boundary conditions described above are described in the text, where appropriate.
Results
Stress–Strain Index was heavily and inversely dependent on EELV increasing quasi-exponentially when EELV decreases (Fig. 1).
The Stress-Strain Index on the x-axis plotted against the end expiratory lung volume (EELV) on the y-axis and the tidal volume (V t, left panel) and the respiratory rate (f, right panel) on the z-axis. The Stress-Strain Index increased quasi-exponentially with the EELV (x–y axis) and for low EELV, a specific V t and f at which the SSI is minimal can be found (y–z axis)
For each level of EELV a breath pattern that minimized SSI was found (Table 2). However, the effects of V t − f combinations in changing SSI were more obvious at low EELV (Fig. 1).
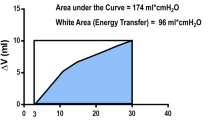
The breath strategies compared gave very different SSI at low EELV but are very similar when EELV is normal or high (Fig. 2).
Discussion
The present paper elaborates on the stress and strain concept applied to mechanical ventilation as described by Gattinoni and co-workers [5, 6] and explores the effect of EELV and the selection of f and V t on a SSI in mechanically ventilated patients.
The main findings are
-
1.
The SSI clearly depends on EELV, increasing dramatically when EELV is reduced (Fig. 1).
-
2.
For each level of EELV, an optimal V t − f combination resulting in a minimal SSI can be calculated.
-
3.
The impact of f and V t on SSI is much larger when EELV is reduced as compared to normal or high EELV.
It is tempting to connect the different levels of EELV to diseases such as ARDS (“low EELV”) and COPD (“high EELV”). In such a clinical context, the results indeed make intuitive sense. However, the pathophysiology cannot be reduced to simple differences in EELV. In ARDS, lung volume is reduced, but the collapsed or nearly collapsed regions of the lung are still physically present and may present a diffuse pattern of open and closed alveoli. Such inhomogeneity is known to create shear stress and strain, which may lead to lung damage and not the reduction of lung volume per se [8]. In COPD, the lung volume is increased because of dynamic hyper-inflation and parenchymal alterations. Such alterations may weaken the lung structures and make them prone to risk for injury. On one hand, it is likely that the SSI will underestimate the risk for lung injury in ARDS and COPD by oversimplifying the different forces and deformations applied to the lung structures [7]. On the other hand, SSI has always a distinct minimum at a certain V t − f combination, which remains valid even thought the absolute SSI value may not be correct.
Numerical simulations showed that SSI always has a minimum at a particular V t and f combination. Although EELV was an important factor for the calculation of SSI, EELV did not play a role in finding the optimal breath pattern. In fact, EELV simply dropped out of the equation of minimal SSI.
We assumed stable conditions such as constant alveolar ventilation and constant respiratory mechanics. Stress and strain were multiplied with factors α and β, respectively, to give each component its specific weight and to allow for a sensitivity analysis. Indeed weighting stress and strain differently may generate different SSI values. However, as factors α and β dropped out during the first derivation of Eq. 7, it does not play a role in finding the optimal f and V t combination.
Clinical implications
Assuming that stress and strain are determinants of lung injury and SSI as to estimating such stress and strain, it makes sense to reduce SSI as much as possible during mechanical ventilation. Because EELV is a main component in the SSI calculation (see Eq. 7), increasing EELV is obviously the first step to tentatively reduce lung injury induced by mechanical ventilation. Methods to increase EELV include PEEP, controlled use of dynamic hyperinflation, recruitment manoeuvres or a combination thereof [9]. However, it is important to critically upraise the beneficial effects of these measures, particularly PEEP, since their benefit will depend on how much they can open the lungs and keep them open [6]. Basically, if PEEP is recruiting the lung and increasing EELV, the strain is reduced as the denominator in Eq. 2 is increased. If PEEP is not recruiting the lung but overdistending the healthy part of the lung, for instance, one may assume no beneficial effect on the strain. Finally, the effect of PEEP on the stress depends on how much the trans-pulmonary pressure is increased by such PEEP. Interestingly, a recent paper [10] suggests that by setting PEEP based on the esophageal pressure to estimate the trans-pulmonary pressure, i.e., the stress, would result in better oxygenation and clinical outcomes.
Apart from increasing EELV, an additional step to reduce the SSI is to set f and V t according to Eqs. 8 and 9, respectively. These equations yield a lower V t than the “6 ml/kg V t” strategy, which, if used on patients, will require closed monitoring of dead space ventilation and expiratory time constants to avoid inefficient ventilation and inadvertent breath stacking. Ultimately, the present findings show that lower V t and higher f may be beneficial in patients with reduced EELV.
Cautious conclusions
The present computational study found that EELV is the most important determinant of the SSI, which in turn can be minimized by a specific breath pattern. The biological relevance of the SSI as defined in the present study, as well as the clinical implications of minimizing such an index, needs to be further investigated.
References
Otis AB, Fenn WO, Rahn H (1950) Mechanics of breathing in man. J Appl Physiol 2:592–607
Mead J (1961) Mechanical properties of lungs. Physiol Rev 41:281–330
Pontoppidan H, Geffin B, Lowenstein E (1972) Acute respiratory failure in the adult. N Engl J Med 19:799–806
The Acute Respiratory Distress Syndrome Network (2000) Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med 342:1301–1308
Chiumello D, Carlesso E, Cadringher P, Caironi P, Valenza F, Polli F, Tallarini F, Cozzi P, Cressoni M, Colombo A, Marini JJ, Gattinoni L (2008) Lung stress and strain during mechanical ventilation of the acute respiratory distress syndrome. Am J Respir Crit Care Med 178:346–355
Gattinoni L, Carlesso E, Cadringher P, Valenza F, Vagginelli F, Chiumello D (2003) Physical and biological triggers of ventilator-induced lung injury and its prevention. Eur Respir J 47:15s–25s
Wilson TA (1986) Solid mechanics. In: American Physiological Society (ed) Handbook of physiology: a critical comprehensive presentation of physiological knowledge and concepts. Waverly Press, Baltimore, pp 35–39
Vlahakis NE, Hubmayr RD (2005) Cellular stress failure in ventilator-injured lungs. Am J Respir Crit Care Med 171:1328–1342
Kacmarek RM, Kallet RH (2007) Respiratory controversies in the critical care setting. Should recruitment maneuvers be used in the management of ALI and ARDS? Respir Care 52:622–631
Talmor D, Sarge T, Malhotra A, O’Donnell CR, Ritz R, Lisbon A, Novack V, Loring SH (2008) Mechanical ventilation guided by esophageal pressure in acute lung injury. N Engl J Med 359:2095–2104
Acknowledgments
The authors wish to thank Dominik Novotni and Thomas Laubscher for checking the mathematical formulas.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Brunner, J.X., Wysocki, M. Is there an optimal breath pattern to minimize stress and strain during mechanical ventilation?. Intensive Care Med 35, 1479–1483 (2009). https://doi.org/10.1007/s00134-009-1510-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-009-1510-8