Abstract
Purpose
To determine whether Stewart’s approach can improve our ability to diagnose acid–base disorders compared to the traditional model.
Methods
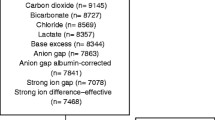
This prospective cohort study took place in a university-affiliated hospital during the period of February–May 2007. We recorded clinical data and acid–base variables from one hundred seventy-five patients at intensive care unit admission.
Results
Of the 68 patients with normal standard base excess (SBE) (SBE between −4.9 and +4.9), most (n = 59; 86.8%) had a lower effective strong ion difference (SIDe), and of these, 15 (25.4%) had SIDe < 30 mEq/L. Thus, the evaluation according to Stewart’s method would allow an additional diagnosis of metabolic disorder in 33.7% patients.
Conclusions
The Stewart approach, compared to the traditional evaluation, results in identification of more patients with major acid–base disturbances.
Similar content being viewed by others
References
Gunnerson KJ, Kellum JA (2003) Acid-base and electrolyte analysis in critically ill patients: are we ready for the new millennium? Curr Opin Crit Care 9:468–473
Sirker AA, Rhodes A, Grounds RM, Bennett ED (2002) Acid-base physiology: the “traditional” and the “modern” approaches. Anaesthesia 57:348–356
Martin M, Murray J, Berne T, Demetriades D, Belzberg H (2005) Diagnosis of acid-base derangements and mortality prediction in the trauma intensive care unit: the physiochemical approach. J Trauma 58:238–243
Cusack RJ, Rhodes A, Lochhead P, Jordan B, Perry S, Ball JA, Grounds RM, Bennett ED (2002) The strong ion gap does not have prognostic value in critically ill patients in a mixed medical/surgical adult ICU. Intensive Care Med 28:864–869
Balasubramanyan N, Havens P, Hoffman G (1999) Unmeasured anions identified by the Fencl-Stewart method predict mortality better than base excess, anion gap, and lactate in patients in the pediatric intensive care unit. Crit Care Med 27:1577–1581
Stewart PA (1981) How to understand acid base balance. In: Stewart PA (ed) A quantitative acid-base primer for biology and medicine. New York, Elsevier
Stewart PA (1983) Modern quantitative acid-base chemistry. Can J Physiol Pharmacol 61:1444–1461
Figge J, Rossing TH, Fencl V (1991) The role of serum proteins in acid-base equilibria. J Lab Clin Med 117:453–467
Figge J, Mydosh T, Fencl V (1992) Serum proteins and acid-base equilibria: a follow-up. J Lab Clin Med 120:713–719
Moviat M, van Haren F, van der Hoeven H (2003) Conventional or physicochemical approach in intensive care unit patients with metabolic acidosis. Crit Care 7:R41–R45
Murray DM, Olhsson V, Fraser JI (2004) Defining acidosis in postoperative cardiac patients using Stewart’s method of strong ion difference. Pediatr Crit Care Med 5:240–245
Figge J, Jabor A, Kazda A, Fencl V (1998) Anion gap and hypoalbuminemia. Crit Care Med 26:1807–1810
Fencl V, Leith DE (1993) Stewart’s quantitative acid-base chemistry: application in biology and medicine. Respir Physiol 91:1–16
Gilfix BM, Bique M, Magder S (1993) A physical chemical approach to the analysis of acid-base balance in the clinical setting. J Crit Care 8:187–197
Fencl V, Jabor A, Kazda A, Figge J (2000) Diagnosis of metabolic acid-base disturbances in critically ill patients. Am J Resp Crit Care Med 162:2246–2251
Kaplan LJ, Kellum JA (2004) Initial pH, base deficit, lactate, anion gap, strong ion difference, and strong ion gap predict outcome from major vascular injury. Crit Care Med 32:1120–1124
Dondorp AM, Chau TT, Phu NH, Mai NT, Loc PP, Chuong LV, Sinh DX, Taylor A, Hien TT, White NJ, Day NP (2004) Unidentified acid of strong prognostic significance in severe malaria. Crit Care Med 32:1683–1688
Boniatti MM, Cardoso PC, Castilho RK, Vieira SR, Friedman G, Ribeiro SP, Fialkow L (2008) Prognostic value of unmeasured anions in critically ill patients. Intensive Care Med (Supplement 1):S241
Henderson LJ (1908) The theory of neutrality regulation in the animal organism. Am J Physiol 21:427–428
Hasselbach KA (1916) Die Berechnung der Wasserstoffzahl des blutes auf der freien und gebundenen Kohlensaure desselben, und die Sauerstoffbindung des Blutes als Funktion der Wasserstoffzahl. Biochem Z 78:112–144
Siggard-Andersen O, Wimberly PD, Fogh-Andersen N, Gøthgen IH (1988) Measured and derived quantities with modern pH and blood gas equipment: calculation algorithms with 54 equations. Scand J Clin Lab Inves 48(Supp 189):7–15
Dubin A, Menises MM, Masevicius FD, Moseinco MC, Kutscherauer DO, Ventrice E, Laffaire E, Estenssoro E (2007) Comparison of three different methods of evaluation of metabolic acid-base disorders. Crit Care Med 35:1264–1270
Kellum JA (2007) Disorders of acid-base balance. Crit Care Med 35:2630–2636
Kellum JA (2003) Closing the gap on unmeasured anions. Crit Care 7:219–220
Knaus WA, Draper EA, Wagner DP, Zimmerman JE (1985) APACHE II: a severity of disease classification system. Crit Care Med 13:818–829
Vincent JL, Moreno R, Takala J, Willatts S, De Mendonça A, Bruining H, Reinhart CK, Suter PM, Thijs LG (1996) The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med 22:707–710
Funk G-C, Doberer D, Sterz F, Richling N, Kneidinger N, Lindner G, Schneeweiss B, Eisenburger P (2009) The strong ion gap and outcome after cardiac arrest in patients treated with therapeutic hypothermia: a retrospective study. Intensive Care Med 35:232–239
Rocktaeschel J, Morimatsu H, Uchino S, Bellomo R (2003) Unmeasured anions in critically ill patients: can they predict mortality? Crit Care Med 31:2131–2136
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Boniatti, M.M., Cardoso, P.R.C., Castilho, R.K. et al. Acid–base disorders evaluation in critically ill patients: we can improve our diagnostic ability. Intensive Care Med 35, 1377–1382 (2009). https://doi.org/10.1007/s00134-009-1496-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-009-1496-2