Abstract
Objective
To assess the role of antipseudomonal agents on Pseudomonas aeruginosa colonization and acquisition of resistance.
Design
Prospective cohort study.
Setting
Two medical intensive care units.
Patients and participants
346 patients admitted for ≥ 48 h.
Intervention
Analysis of data from an 8-month study comparing a mixing versus a cycling strategy of antibiotic use.
Measurements and results
Surveillance cultures from nares, pharynx, rectum, and respiratory secretions were obtained thrice weekly. Acquisition of resistance was defined as the isolation, after 48 h of ICU stay, of an isolate resistant to a given antibiotic if culture of admission samples were either negative or positive for a susceptible isolate. Emergence of resistance refers to the conversion of a defined pulsotype from susceptible to non-susceptible. Forty-four (13%) patients acquired 52 strains of P. aeruginosa. Administration of piperacillin-tazobactam for ≥ 3 days (OR 2.6, 95% CI 1.09–6.27) and use of amikacin for ≥ 3 days (OR 2.6, 95% CI 1.04–6.7) were positively associated with acquisition of P. aeruginosa, whereas use of quinolones (OR 0.27, 95% CI 0.1–0.7) and antipseudomonal cephalosporins (OR 0.27, 95% CI 0.08–0.9) was protective. Exposure to quinolones and cephalosporins was not associated with the acquisition of resistance, whereas it was linked with usage of all other agents. Neither quinolones nor cephalosporins were a major determinant on the emergence of resistance to themselves, as resistance to these antibiotics developed at a similar frequency in non-exposed patients.
Conclusions
In critically ill patients, quinolones and antipseudomonal cephalosporins may prevent the acquisition of P. aeruginosa and may have a negligible influence on the acquisition and emergence of resistance.
Similar content being viewed by others
Introduction
Pseudomonas aeruginosa is a leading cause of nosocomial infections in critically ill patients, and clinical disease is usually preceded by the settlement of the pathogen on mucosal surfaces [1]. Previous studies have established that acquisition of P. aeruginosa is associated with the administration of antimicrobial agents devoid of antipseudomonal activity [2, 3]. In this regard, however, the role of antipseudomonal agents is less clear. Some studies which have linked prior use of antibiotics with ventilator-associated pneumonia due to P. aeruginosa [4] or potentially resistant organisms (essentially P. aeruginosa, other non-fermenters and methicillin-resistant S. aureus) [5] have suggested that certain drugs such as imipenem, aminoglycosides and fluoroquinolones may have a role as individual risk factors, although their specific contribution has never been assessed.
P. aeruginosa is remarkable by the spontaneous generation of mutants resistant to any currently used antipseudomonal agent, which may be selected under appropriate antibiotic exposure. Emergence of resistance has been reported to occur in 6–53% of patients treated with any antipseudomonal agent [6–8]. In addition, several cohort or case-control studies have also linked previous use of antipseudomonal agents with the acquisition of P. aeruginosa resistant to the corresponding antibiotic [3, 9–21], other agents or multiple drugs [10, 12, 13, 15, 19, 22–31].
During an intervention study aimed to compare a mixing versus a cycling strategy of antibiotics use in the critical care setting [32], we were able to gather detailed longitudinal data about exposure to antibiotics and colonization by P. aeruginosa. We hypothesized that the risk of acquiring P. aeruginosa, of ending up by carrying a strain resistant to a given antipseudomonal agent that was susceptible or not present on admission and of developing of resistance in previously susceptible strains, could vary according to the particular antimicrobial to which the patient was exposed. The aims of the present study were to assess the role that exposure to each one of the antipseudomonal agents could have on the acquisition of P. aeruginosa, the role of exposure on the eventual carriage of a strain resistant to the same or a different antipseudomonal agent, and the role of exposure on the emergence of resistance in patients previously colonized with a susceptible strain.
Patients and methods
During eight consecutive months (from 15 October 2001 to 15 June 2002), patients admitted to two ICUs (a eight-bed medical ICU and a respiratory ICU with six beds) of a 700-bed university hospital whose expected length of stay was at least 2 days were included in a study aimed to compare the influence of two strategies (mixing vs. cycling) of use of anti-Pseudomonas antibiotics on the acquisition of resistant Gram-negative bacilli [32]. Patients were assigned to receive a cephalosporin, ciprofloxacin, a carbapenem or piperacillin-tazobactam in this order. Cycling was accomplished by prescribing one of these antibiotics during 1-month each. Mixing was accomplished by using the same order of antibiotic administration on consecutive patients. Interventions were carried out during two successive 4-month periods, starting with mixing in one unit and cycling in the other.
Microbiological procedures
Swabbing of nares, pharynx and rectum, and culture of respiratory secretions (tracheobronchial aspirates or sputum) were obtained thrice weekly. In addition, clinical samples were obtained as deemed necessary by the attending physician. No environmental cultures were taken. Susceptibility testing was done by a microdilution technique according to the CLSI guidelines [33]. For the purpose of analysis, intermediate susceptibility was considered as resistance. Molecular typing was performed by pulse-field gel electrophoresis (PFGE) using SpeI endonuclease as previously described [34].
Clinical variables
The set of clinical variables recorded is described in detail elsewhere [32] and correspond to those showed in Table 1. For the purposes of analysis, ceftazidime and cefepime were grouped as cephalosporins, imipenem and meropenem as carbapenems, and ciprofloxacin and levofloxacin as quinolones. Piperacillin-tazobactam and amikacin were considered individually.
Definitions
Patients with positive cultures within 48 h of admission to the units were considered to be colonized on admission. Microorganisms isolated after 48 h of admission were considered as ICU-acquired. In regards to species, acquisition was defined as a positive culture after 48 h of admission with previous negative specimens. Patients who acquired a pulsotype identical to that of an isolate previously found in another patient staying in the same unit and in the same period were considered to be cases of cross-transmission. Acquisition of resistance was defined as the isolation, after 48 h of ICU stay, of an isolate resistant to a given antimicrobial agent if culture of admission samples were either negative or positive for a susceptible isolate. Emergence of resistance to a given antibiotic refers to the conversion of a genotypically defined strain from susceptible to non-susceptible. Therefore, patients who fulfilled the “emergence of resistance” definition were the subset of patients that belonged to the “acquisition of resistance” group whose previously susceptible strain developed resistance. Time at risk means the time elapsed from ICU admission to the isolation of P. aeruginosa for patients acquiring the organisms or the length of ICU stay for those not acquiring the pathogen. Antibiotic exposure means at least 24 h of treatment. Colonization pressure with P. aeruginosa was estimated as previously described [35].
Statistical analysis
Clinical variables and exposures were compared between patients who acquired P. aeruginosa and those who did not; between patients who eventually carried a strain resistant to a given antipseudomonal agent that was either susceptible or not present on admission and those who did not; and, among patients colonized with a strain of P. aeruginosa susceptible to a given antipseudomonal agent, the same variables were compared between those in whom resistance to that antibiotic emerged and those in whom did not. For patients who reached the first two outcomes, evaluable exposures had to be present any time before detection of the defining event. For the third outcome, evaluable exposures had to be present from detection of the susceptible strain to isolation of its resistant counterpart.
Proportions were compared by using the χ2 or Fisher’s exact test. Continuous variables were compared by using the t test or Mann–Whitney test. A stepwise logistic regression procedure was used to select the best predictors of P. aeruginosa acquisition and acquisition of resistance to cephalosporins and quinolones. Only those variables with a P value ≤0.1 in the univariate analysis were entered into the logistic models. No attempt was made to perform multivariate analysis when the number of responses defining the outcome was less than 20.
Results
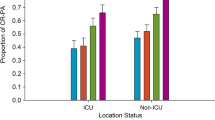
A total of 346 patients was evaluated, of whom 44 (13%) acquired 52 strains of P. aeruginosa during their ICU stay (37 patients acquired a sole strain, six acquired two and one acquired three). Twenty-eight (8%) additional patients were colonized on admission. Acquired isolates belonged to 17 unique genotypes, of which 9 were recovered from more than one patient. As a matter of fact, two unique strains colonized 50% of patients (one was acquired by 13, the other by eight and one patient acquired both). Out of the 52 isolates, 21 (40%) in 19 patients were acquired via cross-transmission and the remaining were of endogenous or unknown origin. Sites of primary detection included the rectum in 20 patients (45%), the nares or pharynx in 11 (25%), the lower respiratory tract in 3 (7%), more than one of these places in 9 (20%) and other sites (skin) in one (2%). The median time to P. aeruginosa acquisition was 6 days (IQ range 4.25–11.5, range 3–37).
Two-hundred and forty-three patients (70%) received an antipseudomonal agent during their ICU stay; 87 (25%) were exposed to cephalosporins (88% to cefepime), 97 (28%) to carbapenems (70% to imipenem), 81 (23%) to piperacillin-tazobactam, 126 (36%) to quinolones (89% to ciprofloxacin) and 83 (24%) to amikacin. Ninety-one patients received only one antipseudomonal agent (13 a cephalosporin, 20 a carbapenem, 26 piperacillin-tazobactam, 38 a quinolone and 4 amikacin), 100 received a single antipseudomonal β-lactam and either a quinolone (n = 51), amikacin (n = 34) or both (n = 15), 22 received more than one β-lactam, 8 received more than one β-lactam and amikacin, 21 received more than one β-lactam and both a quinolone and amikacin, and a patient received a quinolone and amikacin. Quinolones (n = 88, 70%) and amikacin (n = 79, 95%) were preferentially used in combination with other antipseudomonal agents. The median daily dosages were 4 g for cephalosporins, 3 g for carbapenems, 12 g for piperacillin-tazobactam, 800 mg for ciprofloxacin, 500 mg for levofloxacin, and 1 g for amikacin (given always as a single daily dose). Almost all patients (n = 331, 99%) received some antibiotic for at least 24 h during their ICU stay. Median (interquartile range) days of exposure were 4 (2–7) for cephalosporins, 6 for carbapenems (2–11.5), 5 (2–8) for piperacillin-tazobactam, 4 for quinolones (2–8), 6 for amikacin (2–9) and 5 (1.75–8) for other antimicrobial agents.
Risk factors for the acquisition of P. aeruginosa
The relation between patient characteristics or exposures and the acquisition of P. aeruginosa is shown in Table 1. In regards to the previous use of antibiotics, there was a significant positive association with piperacillin-tazobactam, amikacin and non-antipseudomonal agents, whereas the administration of quinolones and antipseudomonal cephalosporins was protective. Multivariate analysis selected the following variables as independently associated with the acquisition of P. aeruginosa: enteral nutrition (OR 11.4, 95% CI 4.9–26.4), prior administration of quinolones (OR 0.27, 95% CI 0.1–0.7), prior administration of antipseudomonal cephalosporins (OR 0.27, 95% CI 0.08–0.9), use of piperacillin-tazobactam during three days or longer (OR 2.6, 95% CI 1.09–6.27) and administration of amikacin during three days or longer (OR 2.6, 95% CI 1.04–6.7).
Relation between acquisition of resistance to antipseudomonal agents and prior exposure to the same or a different agent
The number of patients in whom a P. aeruginosa isolate resistant to the different antipseudomonal agents was detected during ICU stay, the resistance status of these strains when first isolated and the number of cases of cross-transmission are shown in Table 2. In most cases, resistance emerged from previous susceptible strains. Univariate analysis assessing the relationship between acquisition of resistance to the different antipseudomonal agents and prior exposure to each agent is shown in Table 3. Neither the use of antipseudomonal cephalosporins nor quinolones was associated with the acquisition of resistance. Conversely, administration of carbapenems was associated with acquisition of resistance to themselves, piperacillin-tazobactam and amikacin; use of piperacillin-tazobactam was associated with resistance to antipseudomonal cephalosporins, and use of amikacin was associated with the acquisition of resistance to itself, carbapenems and quinolones. Multivariate analysis selected enteral nutrition as the only risk factor independently associated with acquisition of quinolone resistance (OR 10.9, 95% CI 3.67–32.5), and enteral nutrition (OR 4.52, 95% CI 1.82–11.2) and exposure to piperacillin-tazobactam (OR 2.6, 95% CI 1.12–6) as the main predictors of cephalosporin resistance acquisition. After adjusting for enteral nutrition and exposure to piperacillin-tazobactam, admission during the mixing periods showed a trend towards association with the acquisition of cephalosporin resistance (OR 2.33, 95% CI 0.95–5.68).
Emergence of resistance after exposure and non-exposure of susceptible isolates to the different antipseudomonal agents
The risk of resistance emergence in patients previously colonized with susceptible strains of P. aeruginosa after exposure and non-exposure to the corresponding classes of antipseudomonal antibiotics is shown in Table 4. Exposure to any antibiotic, administered alone or in combination, was endowed with some risk for the emergence of resistance and, in this regard, combination therapy was apparently devoid of any preventive activity. Emergence of resistance was somewhat lower for piperacillin-tazobactam than for other antibiotics, although only the difference with carbapenems reached statistical significance (9 vs. 39%, P = 0.03). Five out of the eight courses of combination therapy which failed to prevent resistance were associated with the loss of susceptibility to the two components of the association. Resistance always arose after exposure to a given antibiotic for at least 3 days.
Emergence of resistance to quinolones and cephalosporins occurred at similar frequencies in patients exposed and not exposed to these agents, whereas carbapenem and amikacin resistance was clearly associated with the administration of these antibiotics.
Discussion
The present study provides some unique data concerning the putative role of antipseudomonal agents on their ability to promote P. aeruginosa colonization, acquisition of resistant strains and emergence of resistance in critically ill patients. In regards to the first outcome, our data suggest that quinolones and antipseudomonal cephalosporins may actually prevent the acquisition of P. aeruginosa, whereas piperacillin-tazobactam and amikacin may enhance it. With respect to the acquisition of resistance, we found that quinolones and cephalosporins were rather neutral, whereas all the other agents were associated with the acquisition of resistance to themselves or other antibiotics. Finally, emergence of resistance to any of the antipseudomonal agents certainly occurred after administering the corresponding antibiotic to patients previously colonized by susceptible strains, but for quinolones and cephalosporins this was not more frequent in patients who took the antimicrobial than in those who did not. Finally, the present data also suggest that emergence of resistance never arose to detectable levels before three days of continuous therapy and that combination treatment was not useful for prevention.
The role of systemic agents with antipseudomonal activity on the acquisition of P. aeruginosa in ICU patients has not been adequately explored. Our finding that some agents may have a significant preventive effect is not entirely unexpected. The impressive record of quinolones in preventing infections due to gram-negative bacilli, even in the surge of the current wave of resistance among common enteric bacilli and non-fermenters [36], is probably still due to their ability to decolonize mucosal surfaces and deter the acquisition of susceptible exogenous flora. It is more difficult to explain the discordant effect of antipseudomonal cephalosporins on one hand and piperacillin-tazobactam or amikacin on the other.
When acquisition of resistance to the different antipseudomonal agents is considered, the present data clearly diverge from those of other studies, particularly in regards to the role of quinolones. At least four studies have linked prior administration of quinolones with the acquisition of quinolone-resistant P. aeruginosa in either the gastrointestinal tract [3], any clinical sample [14, 19] or bloodstream isolates [15]. In addition, other investigations have shown an association between quinolone usage and resistance to piperacillin-tazobactam [31], imipenem [21, 25] and multidrug resistance [24, 29]. Although studies differ in design, and some have compared patients with resistant versus susceptible strains [14, 15, 19] (a strategy prone to magnify the risk associated with quinolone usage), it is difficult to ascertain the true reason for the discrepancy with the present data. It may rely, in part, on the predominant use of ciprofloxacin in our patients, a quinolone that, contrarily to levofloxacin, in some studies has not been associated with the acquisition of quinolone-resistant P. aeruginosa [13, 20, 37]. On the other hand, our sampling procedure, being more frequent and thorough than that of other studies, not only increased the chances of detecting P. aeruginosa but also provided a more accurate time estimation of the evaluated outcomes and the actual moment of antibiotic exposure in relation to them. The lack of association of quinolone usage with acquisition of resistance to carbapenems, piperacillin-tazobactam and amikacin may have been due, in part, to the small sample size. It must be remembered, however, that some studies have found quinolones to be protective against cephalosporin resistance in gram-negative bacilli, including P. aeruginosa [38].
The strategy of antibiotic use (mixing or cycling) was not influential in the acquisition of P. aeruginosa, but during mixing there was a non-significant trend towards an increased risk of resistance acquisition to cephalosporins. This is consistent with our previous observation that cycling was better than mixing in regards to the acquisition of P. aeruginosa resistant to selected β-lactams, particularly cefepime [32]. In the present study, enteral nutrition was the sole factor apparently associated with the acquisition of strains with a quinolone-resistant phenotype and was also an important predictor of the acquisition of strains resistant to cephalosporins and other antipseudomonal agents. Enteral feeding has been previously reported as an independent risk factor for multidrug resistance [24]. Although we do not have a plausible explanation for this finding, we think that enteral feeding could be a marker for some non-assessed variable involved in transmission.
Other associations found in the present study have been previously observed, such as the involvement of prior administration of imipenem and amikacin in imipenem resistance [9, 11, 18, 21], previous use of imipenem in piperacillin-tazobactam resistance [12], and prior exposure to piperacillin in ceftazidime resistance [26]. Our data also suggest that the use of carbapenems may predispose to the acquisition of amikacin resistance, and amikacin to quinolone resistance. Many, albeit not all of these associations can be explained by the selection of mutants overexpressing different multidrug efflux systems of the resistance-nodulation-division family [39]. However, studies aimed to correlate the specific mechanisms of resistance with prior antibiotic exposure are necessary to clarify this issue.
In the present study, emergence of resistance was observed after exposure to any of the antipseudomonal agents at frequencies within the range previously described in the literature. However, some intriguing differences were again noted between quinolones and cephalosporins on one hand and the remaining agents on the other. For all antibiotics we clearly documented that emergence of resistance occurred without exposure to the corresponding agent, which, in the case of quinolones and cephalosporins, was as common as in patients actually exposed. Although the number of treated patients was low, combination therapy did not seem to prevent the emergence of resistance, but the value of this strategy has never been consistently demonstrated in the clinical scenario [40].
Patients could end up carrying a strain resistant to a given antipseudomonal agent by acquisition of an already resistant isolate from other patients or an unknown source or by selection of resistance on a previously susceptible strain. The number of patients who acquired resistance due to cross-transmission of a resistant stain ranged from 0 for carbapenems and piperacillin-tazobactam to 6 (23%) for cephalosporins (Table 2). The respective roles of patient-to-patient transmission of a resistant clone and selection of resistance may depend on the proportion of other patients being colonized by strains resistant to the antibiotic considered (colonization pressure). In this study, however, colonization pressure was not associated with the acquisition of P. aeruginosa or of resistance. This may have been due to the relative few outcomes observed and to the low values of colonization pressure, which exceptionally were ≥0.5 [35].
The present study has several caveats, the most obvious being the relatively low number of observed outcomes of interest, hence many of the associations found should be confirmed in larger studies. On the other hand, the results may have been influenced by local epidemiological variables not applicable to other settings. Some of these potential confounders may include a relative high rate of horizontal transmission, almost universal exposure to antibiotics, preferential use of ciprofloxacin over levofloxacin and the frequent use of quinolones in combination regimens. In addition, we dealt with colonizing strains prospectively searched by an active sampling program, which could affect the clinical relevance of our observations.
In conclusion, the influence of antipseudomonal antibiotics on the risk of colonization by P. aeruginosa, acquisition of a resistant phenotype or the emergence of resistance of this pathogen depends on the particular antimicrobial agent. At least in some critical care settings, quinolones and antipseudomonal cephalosporins may actually prevent the acquisition of P. aeruginosa and may have a negligible effect on the acquisition and emergence of resistance.
References
Vincent JL (2003) Nosocomial infections in adult intensive-care units. Lancet 361:2068–2077
Bonten MJM, Bergmans DCJJ, Speijer H, Stobberingh EE (1999) Characteristics of polyclonal endemicity of Pseudomonas aeruginosa colonization in intensive care units. Implications for infection control. Am J Respir Crit Care Med 160:1212–1219
Lepelletier D, Caroff N, Riochet D, Bizouarn P, Bourdeau A, Le Gallou F, Esparze E, Reynaud A, Richet H (2006) Role of hospital stay and antibiotic use on Pseudomonas aeruginosa gastrointestinal colonization in hospitalized patients. Eur J Clin Microbiol Infect Dis 25:600–603
Rello J, Ausina V, Ricart M, Castella J, Prats G (1993) Impact of previous antimicrobial therapy on the etiology and outcome of ventilator-associated pneumonia. Chest 104:1230–1235
Trouillet JL, Chastre J, Vuagnat A, Joly-Guillou ML, Combaux D, Dombret MC, Gibert C (1998) Ventilator-associated pneumonia caused by potentially drug-resistant bacteria. Am J Respir Crit Care Med 157:531–539
Carmeli Y, Troillet N, Eliopoulos GM, Samore MH (1999) Emergence of antibiotic-resistant Pseudomonas aeruginosa: comparison of risks associated with different antipseudomonal agents. Antimicrob Agents Chemother 43:1379–1382
Fink MP, Snydman DR, Niederman MS, Leeper KV, Johnson RH, Heard SO, Wunderink RG, Caldwell JW, Schentag JJ, Siami GA, Zameck RL, Harverstock DC, Reinhart HH, Echols RM, the Severe Pneumonia Study Group (1994) Treatment of severe pneumonia in hospitalizae patients: result of a multicenter, randomized, double-blind trial comparing intravenous ciprofloxacin with imipenem-cilastatin. Antimicrob Agents Chemother 38:547–557
Zanetti G, Bally F, Greub G, Garbino J, Kinge T, Lew D, Romand JA, Bille J, Aymon D, Stratchounski L, Krawczyk L, Rubinstein E, Schaller MD, Chiolero R, Cometta A, The Cefepime Study Group (2003) Cefepime versus imipenem-cilastatin for treatment of nosocomial pneumonia in intensive care unit patients: a multicenter, evaluator-blind, prospective, randomized study. Antimicrob Agents Chemother 47:3442–3447
Troillet N, Samore MH, Carmeli Y (1997) Imipenem-resistant Pseudomonas aeruginosa: risk factors and antibiotic susceptibility patterns. Clin Infect Dis 25:1094–1098
El Amari EB, Chamot E, Auckenthaler R, Pechère JC, Van Delden C (2001) Influence of previous exposure to antibiotic therapy on the susceptibility pattern of Pseudomonas aeruginosa bacteremic isolates. Clin Infect Dis 33:1859–1864
Harris AD, Smith D, Johnson JA, Bradham DD, Roghmann MC (2002) Risk factors for imipenem-resistant Pseudomonas aeruginosa among hospitalized patients. Clin Infect Dis 34:340–345
Harris AD, Perencevich E, Roghmann MC, Morris G, Kaye KS, Johnson JA (2002) Risk factors for piperacillin-tazobactam-resistant Pseudomonas aeruginosa among hospitalized patients. Antimicrob Agents Chemother 46:854–858
Paladino JA, Sunderlin JL, Forrest A, Schentag JJ (2003) Characterization of the onset and consequences of pneumonia due to fluoroquinolone-susceptible or resistant Pseudomonas aeruginosa. J Antimicrob Chemother 52:457–463
Hsu DI, Okamoto MP, Murthy R, Wong-Beringer A (2005) Fluoroquinolone-resistant Pseudomonas aeruginosa: risk factors for acquisition and impact on outcomes. J Antimicrob Chemother 55:535–541
Kang CI, Kim SH, Park WB, Lee KD, Kim HB, Kim EC, Oh MD, Choe KW (2005) Risk factors for antimicrobial resistance and influence of resistance on mortality in patients with bloodstream infection caused by Pseudomonas aeruginosa. Microb Drug Resist 11:68–74
Ozkurt Z, Erteck M, Ero S, Altoparlak U, Akcay MN (2005) The risk for acquisition of imipenem-resistant Pseudomonas aeruginosa in the burn unit. Burn 31:870–873
Zavascki AP, Cruz RP, Goldani LZ (2005) Risk factors for imipenem-resistant Pseudomonas aeruginosa: a comparitive analysis of two case-control studies in hospitalized patients. J Hosp Infect 59:96–101
Fortaleza CM, Freire MP, Filho Dde C, de Carvalho Ramos M (2006) Risk factors for recovery of imipenem- or ceftazidime-resistant Pseudomonas aeruginosa among patients admitted to a teaching hospital in Brazil. Infect Control Hosp Epidemiol 27:901–906
Gasink LB, Fishman NO, Weiner MG, Nachmkin I, Bilker WB, Lautehnbach E (2006) Fluoroquinolone-resistant Pseudomonas aeruginosa: assessment of risk factors and clinical impact. Am J Med 119:526.e19–526.e25
Kaye KS, Kanafani ZA, Dodds AE, Engemann JJ, Weber SG, Carmeli Y (2006) Differential efects of levofloxacin and ciprofloxacin on the risk for isolation of quinolone-resistant Pseudomonas aeruginosa. Antimicrob Agents Chemother 50:2192–2196
Peña C, Guzmán A, Suarez C, Dominguez MA, Tubau F, Pujol M, Gudiol F, Ariza J (2007) Effects of carbapenem exposure on the risk for digestive tract carriage of intensive care unit-endemic carbapenem-resistant Pseudomonas aeruginosa strains in critically ill patients. Antimicrob Agents Chemother 51:1967–1971
Arruda EAG, Marinho IS, Boulos M, Sinto SI, Caiaffa HH, Mendes CM, Oplustil CP, Sader H, Levy CE, Levin AS (1999) Nosocomial infections caused by multiresistant Pseudomonas aeruginosa. Infect Control Hosp Epidemiol 20:620–623
Cao B, Wang H, Sun H, Zhu Y, Chen M (2004) Risk factors and clinical outcomes of nosocomial multi-drug resistant Pseudomonas aeruginosa infections. J Hosp Infect 57:112–118
Defez C, Fabbro-Peray P, Bouziges N, Gouby A, Mahamat A, Daurès JP, Sotto A (2004) Risk factors for multidrug-resistant Pseudomonas aeruginosa nosocomial infection. J Hosp Infect 57:209–216
Lauthenbach E, Weiner MG, Nachamkin I, Bilker WB, Sheridan A, Fishman NO (2006) Imipenem resistance among Pseudomonas aeruginosa isolates: risk factors for infection and impact of resistance on clinical and economic outcomes. Infec Control Hosp Epidemiol 27:893–900
Lee SC, Fung CP, Liu PYF, Wang TC, See LC, Lee N, Chen SC, Shieh WB (1999) Nosocomial infections with ceftazidime-resistant Pseudomonas aeruginosa: risk factors and outcome. Infect Control Hosp Epidemiol 20:205–207
Ohmagari N, Hanna H, Graviss L, Hackett B, Perego C, Gonzalez V, Dvorak T, Hogan H, Hachem R, Rolston K, Raad I (2005) Risk factors for infections with multidrug-resistant Pseudomonas aeruginosa in patients with cancer. Cancer 104:205–212
Ortega B, Groeneveld ABJ, Schultsz C (2004) Endemic multidrug-resistant Pseudomonas aeruginosa in critically ill patients. Infect Control Hosp Epìdemiol 25:825–831
Paramythiotou E, Lucet JC, Timsit JF, Vanjak D, Paugam-Burtz C, Trouillet JL, Belloc S, Kassis N, Karabinis A, Andremont A (2004) Acquisition of multidrug-resistant Pseudomonas aeruginosa in patients in intensive care units: role of antibiotics with antipseudomoal activity. Clin Infect Dis 38:670–677
Philippe E, Weiss M, Schultz JM, Yeomans F, Ehrenkranz NJ (1999) Emergence of highly antibiotic-resistant Pseudomonas aeruginosa in relation to duration of empirical antipseudomonal antibiotic treatment. Clin Perform Qual Health Care 7:83–87
Trouillet JL, Vuagnat A, Combes A, Kassis N, Chastre J, Gibert C (2002) Pseudomonas aeruginosa ventilator-associated pneumonia: comparison of episodes due to piperacillin-resistant versus piperacillin-susceptible organisms. Clin Infect Dis 34:1047–1054
Martinez JA, Nicolas JM, Marco F, Horcajada JP, Garcia-Segarra G, Trilla A, Codina C, Torres A, Mensa J (2006) Comparison of antimicrobial cycling and mixing strategies in two medical intensive care units. Crit Care Med 34:329–336
Clinical and Laboratory Standard Institute. Performance standards for antimicrobial susceptibility testing; sixteenth informational supplement (2006) Document M100-S16. Wayne, Pennsylvania
Gautom RK (1997) Rapid pulsed-field gel electrophoresis protocol for typing of Escherichia coli O157:H7 and other gram-negative organisms in 1 day. J Clin Microbiol 35:2977–2980
Bonten MJM, Slaugther S, Ambergen AW, Hayden MK, von Voorhis J, Nathan C, Weinstein RA (1998) The role of “colonization pressure” in the spread of vancomycin-resistant enterococci. Arch Intern Med 158:1127–1132
Bucaneve G, Micozzi A, Menichetti F, Martino P, Dionisi MS, Martinelli G, Allione B, D’Antonio D, Buelli M, Nosari AM, Cilloni D, Zuffa E, Cantaffa R, Specchia G, Amadori S, Fabbiano F, Deliliers GL, Lauria F, Foa R, Del Favero A, Gruppo Italiano Malattie Ematologiche dell’Adulto (GIMEMA) Infection Program (2005) Levofloxacin to prevent bacterial infection in patients with cancer and neutropenia. N Engl J Med 353:977–987
Polk RE, Johnson CK, McClish D, Wenzel RP, Edmond MB (2004) Predicting hospital rates of fluoroquinolone-resistant Pseudomonas aeruginosa from fluoroquinolone use in US hospitals and their surrounding communities. Clin Infect Dis 39:497–503
Schwaber MJ, Cosgrove SE, Gold HS, Kaye KS, Carmeli Y (2004) Fluoroquinolones protective against cephalosporin resistance in gram-negative nosocomial pathogens. Em Infect Dis 10:94–99
Ziha-Zarifi I, Llanes C, Kohler T, Pechere JC, Plesiat P (1999) In vivo emergence of multidrug-resistant mutants of Pseudomonas aeruginosa overexpressin the active efflux system MexA-MexB-OprM. Antimicrob Agents Chemother 43:287–291
Bliziotis IA, Samonis G, Vardakas KZ, Chrysanthopoulou S, Falagas ME (2005) Effect of aminoglycoside and beta-lactam combination therapy versus beta-lactam monotherapy on the emergence of antimicrobial resistance: a meta-analysis of randomized, controlled trials. Clin Infect Dis 41:149–158
Acknowledgments
This work was supported by a grant from the Agencia d’Avaluació i Recerca Médiques de la Generalitat de Catalunya (019/02/2000).
Conflict of interest statement
Dr. JA Martínez has received honoraria from Bayer and Pfizer, Dr. J Mensa has received honoraria from Bayer, Pfizer, Aventis and MSD, and Dr. A Torres has received honoraria from MSD. All other authors have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Martínez, J.A., Delgado, E., Martí, S. et al. Influence of antipseudomonal agents on Pseudomonas aeruginosa colonization and acquisition of resistance in critically ill medical patients. Intensive Care Med 35, 439–447 (2009). https://doi.org/10.1007/s00134-008-1326-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-008-1326-y