Abstract
Objective
To evaluate arginine vasopressin (AVP) and copeptin plasma concentrations in patients with vasodilatory shock after cardiac surgery.
Design
Prospective, controlled, clinical study.
Setting
Surgical intensive care unit and cardiac surgery ward in a tertiary university teaching hospital.
Patients and participants
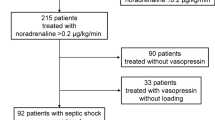
Thirty-three critically ill patients with vasodilatory shock after cardiac surgery and ten control patients undergoing uncomplicated aorto-coronary bypass surgery.
Measurements and results
Hemodynamic, laboratory and clinical data were recorded daily in all patients during the first 7 days after cardiac surgery. At the same time, points blood was withdrawn to determine plasma concentrations of AVP (radioimmunoassay) and copeptin (immunoluminometric assy). Standard tests, a mixed effects model and regression analyses were used for statistical analysis. The course of AVP was significantly different between groups (P < 0.001). While AVP concentrations were lower in the study group on the first postoperative day, they were higher than that in the control group from postoperative day 3 on. There was no difference in the postoperative AVP response between study patients with or without chronic angiotensin-converting enzyme inhibitor therapy. Except during continuous veno-venous hemofiltration, AVP and copeptin correlated significantly with each other (P < 0.001; r = 0.749).
Conclusions
The AVP response to cardiac surgery is significantly different between patients with vasodilatory shock and patients undergoing uncomplicated aorto-coronary bypass surgery. Although no causative relationship between AVP concentrations and cardiovascular instability can be drawn from these results, our data support the hypothesis that inadequately low AVP plasma levels contribute to the failure to restore vascular tone in vasodilatory shock after cardiac surgery.



Similar content being viewed by others
References
St André AC, Del Rossi A (2005) Hemodynamic management of patients in the first 24 h after cardiac surgery. Crit Care Med 33:2082–2093
Laffey JG, Boylan JF, Cheng DC (2002) The systemic inflammatory response to cardiac surgery: implications for the anesthesiologist. Anesthesiology 97:215–252
Dunser MW, Mayr AJ, Ulmer H, Ritsch N, Knotzer H, Pajk W, Mutz NJ, Hasibeder WR (2001) The effects of vasopressin on systemic hemodynamics in catecholamine-resistant septic and postcardiotomy shock: a retrospective analysis. Anesth Analg 93:7–13
Morales DL, Gregg D, Helman DN, Williams MR, Naka Y, Landry DW, Oz MC (2000) Arginine vasopressin in the treatment of 50 patients with postcardiotomy vasodilatory shock. Ann Thorac Surg 69:102–106
Dunser MW, Mayr AJ, Stallinger A, Ulmer H, Ritsch N, Knotzer H, Pajk W, Mutz NJ, Hasibeder WR (2002) Cardiac performance during vasopressin infusion in postcardiotomy shock. Intensive Care Med 28:746–751
Argenziano M, Choudhri AF, Oz MC, Rose EA, Smith CR, Landry DW (1997) A prospective randomized trial of arginine vasopressin in the treatment of vasodilatory shock after left ventricular assist device placement. Circulation 96(9 Suppl):II-286–II-290
Landry DW, Oliver JA (2001) The pathogenesis of vasodilatory shock. N Engl J Med 345:588–595
Luckner G, Dünser MW, Jochberger S, Mayr VD, Wenzel V, Ulmer H, Schmid S, Knotzer H, Pajk W, Hasibeder W, Mayr AJ, Friesenecker B (2005) Arginine vasopressin in 316 patients with advanced vasodilatory shock. Crit Care Med 33:2659–2666
Jochberger S, Mayr VD, Luckner G, Wenzel V, Ulmer H, Schmid S, Knotzer H, Pajk W, Hasibeder W, Friesenecker B, Mayr AJ, Dunser MW (2006) Serum vasopressin concentrations in critically ill patients. Crit Care Med 34:293–299
Jochberger S, Mayr VD, Luckner G, Torgersen C, Hasibeder WR, Dunser MW (2007) Vasopressin plasma concentrations in postcardiotomy shock: a prospective, controlled trial. Intensive Care Med 33(Suppl 2):A0763
Keats AS (1978) The ASA classification of physical status–a recapitulation. Anesthesiology 49:233–236
Le Gall JR, Lemeshow S, Saulnier F (1993) A new simplified acute physiologic score (SAPS II) based on a European/North American multicenter study. JAMA 270:2957–2963
Cotter G, Moshkovitz Y, Kaluski E, Milo O, Nobikov Y, Schneeweiss A, Krakover R, Vered Z (2003) The role of cardiac power and systemic vascular resistance in the pathophysiology and diagnosis of patients with acute congestive heart failure. Eur J Heart Fail 5:443–451
Goris RJ, te Boekhorst TP, Nuytinck JK, Gimbrère JS (1985) Multiple-organ failure. Generalized autodestructive inflammation? Arch Surg 120:1109–1115
Beardwell CG (1971) Radioimmunoassay of arginine vasopressin in human plasma. J Clin Endocrinol Metab 33:254–260
Morgenthaler NG, Struck J, Alonso C, Bergmann A (2006) Assay for the measurement of copeptin, a stable peptide derived from the precursor of vasopressin. Clin Chem 52:112–119
Woods WG, Forsling ML, Le Quesne LP (1989) Plasma arginine vasopressin levels and arterial pressure during open heart surgery. Br J Surg 76:29–32
Guyton AC, Hall JE (2000) The posterior pituitary gland and its relation to the hypothalamus. In: Guyton AC, Hall JE (eds) Textbook of medical physiology. W·B. Saunders, Philadelphia, pp 854–857
Landgraf R, Neumann I, Holsboer F, Pittman QJ (1995) Interleukin-1 beta stimulates both central and peripheral release of vasopressin and oxytocin in the rat. Eur J Neurosci 7:592–598
Raber J, Bloom FE (1994) IL-2 induces vasopressin release from the hypothalamus and the amygdale: role of nitric oxide-mediated signalling. J Neurosci 14:6187–6195
Ruthberg H, Hakanson E, Anderberg B, Jorfeldt L, Schildt B, Tegler L (1984) Thyroid hormones, catecholamine and cortisol concentrations after upper abdominal surgery. Acta Chir Scand 150:273–278
Lindner KH, Strohmenger HU, Ensinger H, Hetzel WD, Ahnefeld FW, Georgieff M (1992) Stress hormone response during and after cardiopulmonary resuscitation. Anesthesiology 77:662–668
Westermann I, Dunser MW, Haas T, Jochberger S, Luckner G, Mayr VD, Wenzel V, Stadlbauer KH, Innerhofer P, Morgenthaler NG, Hasibeder WR, Voelckel WG (2007) Endogenous vasopressin and copeptin response in multiple trauma patients. Shock 28(6):644–649
Schmidt HB, Werdan K, Müller-Werdan U (2001) Autonomic dysfunction in the ICU patient. Curr Opin Crit Care 7:314–322
Carnio EC, Stabile AM, Batalhao ME, Silva JS, Antunes-Rodrigues J, Branco LG, Magder S (2005) Vasopressin release during endotoxaemic shock in mice lacking inducible nitric oxide synthase. Pflugers Arch 450:390–394
Sharshar T, Carlier R, Blanchard A, Feydy A, Gray F, Paillard M, Raphael JC, Gajdos P, Annane D (2002) Depletion of neurohypophyseal content of vasopressin in septic shock. Crit Care Med 30:497–500
Leng G, Brown CH, Russell JA (1999) Physiological pathways regulating the activity of magnocellular neurosecretory cells. Prog Neurobiol 57:625–655
Day TA, Randle JC, Renaud LP (1985) Opposing α- and β-adrenergic mechanisms mediate dose-dependent actions of norepinephrine on supraoptic vasopressin neurons in vivo. Brain Res 358:171–179
Pfeiffer A, Herz A (1984) Endocrine actions of opioids. Horm Metab Res 16:386–397
Gotloib L, Barzilay E, Shustak A, Waiss Z, Lev A (1985) Hemofiltration in severe septic adult respiratory distress syndrome associated with varicella. Intensive Care Med 11:319–322
Argenziano M, Chen JM, Choudhri AF, Culminane S, Garfein E, Weinberg AD, Smith CR Jr, Rose EA, Landry DW, Oz MC (1998) Management of vasodilatory shock after cardiac surgery: identification of predisposing factors and use of a novel pressor agent. J Thorac Cardiovasc Surg 116:973–980
Brabant SM, Bertrand M, Eyraud D, Darmon PL, Coriat P (1999) The hemodynamic effects of anesthetic induction in vascular surgical patients chronically treated with angiotensin II receptor antagonists. Anesth Analg 89:1388–1392
Jochberger S, Morgenthaler NG, Mayr VD, Luckner G, Wenzel V, Ulmer H, Schwarz S, Hasibeder WR, Friesenecker BE, Dünser MW (2006) Copeptin and arginine vasopressin concentrations in critically ill patients. J Clin Endocrinol Metab 91:4381–4386
Acknowledgments
Supported by the Austrian National Bank, Science Project No. 11343, Vienna, Austria. Nils G. Morgenthaler works at the Department of Research of the B.R.A.H.M.S. company, which has developed and patented the copeptin assay. No other author has a conflict of interest in regards of drugs or assays discussed in this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jochberger, S., Velik-Salchner, C., Mayr, V.D. et al. The vasopressin and copeptin response in patients with vasodilatory shock after cardiac surgery: a prospective, controlled study. Intensive Care Med 35, 489–497 (2009). https://doi.org/10.1007/s00134-008-1279-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-008-1279-1