Abstract
Objective
To investigate the possible impact of obesity on morbidity and mortality in intensive care unit (ICU) patients included in the European observational sepsis occurrence in acutely ill patients (SOAP) study.
Design
Planned substudy from the SOAP database.
Setting
One hundred and ninety-eight ICUs in 24 European countries.
Patients
All patients admitted to one of the participating ICUs. Patients were classified, according to their body mass index (BMI), as underweight (<18.5 kg/m2), normal weight (18.5–24.9 kg/m2), overweight (25–29.9 kg/m2), obese (30–39.9 kg/m2), and very obese (≥40 kg/m2).
Measurements and results
The BMI was available in 2,878 (91%) of the 3,147 patients included in the SOAP study; 120 patients (4.2%) were underweight, 1,206 (41.9%) had a normal BMI, 1,047 (36.4%) were overweight, 424 (14.7%) were obese, and 81 (2.8%) were very obese. Obese and very obese patients more frequently developed ICU-acquired infections than patients in lower BMI categories. Very obese patients showed a trend towards longer ICU [median (IQ): 4.1 (1.8–12.1) vs. 3.1 (1.7–7.2) days, P = 0.056) and hospital lengths of stay [14.3 (8.4–27.4) vs. 12.3 (5.1–24.4), days P = 0.077] compared to those with a normal BMI. However, there were no significant differences among the groups in ICU or hospital mortality rates. In a multivariate Cox regression analysis, none of the BMI categories was associated with an increased risk of 60-day in-hospital death.
Conclusion
BMI did not have a significant impact on mortality in this mixed population of ICU patients.
Similar content being viewed by others
Introduction
Excess body weight has long been recognised as a harbinger of disease and early death in the general population [1–6]. In addition to the psychological and social difficulties often faced by overweight people, obese individuals are more susceptible to medical complications, including hypertension, type 2 diabetes mellitus, cardiovascular disease, pulmonary disease, and cancer [1–6]. Many epidemiological studies have demonstrated that obesity is associated with higher morbidity and mortality rates in the general population [7–9].
Management of obese patients in the intensive care unit (ICU) may present additional practical challenges [10, 11]. For example, the distribution, metabolism, protein binding, and clearance of many drugs are altered in these patients [12, 13]. Mechanical ventilation is also hampered by the reduction in compliance of the lung and chest wall and increased airway resistance [14] and weaning from the ventilator may be more difficult in obese patients [10], probably as a result of increased work of breathing when changing from positive pressure ventilation to spontaneous breathing [15]. The risk of ventilator-associated pneumonia (VAP) is also increased in severely obese patients [16], probably because of the higher gastric volume, lower normal pH of gastric fluids in fasting obese patients, increased intraabdominal pressure, and a higher incidence of gastric reflux [17, 18]. Deep venous thromboses, pulmonary embolism, and cardiovascular complications are also increased in obese patients [19].
With an increase in the number of overweight and obese patients being admitted to the ICU, the attributable morbidity and mortality of obesity has become a concern for the intensivist. Several studies on acutely or critically ill patients have investigated the effect of obesity on outcome [20–31]. These studies, the majority of which have been performed in the United States, have yielded conflicting results. The epidemiology of obesity in the ICU and the possible relationship between obesity and outcome of ICU patients has not previously been reported in a multicentre European study.
We investigated the possible impact of obesity, as assessed by the body mass index (BMI), on morbidity and mortality in ICU patients included in the sepsis occurrence in acutely ill patients (SOAP) study [32].
This study has been partially presented previously in abstract form [33].
Methods
The SOAP study was a prospective, multicentre, observational study designed to evaluate the epidemiology of sepsis, as well as other characteristics of ICU patients in European countries. Recruitment, data collection, and management are detailed elsewhere [32]. Briefly, all patients above 15 years, admitted to the 198 participating centres (see the “Appendix” for a list of participating countries and centres) between 1 May and 15 May 2002 were included, except patients who stayed in the ICU for less than 24 h for routine postoperative observation. Patients were followed up until death, hospital discharge, or for 60 days. Due to the observational nature of the study, institutional review board approval was either waived or expedited in participating institutions and informed consent was not required.
Data were collected prospectively using pre-printed case report forms. Data collection on admission included demographic data and comorbidities. Clinical and laboratory data for the simplified acute physiology (SAPS) II score [34] were reported as the worst value within 24 h after admission. Microbiologic and clinical infections were reported daily as well as the antibiotics administered. A daily evaluation of organ function according to the sequential organ failure assessment (SOFA) score [35] was performed, with the most abnormal value for each of the six organ systems (respiratory, renal, cardiovascular, hepatic, coagulation, and neurological) collected on admission and every 24 h thereafter. Sepsis was defined according to consensus conference definitions [36]. Organ failure was defined as a SOFA score >2 for the organ in question [37]. Severe sepsis was defined as sepsis with at least one organ failure.
Weight and height were calculated from actual measurements or, when not available, from the best clinical estimate by the patient’s care provider. The degree of obesity was assessed by the BMI using the formula: BMI = body weight (kg)/height2 (m2) [38]. We classified the patients, according to the definitions of the National Institutes of Health and World Health Organisation criteria for BMI [38], as underweight (<18.5 kg/m2), normal weight (18.5–24.9 kg/m2), overweight (25–29.9 kg/m2), obese (30–39.9 kg/m2), and very obese (≥40 kg/m2).
The a-priori defined outcome parameters for this analysis included the degree of organ dysfunction/failure as assessed by the SOFA score, the occurrence of sepsis syndromes and organ failure in the ICU, hospital and ICU lengths of stay, and all cause hospital and ICU mortality.
Statistical methods
Data were analysed using SPSS 12.0 for Windows (SPSS Inc, Chicago, IL). The Kolmogorov–Smirnov test was used to verify the normality of distribution of continuous variables. Non-parametric tests of comparison were used for variables evaluated as not normally distributed. Difference testing between the groups was performed using a Kruskal Wallis H test, Mann–Whitney U test, Chi square test, and Fisher exact test as appropriate. A Bonferroni correction was done for multiple comparisons. SAPS II adjusted odds ratios (OR) [95% confidence interval (CI)] for in-hospital mortality were computed using logistic regression. Kaplan–Meier survival curves were plotted and compared using a signed log Rank test. We performed a multivariate Cox proportional hazard model with time to in-hospital death right censored at 60 days as the dependent factor in the overall population, to avoid a positive effect on LOS from early mortality. Variables included in the Cox regression analysis were age, gender, comorbid diseases, SAPS II and SOFA scores on admission, the type of admission (medical or surgical), the presence of sepsis, and the need for mechanical ventilation or renal replacement therapy during the ICU stay. Variables were introduced in the model if significantly associated with a higher risk of 60-day in-hospital death on a univariate basis at a P-value <0.2. Colinearity between the variables was excluded prior to modelling. The time dependent covariate method was used to check the proportional hazard assumption of the model; an extended Cox model was constructed, adding interaction terms that involve time, i.e. time dependent variables, computed as the by-product of time and individual covariates in the model (time × covariate), individual time dependent covariates were introduced one by one and in combinations in the extended model, none of which was found to be significant (Wald Chi-square statistics). A forward stepwise approach was used and BMI was forced as the last step in the model, after adjustment for other factors, as a categorical variable with normal BMI as the reference category. We tested for a possible country effect by introducing the country of origin as a categorical variable in the final model, with the country with the lowest mortality rates and sufficient sample size (Germany) as a reference category.
Continuous data are presented as mean ± SD and categorical as number (%), unless otherwise indicated. All statistics were two-tailed and a P < 0.05 was considered to be statistically significant.
Results
Characteristics of the study group
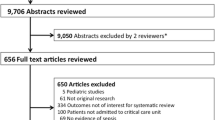
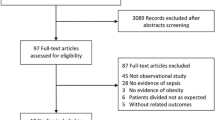
BMI was reported in 2,878 (study group, mean age 60.8 ± 17.3 years, 62.3% male) of the 3,147 patients included in the SOAP study. Table 1 presents the characteristics of the study group on admission to the ICU. The distribution of the various BMI categories varied among the contributing countries (Fig. 1). The mean BMI was 26.1 ± 5.8 kg/m2 (Fig. 2; range 12.2–80.0 kg/m2). A total of 1,672 patients (58.1%) had an abnormal BMI: 120 patients (4.2%) were underweight, 1,047 (36.4%) were overweight, 424 (14.7%) obese, and 81 (2.8%) very obese. Overweight and obese patients were older (63.6 ± 15.0 and 63.5 ± 14.1 vs. 58.4 ± 19.1 years, respectively, each P < 0.01) and underweight patients were younger (52.6 ± 21.0 vs. 58.4 ± 19.1 years, p < 0.05) than patients with normal BMI. Very obese (61.7 vs. 38.1%, P < 0.01) and underweight (53.2 vs. 38.1%, P < 0.05) patients were more commonly female when compared with the patients with normal BMI. The source and type of admission, medical versus surgical status, and incidence of sepsis syndromes on admission to the ICU were similar regardless of the BMI. The SOFA score (3.7 ± 3.3 vs. 5.1 ± 3.7, P < 0.01) and the incidence of respiratory failure (12.5 vs. 20.8%, P < 0.01) were lower on admission to the ICU in underweight patients than in patients with normal BMI.
Morbidity
Obese and very obese patients more often developed ICU-acquired infections; however, the overall incidence of sepsis syndromes during the ICU stay was similar among the groups (Table 2). The overall incidence of respiratory failure and mechanical ventilation occurring at some point during the ICU stay increased significantly with increasing BMI category, likely because of a higher occurrence of respiratory failure with increasing BMI category on admission to the ICU. The incidence of new organ dysfunction during the ICU stay was similar among the groups. The maximum (5.2 ± 4.1 vs. 6.5 ± 4.3, P < 0.01) and the mean (3.5 ± 3.1 vs. 4.5 ± 3.4, P < 0.01) SOFA scores during the ICU stay were lower in underweight patients than that in patients with normal BMI.
Very obese patients showed a trend towards longer ICU (median [IQ]: 4.1 (1.8–12.1) vs. 3.1 (1.7–7.2), days, P = 0.06) and hospital [14.3 (8.4–27.4) vs. 12.3 (5.1–24.4), days, P = 0.08) lengths of stay when compared with those with a normal BMI (Fig. 3).
Mortality
The overall ICU and hospital mortality rates for the entire population were 18.1 and 23.5%, respectively. ICU and hospital mortality rates were unrelated to BMI (Table 2). A Kaplan Meier survival analysis showed similar survival patterns in the different groups (Fig. 4). The SAPS II adjusted odds ratio of in-hospital mortality (with normal BMI as a reference group) was 1.27 [95% confidence interval (CI): 0.75–2.14, P = 0.371] in underweight patients, 0.96 (95% CI: 0.76–1.21, P = 0.74) in overweight, 0.9 (95% CI: 0.66–1.22, P = 0.483) in obese, and 1.15 (95% CI: 0.62–2.13, P = 0.650) in the very obese (Table 3). The SAPS II adjusted odds ratio for hospital mortality was not significantly increased in any of the BMI categories compared with normal BMI in a subgroup analysis stratifying patients according to sex, age, the presence of sepsis, septic shock, or shock due to any cause, the type of admission (medical or surgical), and ICU length of stay of more or less than 2 days (Table 3). In the subgroup of patients who were mechanically ventilated for more than 2 days, there was a trend towards higher mortality in underweight patients when compared to those with normal BMI (SAPS II adjusted odds ratio: 1.84, 95% CI: 0.94–3.61, P = 0.077).
Kaplan Meier survival curves stratified according to body mass index; underweight (<18.5 kg/m2), normal (18.5–24.9 kg/m2), overweight (25–29.9 kg/m2), obese (30–39.9 kg/m2), and very obese (≥40 kg/m2). Log Rank (compared with normal BMI): underweight = 0.4 (P = 0.525), overweight = 0.14 (P = 0.705), obese = 0.297 (P = 0.586), and very obese = 2.17 (P = 0.141)
In a multivariate Cox regression analysis, none of the BMI categories was associated with an increased risk of 60-day in-hospital death (Table 4). Older age, medical admissions, a diagnosis of haematological cancer or cirrhosis, SAPS II score, and SOFA score on admission to the ICU, and the need for mechanical ventilation during the ICU stay were independently associated with an increased risk of 60-day in-hospital death.
Discussion
In this large cohort of ICU patients, obesity was associated with increased morbidity as patients with higher BMI more often developed ICU-acquired infections. There was also a trend towards longer ICU and hospital lengths of stay in very obese patients when compared with those of normal BMI. However, obesity was not associated with increased mortality.
In obese patients, despite a greater prevalence of comorbid conditions and the liability to develop physiologic derangement that may impair their ability to compensate for the stress of critical illness [16, 39], an independent effect of obesity on outcome from critical illness has never been conclusively demonstrated. In a retrospective review [40] of the study to understand prognoses and preferences for outcomes and risks of treatment (SUPPORT), a low BMI, but not a high BMI, was a significant and independent predictor of mortality. Likewise, Tremblay and Bandi [21] found an increased mortality rate in underweight patients but not in overweight, obese, or severely obese patients included in a large national cooperative database (n = 41,011). Two single-centre French studies investigated the possible influence of BMI on outcome in ICU patients. In a prospective study by Goulenok et al. [22], a BMI greater than 27 kg/m2 was predictive of increased mortality. Obesity was associated with longer ICU stays, increased severity of illness, and higher mortality rates. This study [22] was limited by the relatively small sample size (n = 813) and the criteria used to classify patients. In a matched cohort study, Bercault et al. [11] found that obesity was significantly associated with ICU mortality, especially in younger patients and in patients with a probability of death of 11–50%. The authors observed that obese patients had a fourfold increase in the likelihood of developing nosocomial infections and other ICU-related complications. Others have reported no effect of obesity on short [26] or long-term [27] mortality rates, and a recent meta-analysis of 14 studies concluded that obesity is not associated with excess mortality but is significantly related to prolonged duration of mechanical ventilation and ICU length of stay [41].
The impact of obesity may depend on the specific population of patients. In a subset of surgical ICU patients with an ICU LOS ≥4 days (n = 406), admitted to one centre included in the IMPACT project, Nasraway et al. [30] recently reported that ICU and hospital mortality rates were increased in morbidly obese, critically ill surgical patients (BMI ≥ 40 kg/m2) when compared with the patients with a normal BMI and that morbid obesity was an independent risk factor for death in these patients. However, the reference group included underweight and obese patients, limiting the interpretation of these data. In critically ill trauma patients, Bochicchio et al. [25] reported that obese patients were 7.1 times more likely to die than non-obese patients after controlling for age, diabetes, gender, obesity, COPD, and injury severity score, and others have reported that obesity is an independent risk factor for death in critically ill blunt trauma patients [23, 31].
This is the first study reporting the distribution of BMI in a large cohort of European ICU patients. The incidence of abnormal BMI was lower in our study than in the reports from the United States [20, 24, 29, 30]; this may reflect general differences between European and USA populations [42]. In accordance with other literature [24, 30], very obese and underweight patients in our study were more commonly female. In contrast to some studies from the USA [29, 30], however, overweight and obese patients were older than patients with a normal BMI.
In our study, the incidence of respiratory failure and mechanical ventilation on admission to the ICU were greater in patients with higher BMI classes; however, the incidence of late-onset respiratory failure was similar among groups. The association between obesity and respiratory complications in the ICU has been described previously [43], although BMI does not appear to be a predictive factor for post-operative pulmonary complications [44]. Severely obese patients may have underlying ventilation–perfusion mismatch with a greater incidence of basal atelectasis causing hypoxaemia [45], abnormalities in control of breathing, and a higher prevalence of sleep apnoea syndrome [46, 47]. Obesity has been reported to increase respiratory muscle oxygen demand, with more oxygen being consumed for any given task compared to patients with normal weight [48]. This results in a decrease in performance, even in patients with normal lung function. In our study, the SAPS II adjusted odds ratio was not significantly increased in any of the BMI categories when compared with normal BMI in the whole cohort or in subgroup analysis. However, in patients who were mechanically ventilated for more than 2 days, we did find a trend towards a higher mortality in underweight patients compared with those with normal BMI. In a retrospective analysis of 1,488 patients with acute lung injury included in the project IMPACT database, O’Brien et al. [29] reported that a lower BMI was associated with a higher risk of death, whereas BMIs corresponding to overweight and obese were associated with a lower risk. However, in 902 mechanically ventilated patients who were enrolled in randomised, controlled trials of therapies for acute lung injury, overweight and obese patients had outcomes similar to those of patients with normal BMIs [49]. Morris et al. [50] reported that although BMI was not associated with mortality in patients with acute lung injury, severely obese patients had longer duration of mechanical ventilation and longer ICU lengths of stay than patients with normal BMI.
Patients with higher BMI more often developed ICU-acquired infections in our study. Nevertheless, the overall incidence of sepsis syndromes during the ICU stay was similar between the groups, precluding a negative influence of ICU-acquired infection on the net outcome. Other studies have reported an increased incidence of VAP and other nosocomial infections in obese patients [11, 16, 17, 25].
In agreement with previous studies [21, 23], we found that very obese patients had a trend towards longer ICU and hospital lengths of stay compared with patients of normal BMI. Given the lack of increased mortality in the obese and very obese patients in our study, the increased length of stay may be attributed to prolonged recovery from illness or to an increased incidence of non-fatal complications, and may, thus, be associated with an increase in consumption of medical resources in these patients.
There is a documented bias against obese individuals in health care settings [51, 52] that can affect care [53]. As obesity was not associated with a worse outcome in our study, this potential bias is unlikely to have been a major factor.
Our study has some limitations. First, body weight and height were not consistently measured according to our study protocol. This imprecision is quite common [21, 29, 30, 49], and most ICU practitioners will acknowledge that weight and height are often estimated rather than measured [21]. Second, body weight at the time of ICU admission may be significantly different from a patient’s normal body weight because of volume depletion or overload; recent changes in BMI could not be taken into account and may have played a role in determining outcomes. These data are difficult to quantify and adjust for, even in prospectively designed studies [11]. Third, we are unable to determine how many of the obese patients were admitted to the ICU because they were obese, and would not have needed admission if their BMI had been normal. Similarly, we are unable to determine whether the longer ICU stays in very obese patients were related to ongoing disease or logistic difficulties, with discharge related to their high BMI. Fourth, we did not collect data on tracheostomy or weaning processes, or on specific mechanical ventilatory settings, which can be different in obese patients and may influence outcomes. Fifth, the multivariate analysis we performed is limited by the variables included. However, we adjusted for a fairly large number of variables which are known to influence the outcome prediction.
In conclusion, BMI did not have any significant impact on mortality in a large heterogeneous group of ICU patients in Europe. Patients with higher BMI developed ICU-acquired infections more frequently than those with normal BMI. A trend towards longer ICU and hospital lengths of stay in very obese patients compared to those with normal BMI suggests that such patients may have a higher consumption of medical resources.
References
Flegal KM, Carroll MD, Ogden CL, Johnson CL (2002) Prevalence and trends in obesity among US adults, 1999–2000. JAMA 288:1723–1727
Katzmarzyk PT, Janssen I, Ardern CI (2003) Physical inactivity, excess adiposity and premature mortality. Obes Rev 4:257–290
Willett WC, Dietz WH, Colditz GA (1999) Guidelines for healthy weight. N Engl J Med 341:427–434
McGee DL (2005) Body mass index and mortality: a meta-analysis based on person-level data from twenty-six observational studies. Ann Epidemiol 15:87–97
Adams KF, Schatzkin A, Harris TB, Kipnis V, Mouw T, Ballard-Barbash R, Hollenbeck A, Leitzmann MF (2006) Overweight, obesity, and mortality in a large prospective cohort of persons 50 to 71 years old. N Engl J Med 355:763–778
Yan LL, Daviglus ML, Liu K, Stamler J, Wang R, Pirzada A, Garside DB, Dyer AR, Van Horn L, Liao Y, Fries JF, Greenland P (2006) Midlife body mass index and hospitalization and mortality in older age. JAMA 295:190–198
Hedlund J, Hansson LO, Ortqvist A (1995) Short- and long-term prognosis for middle-aged and elderly patients hospitalized with community-acquired pneumonia: impact of nutritional and inflammatory factors. Scand J Infect Dis 27:32–37
Calle EE, Thun MJ, Petrelli JM, Rodriguez C, Heath CW Jr (1999) Body-mass index and mortality in a prospective cohort of U.S. adults. N Engl J Med 341:1097–1105
Grady KL, White-Williams C, Naftel D, Costanzo MR, Pitts D, Rayburn B, VanBakel A, Jaski B, Bourge R, Kirklin J (1999) Are preoperative obesity and cachexia risk factors for postheart transplant morbidity and mortality: a multi-institutional study of preoperative weight–height indices. Cardiac transplant research database (CTRD) Group. J Heart Lung Transplant 18:750–763
Varon J, Marik P (2001) Management of the obese critically ill patient. Crit Care Clin 17:187–200
Bercault N, Boulain T, Kuteifan K, Wolf M, Runge I, Fleury JC (2004) Obesity-related excess mortality rate in an adult intensive care unit: a risk-adjusted matched cohort study. Crit Care Med 32:998–1003
Salazar DE, Corcoran GB (1988) Predicting creatinine clearance and renal drug clearance in obese patients from estimated fat-free body mass. Am J Med 84:1053–1060
Stokholm KH, Brochner-Mortensen J, Hoilund-Carlsen PF (1980) Increased glomerular filtration rate and adrenocortical function in obese women. Int J Obes 4:57–63
Pelosi P, Croci M, Ravagnan I, Vicardi P, Gattinoni L (1996) Total respiratory system, lung, and chest wall mechanics in sedated-paralyzed postoperative morbidly obese patients. Chest 109:144–151
Kress JP, Pohlman AS, Alverdy J, Hall JB (1999) The impact of morbid obesity on oxygen cost of breathing (VO(2RESP)) at rest. Am J Respir Crit Care Med 160:883–886
Vaughan RW, Conahan TJ III (1980) Part I: cardiopulmonary consequences of morbid obesity. Life Sci 26:2119–2127
Vaughan RW, Bauer S, Wise L (1975) Volume and pH of gastric juice in obese patients. Anesthesiology 43:686–689
Jacobson BC, Somers SC, Fuchs CS, Kelly CP, Camargo CA Jr (2006) Body-mass index and symptoms of gastroesophageal reflux in women. N Engl J Med 354:2340–2348
Darvall KA, Sam RC, Silverman SH, Bradbury AW, Adam DJ (2007) Obesity and thrombosis. Eur J Vasc Endovasc Surg 33:223–233
El Solh A, Sikka P, Bozkanat E, Jaafar W, Davies J (2001) Morbid obesity in the medical ICU. Chest 120:1989–1997
Tremblay A, Bandi V (2003) Impact of body mass index on outcomes following critical care. Chest 123:1202–1207
Goulenok C, Monchi M, Chiche JD, Mira JP, Dhainaut JF, Cariou A (2004) Influence of overweight on ICU mortality: a prospective study. Chest 125:1441–1445
Brown CV, Neville AL, Rhee P, Salim A, Velmahos GC, Demetriades D (2005) The impact of obesity on the outcomes of 1, 153 critically injured blunt trauma patients. J Trauma 59:1048–1051
Ray DE, Matchett SC, Baker K, Wasser T, Young MJ (2005) The effect of body mass index on patient outcomes in a medical ICU. Chest 127:2125–2131
Bochicchio GV, Joshi M, Bochicchio K, Nehman S, Tracy JK, Scalea TM (2006) Impact of obesity in the critically ill trauma patient: a prospective study. J Am Coll Surg 203:533–538
Aldawood A, Arabi Y, Dabbagh O (2006) Association of obesity with increased mortality in the critically ill patient. Anaesth Intensive Care 34:629–633
Peake SL, Moran JL, Ghelani DR, Lloyd AJ, Walker MJ (2006) The effect of obesity on 12-month survival following admission to intensive care: a prospective study. Crit Care Med 34:2929–2939
Alban RF, Lyass S, Margulies DR, Shabot MM (2006) Obesity does not affect mortality after trauma. Am Surg 72:966–969
O’Brien JM Jr, Phillips GS, Ali NA, Lucarelli M, Marsh CB, Lemeshow S (2006) Body mass index is independently associated with hospital mortality in mechanically ventilated adults with acute lung injury. Crit Care Med 34:738–744
Nasraway SA Jr, Albert M, Donnelly AM, Ruthazer R, Shikora SA, Saltzman E (2006) Morbid obesity is an independent determinant of death among surgical critically ill patients. Crit Care Med 34:964–970
Neville AL, Brown CV, Weng J, Demetriades D, Velmahos GC (2004) Obesity is an independent risk factor of mortality in severely injured blunt trauma patients. Arch Surg 139:983–987
Vincent JL, Sakr Y, Sprung CL, Ranieri VM, Reinhart K, Gerlach H, Moreno R, Carlet J, Le Gall JR, Payen D (2006) Sepsis in European intensive care units: results of the SOAP study. Crit Care Med 34:344–353
Sakr Y, de Pont AC, Lovstad RZ, Reinhart K, Vincent JL (2006) Does obesity in the ICU influence outcome? Intensive Care Med 32:58 (abstract)
Le Gall J-R, Lemeshow S, Saulnier F (1993) A new simplified acute physiology score (SAPS II) based on a European/North American multicenter study. JAMA 270:2957–2963
Vincent JL, Moreno R, Takala J, Willatts S, de Mendonça A, Bruining H, Reinhart CK, Suter PM, Thijs LG (1996) The SOFA (sepsis-related organ failure assessment) score to describe organ dysfunction/failure. Intensive Care Med 22:707–710
(1992) American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference: definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Crit Care Med 20:864–874
Vincent JL, de Mendonça A, Cantraine F, Moreno R, Takala J, Suter P, Sprung C, Colardyn FC, Blecher S (1998) Use of the SOFA score to assess the incidence of organ dysfunction/failure in intensive care units: results of a multicentric, prospective study. Crit Care Med 26:1793–1800
National Institutes of Health NHLBI Obesity Education Initiative Expert Panel (1998) Clinical guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults: the Evidence Report. US Department of Health and Human Services, Washington
Alpert MA, Hashimi MW (1993) Obesity and the heart. Am J Med Sci 306:117–123
Galanos AN, Pieper CF, Kussin PS, Winchell MT, Fulkerson WJ, Harrell FE Jr, Teno JM, Layde P, Connors AF Jr, Phillips RS, Wenger NS (1997) Relationship of body mass index to subsequent mortality among seriously ill hospitalized patients. SUPPORT investigators. The study to understand prognoses and preferences for outcome and risks of treatments. Crit Care Med 25:1962–1968
Akinnusi ME, Pineda LA, El Solh AA (2008) Effect of obesity on intensive care morbidity and mortality: a meta-analysis. Crit Care Med 36:151–158
Bray GA (1992) Pathophysiology of obesity. Am J Clin Nutr 55:488S–494S
Rose DK, Cohen MM, Wigglesworth DF, DeBoer DP (1994) Critical respiratory events in the postanesthesia care unit. Patient, surgical, and anesthetic factors. Anesthesiology 81:410–418
Smetana GW, Lawrence VA, Cornell JE (2006) Preoperative pulmonary risk stratification for noncardiothoracic surgery: systematic review for the American College of Physicians. Ann Intern Med 144:581–595
Ray CS, Sue DY, Bray G, Hansen JE, Wasserman K (1983) Effects of obesity on respiratory function. Am Rev Respir Dis 128:501–506
Vgontzas AN, Tan TL, Bixler EO, Martin LF, Shubert D, Kales A (1994) Sleep apnea and sleep disruption in obese patients. Arch Intern Med 154:1705–1711
Drenick EJ, Bale GS, Seltzer F, Johnson DG (1980) Excessive mortality and causes of death in morbidly obese men. JAMA 243:443–445
Burki NK, Baker RW (1984) Ventilatory regulation in eucapnic morbid obesity. Am Rev Respir Dis 129:538–543
O’Brien JM Jr, Welsh CH, Fish RH, Ancukiewicz M, Kramer AM (2004) Excess body weight is not independently associated with outcome in mechanically ventilated patients with acute lung injury. Ann Intern Med 140:338–345
Morris AE, Stapleton RD, Rubenfeld GD, Hudson LD, Caldwell E, Steinberg KP (2007) The association between body mass index and clinical outcomes in acute lung injury. Chest 131:342–348
Moreno R, Apolone G, Miranda DR (1998) Evaluation of the uniformity of fit of general outcome prediction models. Intensive Care Med 24:40–47
Patel PA, Grant BJ (1999) Application of mortality prediction systems to individual intensive care units. Intensive Care Med 25:977–982
Hebl MR, Xu J (2001) Weighing the care: physicians’ reactions to the size of a patient. Int J Obes Relat Metab Disord 25:1246–1252
Acknowledgments
The SOAP study was supported by an unlimited grant from Abbott, Baxter, Eli Lilly, GlaxoSmithKline, and NovoNordisk. These companies had no involvement at any stage of the study design, in the collection and analysis of data, in writing the manuscript, or in the decision to submit for publication.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is discussed in the editorial available at doi:10.1007/s00134-008-1244-z
Appendix
Appendix
Participants by country (listed alphabetically)
Austria: University Hospital of Vienna (G. Delle Karth); LKH Steyr (V. Draxler); LKH-Deutschlandsberg (G. Filzwieser); Otto Wagner Spital of Vienna (W. Heindl); Krems of Donau (G. Kellner, T. Bauer); Barmherzige Bruede of Linz (K. Lenz); KH Floridsdorf of Vienna (E. Rossmann); University Hospital of Innsbruck (C. Wiedermann); Belgium: CHU of Charleroi (P. Biston); Hôpitaux Iris Sud of Brussels (D. Chochrad); Clinique Europe Site St Michel of Brussels (V. Collin); C·H.U. of Liège (P. Damas); University Hospital Ghent (J. Decruyenaere, E. Hoste); CHU Brugmann of Brussels (J. Devriendt); Centre Hospitalier Jolimont-Lobbes of Haine St Paul (B. Espeel); CHR Citadelle of Liege (V. Fraipont); UCL Mont-Godinne of Yvoir (E. Installe); ACZA Campus Stuivenberg (M. Malbrain); OLV Ziekenhuis Aalst (G. Nollet); RHMS Ath-Baudour-Tournai (J.C. Preiser); AZ St Augustinus of Wilrijk (J. Raemaekers); CHU Saint-Pierre of Brussels (A. Roman); Cliniques du Sud-Luxembourg of Arlon (M. Simon); Academic Hospital Vrije Universiteit Brussels (H. Spapen); AZ Sint-Blasius of Dendermonde (W. Swinnen); Clinique Notre-Dame of Tournai (F. Vallot); Erasme University Hospital of Brussels (J.L. Vincent); Czech Republic: University Hospital of Plzen (I. Chytra); U SV.Anny of Brno (L. Dadak); Klaudians of Mlada Boleslav (I. Herold); General Faculty Hospital of Prague (F. Polak); City Hospital of Ostrava (M. Sterba); Denmark: Gentofte Hospital, University of Copenhagen (M. Bestle); Rigshospitalet of Copenhagen (K. Espersen); Amager Hospital of Copenhagen (H. Guldager); Rigshospitalet, University of Copenhagen (K-L. Welling); Finland: Aland Central Hospital of Mariehamn (D. Nyman); Kuopio University Hospital (E. Ruokonen); Seinajoki Central Hospital (K. Saarinen); France: Raymond Poincare of Garches (D. Annane); Institut Gustave Roussy of Villejuif (P. Catogni); Jacques Monod of Le Havre (G. Colas); CH Victor Jousselin of Dreux (F. Coulomb); Hôpital St Joseph & St Luc of Lyon (R. Dorne); Saint Joseph of Paris (M. Garrouste); Hôpital Pasteur of Nice (C. Isetta); CHU Brabois of Vandoeuvre Les Nancy (J. Larché); Saint Louis of Paris (J-R. LeGall); CHU de Grenoble (H. Lessire); CHU Pontchaillou of Rennes (Y. Malledant); Hôpital des Hauts Clos of Troyes (P. Mateu); CHU of Amiens (M. Ossart); Hôpital Lariboisière of Paris (D. Payen); CHD Félix Gyuon of Saint Denis La Reunion (P. Schlossmacher); Hôpital Bichat of Paris (J-F. Timsit); Hôpital Saint Andre of Bordeaux (S. Winnock); Hôpital Victor Dupouy of Argentueil (J-P. Sollet); CH Auch (L. Mallet); CHU Nancy-Brabois of Vandoeuvre (P. Maurer); CH William Morey of Chalon (J-M. Sab); Victor Dupouy of Argenteuil (J-P. Sollet); Germany: University Hospital Heidelberg (G. Aykut); Friedrich Schiller University Jena (F. Brunkhorst); University Clinic Hamburg-Eppendorf (A. Nierhaus); University Hospital Mainz (M. Lauterbach); University Hospital Carl Gustav Carus of Dresden (M. Ragaller); Hans Sushemihl Krankenhaus of Emden (R. Gatz); Vivantes-Klinikum Neukoelln of Berlin (H. Gerlach); University Hospital RWTH Aachen (D. Henzler); Kreisklinik Langen-Seligenstadt (H–B Hopf); GKH Bonn (H. Hueneburg); Zentralklinik Bad Berka (W. Karzai); Neuwerk of Moenchengladbach (A. Keller); Philipps University of Marburg (U. Kuhlmann); University Hospital Regensburg (J. Langgartner); ZKH Links der Weser of Bremen (C. Manhold); University Hospital of Dresden (M. Ragaller); Universtiy of Wuerzburg (B. Reith); Hannover Medical School (T. Schuerholz); Universitätsklinikum Charité Campus Mitte of Berlin (C. Spies); Bethanien Hospital of Moers (R. Stögbauer); KhgmbH Schongau (J. Unterburger); Greece: Thriassio Hospital of Athens (P-M. Clouva-Molyvdas); Sismanoglion General Hospital of Athens (G. Giokas); KAT General Hospital of Athens (E. Ioannidou); G. Papanikolaou General Hospital of Thessaloniki (A. Lahana); Agios Demetrios of Thessaloniki (A. Liolios); Onassis Cardiac Surgery Center of Athens (K. Marathias); University Hospital of Ioannina (G. Nakos); Tzanio Hospital of Athens (A. Tasiou); Athens Gen. Hosp. Gennimatas (H. Tsangaris); Hungary: Peterfy Hospital of Budapest (P. Tamasi); Ireland: Mater Hospital of Dublin (B. Marsh); Beaumont Hospital of Dublin (M. Power); Israel: Hadassah Hebrew University Medical Center (C. Sprung); Italy: Azienda Ospedaliera Senese o Siena (B. Biagioli); S. Martino of Genova (F. Bobbio Pallavicini); Azienda Ospedaliera S. Gerardo dei Tintori of Monza (A. Pesenti); Osp Regionale of Saronno (C. Capra); Ospedale Maggiore - University A. Avogadro of Novara (F. Della Corte); Osp. Molinette of Torino (P. P. Donadio); A.O. Umberto I Ancona, Rianimazione Clinica (A. Donati); Azienda Ospedaliera Universitaria Policlinico of Palermo (A. Giarratano); San Giovanni Di Dio of Florence (T. Giorgio); H San Raffaele IRCCS of Milano (D. Giudici); Ospedale Di Busto Arsizio (S. Greco); Civile Di Massa (A. Guadagnucci); San Paolo of Milano (G. Lapichino); S.Giovanni Bosco Torino (S. Livigni); Osp. San Giovanni of Sesto (G. Moise); S Camillo of Roma (G. Nardi); Vittorio Emanuele of Catania (E. Panascia); Hospital of Piacenza (M. Pizzamiglio); Universita di Torino-Ospedale S. Giovanni Battista (V. M. Ranieri); Policlinico Le Scotte of Siena (R. Rosi); Ospedale Maggiore Policlinico IRCCS of Milano (A. Sicignano); A. Uboldo of Cernusco Sul Naviglio (M. Solca); P·O. Civile Carrara of Massa (G. Vignali); San Giovanni of Roma (I. Volpe Rinonapoli); Netherlands: Boven IJ Ziekenhuis of Amsterdam (M. Barnas); UMC St Radboud of Nijmegen (E.E. De Bel); Academic Medical Center of Amsterdam (A-C. De Pont); VUMC of Amsterdam (J. Groeneveld); Groningen University Hospital (M Nijsten); Waterlandziekenhuis of Purmerend (L Sie); OLVG of Amsterdam (D. F. Zandstra); Norway: Sentralsjukehuset i Rogaland of Stavanger (S. Harboe); Sykehuset Østfold of Fredrikstad (S. Lindén); Aker University Hospital of Oslo (R. Z. Lovstad); Ulleval University Hospitalof Oslo (H. Moen); Akershus University Hospital of Nordbyhagen (N. Smith-Erichsen); Poland: Paediatric University Hospital of Lodz (A. Piotrowski); Central Clinic Hospital SLAM of Katowice (E. Karpel); Portugal : Garcia de Orta of Almada (E. Almeida); Hospital de St. António dos Capuchos of Lisboa (R. Moreno); Hospital de Santa Maria of Lisboa (A. Pais-De-Lacerda); Hospital S.Joao of Porto (J. A. Paiva); Fernado Fonseca of Masama (I. Serra); São Teotonio Viseu (A. Pimentel); Romania: Inst of Cardiovascular Diseases of Bucharest (D. Filipescu); Serbia and Montenegro: Military Medical Academy of Belgrade (K. Jovanovic); Slovakia: SUSCH of Bratislava (P. Malik); Slovenia: General Hospital of Novo Mesto (K. Lucka); General Hospital of Celje (G. Voga); Spain: Hospital Universitario Rio Hortega of Valladolid (C. Aldecoa Alvarez-Santullano); Sabadell Hospital (A. Artigas); Hospital Clinic of Barcelona (E. Zavala, A. Escorsell, J. Nicolas); Virgen del Camino of Pamplona (J. J. Izura Cea); Virgen de la Salud of Toledo (L. Marina); 12 de Octubre of Madrid (J. Montejo); Gregorio Maranon of Madrid (E. Palencia); General Universitario de Elche (F. Santos); Puerta del Mar of Cadiz (R. Sierra-Camerino); Fundación Jiménez Díaz of Madrid (F. Sipmann); Hospital Clinic of Barcelona (E. Zavala); Sweden: Central Hospital of Kristianstad (K. Brodersen); Stockholm Soder Hospital (J. Haggqvist); Sunderby Hospital of Luleå (D. Hermansson); Huddinge University Hospital of Stockholm (H. Hjelmqvist); Switzerland: Kantonsspital Luzern (K. Heer); Hirslanden Klinik Beau-Site of Bern (G. Loderer); University Hospital of Zurich (M. Maggiorini); Hôpital de la ville of La Chaux-de-Fonds (H. Zender); United Kingdom: Edinburgh Western General Hospital (P. Andrews); Peterborough Hospitals NHS Trust of Peterborough (B. Appadu); University Hospital Lewisham, London (C. Barrera Groba); Bristol Royal Infirmary (J. Bewley); Queen Elizabeth Hospital Kings Lynn (K. Burchett); Milton Keynes General (P. Chambers); Homerton University Hospital of London (J. Coakley); Charing Cross Hospital of London (D. Doberenz); North Staffordshire Hospital of Stoke On Trent (N. Eastwood); Antrim Area Hospital (A. Ferguson); Royal Berkshire Hospital of Reading (J. Fielden); The James Cook University Hospital of Middlesbrough (J. Gedney); Addenbrookes of Cambridge (K. Gunning); Rotherham DGH (D. Harling); St.Helier of Carshalton (S. Jankowski); Southport & Formby (D. Jayson); Freeman of Newcastle Upon Tyne (A. Kilner); University Hospital of North Tees at Stockton on Tees (V. Krishna-Kumar); St. Thomas Hospital of London (K. Lei); Royal Infirmary of Edinburgh (S. Mackenzie); Derriford of Plymouth (P. Macnaughton); Royal Liverpool University Hospital (G. Marx); Stirling Royal Infirmary (C. McCulloch); University Hospital of Wales, Cardiff (P. Morgan); St George’s Hospital of London (A. Rhodes); Gloucestershire Royal Hospital (C. Roberts); St Peters of Chertsey (M. Russell); James Paget Hospital of Great Yarmouth (D. Tupper-Carey, M. Wright); Kettering General Hospital (L. Twohey); Burnley DGH (J. Watts); Northampton General Hospital (R. Webster); Dumfries Royal Infirmary (D. Williams).
Rights and permissions
About this article
Cite this article
Sakr, Y., Madl, C., Filipescu, D. et al. Obesity is associated with increased morbidity but not mortality in critically ill patients. Intensive Care Med 34, 1999–2009 (2008). https://doi.org/10.1007/s00134-008-1243-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-008-1243-0