Abstract
Objective
To investigate the effects of using propofol for medium and long-term sedation on mortality and length of intensive care unit (ICU) stay of critically ill adult patients.
Design
Randomised controlled studies comparing propofol with an alternative sedative agent in critically ill adult patients were included without language restriction from the Cochrane Controlled Trial Register (2007 issue 3), EMBASE, and MEDLINE databases (1966 to 1 December 2007). Two reviewers reviewed the quality of the studies and performed data extraction independently.
Measurements and results
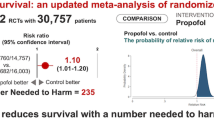
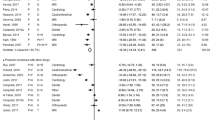
Sixteen randomised controlled studies with a total of 1,386 critically ill adult patients were considered. Nine of the pooled studies (56%) limited the doses of propofol infusion to <6 mg/kg h−1. Mortality was not significantly different between patients sedated with propofol, or an alternative sedative agent (odds ratio [OR] 1.05, 95% confidence interval [CI] 0.80–1.38, P = 0.74; I 2 = 0%). Using propofol for medium and long-term sedation was associated with a significant reduction in length of ICU stay (overall weighted-mean-difference [WMD] in days −0.99, 95%CI −1.51 to −0.47, P = 0.0002; I 2 = 82.26%) when compared to an alternative sedative agent; however, this benefit became insignificant (overall WMD in days −0.98, 95%CI −2.86 to 0.89, P = 0.30; I 2 = 78.8%) when the comparison was limited to between propofol and midazolam.
Conclusions
Using propofol for prolonged sedation in critically ill patients appears to be safe and may reduce duration of mechanical ventilation. It reduces the length of ICU stay when compared to long acting benzodiazepines, but not when compared to midazolam.




Similar content being viewed by others
References
Ostermann ME, Keenan SP, Seiferling RA, Sibbald WJ (2000) Sedation in the intensive care unit: a systematic review. JAMA 283:1451–1459
Walder B, Elia N, Henzi I, Romand JR, Tramèr MR (2001) A lack of evidence of superiority of propofol versus midazolam for sedation in mechanically ventilated critically ill patients: a qualitative and quantitative systematic review. Anesth Analg 92:975–983
Tsuchiya M, Asada A, Maeda K, Ueda Y, Sato EF, Shindo M, Inoue M (2001) Propofol versus midazolam regarding their antioxidant activities. Am J Respir Crit Care Med 163:26–31
Marik PE (2005) Propofol: an immunomodulating agent. Pharmacotherapy 25(5 Pt 2):28S–33S
Ozaki M (2002) The effects of propofol and midazolam on canine left ventricular contractility. Masui 51:611–619
Mistraletti G, Donatelli F, Carli F (2005) Metabolic and endocrine effects of sedative agents. Curr Opin Crit Care 11:312–317
Nanas S, Angelopoulos E, Tsikriki S, Kritikos K, Voutsinas E, Zervakis D, Kanaloupiti D, Pratikaki M, Roussos C (2007) Propofol-induced hyperamylasaemia in a general intensive care unit. Anaesth Intensive Care 35:920–923
Vasile B, Rasulo F, Candiani A, Latronico N (2003) The pathophysiology of propofol infusion syndrome: a simple name for a complex syndrome. Intensive Care Med 29:1417–1425
Fraser GL, Riker RR (2007) Sedation and analgesia in the critically ill adult. Curr Opin Anaesthesiol 20:119–123
Ghori KA, Harmon DC, Elashaal A, Butler M, Walsh F, O’Sullivan MG, Shorten GD (2007) Effect of midazolam versus propofol sedation on markers of neurological injury and outcome after isolated severe head injury: a pilot study. Crit Care Resusc 9:166–171
Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327:557–560
Kress JP, O’Connor MF, Pohlman AS, Olson D, Lavoie A, Toledano A, Hall JB (1996) Sedation of critically ill patients during mechanical ventilation. A comparison of propofol and midazolam. Am J Respir Crit Care Med 153:1012–1018
Harris CE, Grounds RM, Murray AM, Lumley J, Royston D, Morgan M (1990) Propofol for long-term sedation in the intensive care unit. A comparison with papaveretum and midazolam. Anaesthesia 45:366–372
Carson SS, Kress JP, Rodgers JE, Vinayak A, Campbell-Bright S, Levitt J, Bourdet S, Ivanova A, Henderson AG, Pohlman A, Chang L, Rich PB, Hall J (2006) A randomized trial of intermittent lorazepam versus propofol with daily interruption in mechanically ventilated patients. Crit Care Med 34:1326–1332
Sandiumenge Camps A, Sanchez-Izquierdo Riera JA, Toral Vazquez D, Sa Borges M, Peinado Rodriguez J, Alted Lopez E (2000) Midazolam and 2% propofol in long-term sedation of traumatized critically ill patients: efficacy and safety comparison. Crit Care Med 28:3612–3619
Barrientos-Vega R, Mar Sánchez-Soria M, Morales-García C, Robas-Gómez A, Cuena-Boy R, Ayensa-Rincon A (1997) Prolonged sedation of critically ill patients with midazolam or propofol: impact on weaning and costs. Crit Care Med 25:33–40
Chamorro C, de Latorre FJ, Montero A, Sánchez-Izquierdo JA, Jareño A, Moreno JA, Gonzalez E, Barrios M, Carpintero JL, Martín-Santos F, Otero B, Ginestal R (1996) Comparative study of propofol versus midazolam in the sedation of critically ill patients: results of a prospective, randomized, multicenter trial. Crit Care Med 24:932–939
Hall RI, Sandham D, Cardinal P, Tweeddale M, Moher D, Wang X, Anis AH; Study Investigators (2001) Propofol vs midazolam for ICU sedation: a Canadian multicenter randomized trial. Chest 119:1151–1159
Weinbroum AA, Halpern P, Rudick V, Sorkine P, Freedman M, Geller E (1997) Midazolam versus propofol for long-term sedation in the ICU: a randomized prospective comparison. Intensive Care Med 23:1258–1263
Higgins TL, Murray M, Kett DH, Fulda G, Kramer KM, Gelmont D, Dedhia HV, Levy H, Teres D, Zaloga GP, Ko H, Thompson KA (2000) Trace element homeostasis during continuous sedation with propofol containing EDTA versus other sedatives in critically ill patients. Intensive Care Med 26:S413–S421
Kelly DF, Goodale DB, Williams J, Herr DL, Chappell ET, Rosner MJ, Jacobson J, Levy ML, Croce MA, Maniker AH, Fulda GJ, Lovett JV, Mohan O, Narayan RK (1999) Propofol in the treatment of moderate and severe head injury: a randomized, prospective double-blinded pilot trial. J Neurosurg 90:1042–1052
Costa J, Cabré L, Molina R, Carrasco G (1994) Cost of ICU sedation: comparison of empirical and controlled sedation methods. Clin Intensive Care 5(5 Suppl):17–21
Manley NM, Fitzpatrick RW, Long T, Jones PW (1997) A cost analysis of alfentanil + propofol vs morphine + midazolam for the sedation of critically ill patients. Pharmacoeconomics 12(2 Pt 2):247–255
Degauque C, Dupuis A (1991) A study to compare the use of propofol and midazolam for the sedation of patients with acute respiratory failure. J Drug Dev 4(Suppl 3):95–97
Kress JP, Pohlman AS, Hall JB (2001) Effects of sedative interruption in critically Ill, mechanically ventilated patients receiving midazolam or propofol. J Clin Outcomes Manage 8:33–39
Sanchez-Izquierdo-Riera JA, Caballero-Cubedo RE, Perez-Vela JL, Ambros-Checa A, Cantalapiedra-Santiago JA, Alted-Lopez E (1998) Propofol versus midazolam: safety and efficacy for sedating the severe trauma patient. Anesth Analg 86:1219–1224
Fragen RJ (1997) Pharmacokinetics and pharmacodynamics of midazolam given via continuous intravenous infusion in intensive care units. Clin Ther 19:405–419
Mandema JW, Tuk B, van Steveninck AL, Breimer DD, Cohen AF, Danhof M (1992) Pharmacokinetic-pharmacodynamic modeling of the central nervous system effects of midazolam and its main metabolite alpha-hydroxymidazolam in healthy volunteers. Clin Pharmacol Ther 51:715–728
Pandharipande PP, Pun BT, Herr DL, Maze M, Girard TD, Miller RR, Shintani AK, Thompson JL, Jackson JC, Deppen SA, Stiles RA, Dittus RS, Bernard GR, Ely EW (2007) Effect of sedation with dexmedetomidine vs lorazepam on acute brain dysfunction in mechanically ventilated patients: the MENDS randomized controlled trial. JAMA 298:2644–2653
Kress JP, Pohlman AS, O’Connor MF, Hall JB (2000) Daily interruption of sedative infusions in critically ill patients undergoing mechanical ventilation. N Engl J Med 342:1471–1477
Perouansky M (2007) Liaisons dangereuses? General anaesthetics and long-term toxicity in the CNS. Eur J Anaesthesiol 24:107–115
Girard TD, Kress JP, Fuchs BD, Thomason JW, Schweickert WD, Pun BT, Taichman DB, Dunn JG, Pohlman AS, Kinniry PA, Jackson JC, Canonico AE, Light RW, Shintani AK, Thompson JL, Gordon SM, Hall JB, Dittus RS, Bernard GR, Ely EW (2008) Efficacy and safety of a paired sedation and ventilator weaning protocol for mechanically ventilated patients in intensive care (awakening and breathing controlled trial): a randomised controlled trial. Lancet 371:126–134
Acknowledgments
We would like to thank Dr. Kamran Ghori for his assistance in providing unpublished data from his study. All authors have no financial conflict of interests to declare.
Conflict of interest statement
No financial support was received from any commercial company or organisation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ho, K.M., Ng, J.Y. The use of propofol for medium and long-term sedation in critically ill adult patients: a meta-analysis. Intensive Care Med 34, 1969–1979 (2008). https://doi.org/10.1007/s00134-008-1186-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-008-1186-5