Abstract
Objective
Bacterial respiratory tract colonization predisposes critically ill patients to intensive care unit (ICU)-acquired infections. It is unclear to what extent systemic antibiotics affect colonization persistence. Persistence of respiratory tract colonization, and the effects of systemic antibiotics hereon, were determined in a cohort of ICU patients.
Design
Clinical and microbiological data were collected from 715 admitted mechanically ventilated ICU patients with bacterial growth documented in respiratory tract samples. First day of colonization, persistence of colonization and antibiotic effects hereon were analyzed for six groups of pathogens: Pseudomonas aeruginosa, Acinetobacter species, Enterobacteriaceae, Staphylococcus aureus, Streptococcus pneumoniae and Haemophilus influenzae. Systemic antibiotics were grouped into ‘effective’ and ‘ineffective’ antibiotics, based on in-vitro susceptibility data for the relevant bacteria. The effects of antibiotics were quantified as relative risk (RR) of bacterial persistence in the absence of effective antibiotics.
Measurements and results
Persistence of colonization differed significantly between pathogens, ranging from 4 days (median) for H. influenzae and Strep. pneumoniae to 8 days for P. aeruginosa. Systemic antibiotics were administered on 7,102 (61%) of patient days. Antibiotic use was associated with non-persistence for all pathogens, except Acinetobacter species and P. aeruginosa. RR for non-persistence (as compared to ineffective or no antibiotics) ranged from 3.1 (95% CI 1.4–6.6) for H. influenzae to 0.5 (0.3–1.0) for Acinetobacter species.
Conclusions
In mechanically ventilated patients, persistence dynamics of bacterial respiratory tract colonization, and the effects of (in-vitro) effective antibiotics hereon, are pathogen-specific.
Similar content being viewed by others
Introduction
Respiratory tract colonization with nosocomial bacteria predisposes critically ill patients to life-threatening infections, such as ventilator-associated pneumonia (VAP) [1]. Approximately one quarter of intensive care unit (ICU) patients develop VAP, which makes it the most frequently occurring ICU-acquired infection, responsible for the majority of antibiotic prescriptions in the ICU [2]. In patients admitted to the ICU directly from the community, the upper respiratory tract flora changes from so-called early-onset bacteria (such as Streptococcus pneumoniae, Haemophilus influenzae and Staphylococcus aureus) to typical late-onset (or nosocomial) pathogens (such as enteric Gram-negative bacteria, Pseudomonas aeruginosa and Acinetobacter species). The mechanisms underlying this ecological change remain largely unknown, though a role of antibiotics herein seems plausible. Only a proportion of the colonized patients will develop VAP, usually after a gradual change from asymptomatic colonization to clinical infection.
Bacterial colonization of the respiratory tract frequently persists, even when a patient receives antimicrobial treatment, and even though the colonizing bacteria are, in vitro, susceptible to the antibiotics. The capacity of bacteria to continue to grow in the presence of antibiotics was demonstrated long ago [3], in vitro, and such bacteria were called ‘persister’ cells. Such persister cells appear to be specialized survivors [4, 5].
A cohort of mechanically ventilated ICU patients was used to investigate the phenomenon of persistent respiratory tract colonization and the effects of systemic antibiotics hereon, by analyzing endotracheal aspirate cultures performed during ICU stay. We hypothesized that antibiotics with presumed efficacy, based on in-vitro susceptibility testing, reduce the likelihood of persistence of respiratory tract colonization, compared to antibiotics presumed to be ineffective or when no antibiotics were administered at all. Of note, we did not investigate the effects of topical antibiotics. Previously, we described the construction and evaluation of a computerized decision-support system for diagnosing VAP [6]. This computer system, based on Bayesian statistics, computes the likelihood that a mechanically ventilated ICU patient suffers from VAP. The next step in model development is to have the model predict the most likely pathogen causing VAP. The analyses described in the current manuscript were needed as input for optimizing the predictive performance of the computer system.
Materials and methods
Patients
All patients admitted to two adult ICUs (a ten-bed medical ICU and an eight-bed neurosurgical ICU) of the University Medical Center Utrecht (UMCU) between 1 January 2000 and 1 January 2003 were included in this observational cohort study. Patients with cystic fibrosis were excluded, as they frequently are chronically colonized by P. aeruginosa [7]. The UMCU is a 1,062-bed tertiary care hospital. In both ICUs all relevant clinical, laboratory and microbiological variables are registered on a daily basis in computerized patient data management systems. The institutional review board waived the necessity of informed consent for this observational study.
Definitions
Respiratory tract colonization (hereafter often referred to as ‘colonization’) status is based on microbiological culture results of endotracheal aspirates, which were obtained as part of daily patient care, without specific surveillance protocol. Samples were analyzed semi-quantitatively (three-quadrant streak method), and culture positivity was defined as any growth [8]. Absence of a pathogen was considered ‘negative’. Distinction was made between patients who were ‘colonized on admission’ and patients who ‘acquired colonization during ICU stay’.
Colonization was analyzed for the following bacterial species: P. aeruginosa, Acinetobacter spp., Enterobacteriaceae, Staph. aureus, H. influenzae and Strep. pneumoniae. The group of Enterobacteriaceae contains multiple species, including Escherichia coli, Klebsiella pneumoniae, Klebsiella spp. , Proteus mirabilis, Citrobacter spp., Enterobacter cloacae, Enterobacter spp., Morganella spp. and Serratia spp.
Bacterial colonization and persistence
Colonization on admission was defined as a positive culture obtained ≤ 48 h after ICU admission. Acquired endotracheal colonization with a certain pathogen was defined as colonization demonstrated > 48 h after ICU admission and preceded by a negative culture for that specific pathogen. The first day on which a specific pathogen was detected was considered ‘the first day of colonization’. When no culture results were obtained within 48 h after ICU admission, the microbiological status of a patient on admission was considered “unknown”. As a patient can get colonized by multiple pathogens during ICU stay, it is possible to place a patient in more than one category of colonization (for example: a patient is colonized with Staph. aureus on admission and acquires P. aeruginosa during ICU stay). For each group of microorganisms prevalence of colonization on admission was determined, as well as the incidence and first day of acquired colonization.
Persistent colonization was defined as a period, starting at the first day of colonization, in which at least two successive culture results were positive for the same bacterial species. After a positive culture, a single negative culture followed by positive cultures with same bacterial species was also considered persistent colonization. The period between the last positive culture and ICU discharge, during which no other culture was obtained, again was considered persistent colonization. ‘Non-persistent colonization’ was defined as conversion of a positive colonization status to a negative status (for that pathogen) after a period of persistent colonization. The interval between two successive cultures was considered a sub-period of colonization. Thus, multiple sub-periods of colonization per patient could occur. Two successive negative sputum cultures followed by a single positive culture, again followed by a negative culture, was considered ‘non-persistent colonization’. Duration of bacterial persistence was analyzed for all episodes of bacterial colonization.
Antibiotics
For each pathogen, susceptibility to antibiotics was based on in-vitro susceptibility data as determined in our hospital's medical microbiology laboratory. Breakpoints for susceptibility were based on CLSI recommendations (Clinical and Laboratory Standards Institute, Performance Standards for Antimicrobial Susceptibility Testing: 16th Informational Supplement). “No antibiotics” was considered ineffective treatment. The effects of antibiotics on bacterial persistence were analyzed for all episodes of colonization by determining antibiotic exposure during 4-day periods before the moment of culture taking. Exposure was defined as administration of presumed effective antibiotics (based on susceptibility data) during 2 or more days in this 4-day period.
Naturally, only patients with at least two cultures obtained during ICU admission were eligible for this analysis. In case of multiple colonization periods of an individual patient with the same bacteria, only the first episode of bacterial colonization was analyzed. Furthermore, repetitive periods of colonization in an individual patient with similar antibiotic exposure were excluded.
The likelihood of bacterial persistence was determined for situations with and without exposure to effective antibiotics. Absence of antibiotics was grouped with exposure to ineffective antibiotics. In a subsequent case–control analysis, each patient that acquired bacterial colonization with a certain pathogen was matched to three patients that had not acquired colonization with that particular pathogen during ICU stay. The day of matching was the first day of colonization for the “case” patient and a day representing similar length of stay in ICU for the “control” patient (see Fig. 1 for an example). Antibiotic exposure in the days before matching was defined as described above. Antibiotic exposure between patients with acquired colonization and their controls was evaluated.
Case–control analysis, denoted by two timelines: case and control patient. Each box represents one ICU day. SA: Staph. aureus found in endotracheal aspirate; + represents a (assumed) colonized ICU day preceded by a positive culture; – represents a negative culture and, thus, the end of a colonized period. The colonized period as a whole is denoted by gray shading. Antibiotic administration for 4 days preceding the first positive culture is denoted by hatching. Here, day of matching is day 5
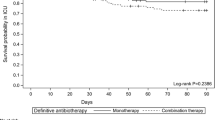
Statistical analysis
SPSS version 14.0 [9] was used for statistical analysis and Gnuplot version 4.0 [10] for creating graphs. Student's t-test and Mann–Whitney-U tests were used when appropriate, and a probability level less than 0.05 was considered statistically significant. A Kaplan–Meier survival analysis was performed to assess the duration of persistence over time. Colonized patients were eligible for the analysis and patients colonized when discharged were censored, i. e., ‘withdrawn alive’.
Results
Patients
The total study cohort consisted of 1,410 admissions (17,709 ICU days), with 3,289 cultures of endotracheal aspirates performed in 1,012 admissions (3.25 cultures per admission), and bacterial growth from at least one endotracheal aspirate was documented for 715 admissions (71%; 2,111 cultures). The characteristics of this patient population have been described previously [6]. For the 715 patients included in this study, the median duration of ICU stay was 11 days (IQR 5–21 days). The median ICU stay of patients without documented bacterial growth from endotracheal aspirates was 6 days (IQR 3–10 days) (p < 0.05). For clarity, patients without cultures taken were not included in this study. To determine whether a longer stay in ICU was associated with a lower or higher number of samples taken, the first 50 days of ICU stay were categorized in consecutive 5-day groups. The average proportion of days on which cultures were taken was 20% and varied from 17% on days 41–45 to 22% on days 26–30. Therefore, longer length of stay did not increase the likelihood of sampling.
Episodes of colonization
Colonization with Enterobacteriaceae occurred most frequently and was demonstrated in 413 patients, followed by Staph. aureus (258 patients, of whom 140 (54%) were admitted to the medical ICU and 118 (46%) to the neurosurgical ICU), P. aeruginosa (180 patients), Strep. pneumoniae (153 patients), H. influenzae (142 patients) and Acinetobacter spp. (73 patients) (Table 1).
Colonization on admission could not be evaluated for 295 patients, because of absence of cultures obtained within 48 h after admission. Colonization on admission was analyzed in 311 patients and was most frequently observed for Enterobacteriaceae, that is, in 33%, whereas colonization on admission with Acinetobacter spp. was documented in 4% of these cases. Overall, the median first day of acquired colonization was day seven (IQR 4–14 days) after ICU admission, which differed considerably between pathogens. Acquired colonization with H. influenzae and Strep. pneumoniae was documented after a median of four and five days in ICU, respectively, whereas the median first day of colonization with Acinetobacter spp. and P. aeruginosa was eleven days. The Enterobacteriaceae group and Staph. aureus fell in-between the early-onset and late-onset colonizers (Table 1).
Once established, duration of colonization also differed considerably between pathogens. Bacterial persistence occurred in 85% of patients colonized with P. aeruginosa, which was a significantly higher proportion than for all other bacteria or bacteria groups (Table 1). The lowest proportions of patients with bacterial persistence were found for H. influenzae and Strep. pneumoniae. The median duration of bacterial persistence for patients colonized with P. aeruginosa was 8 days (IQR 4–16 days), which was significantly longer than persistence of any of the other pathogens (Table 1, Fig. 2).
Antibiotics and antibiotic susceptibility
In the 715 patients included in this analysis, antibiotics were administered on 7,102 (61%) of 11,689 patient days. Amoxicillin + clavulanic acid (58% of patients), gentamicin (36%), ceftriaxone (31%) and ciprofloxacin (28%) were prescribed most frequently (Table 2). When expressed in proportions of all patient days, the same four antibiotics were prescribed most frequently. Median duration of antibiotic therapy ranged from 2 to 5 days. Of note, many patients were discharged from ICU with antibiotic therapy continued on regular wards.
Non-susceptibility levels to antibiotics of the first isolates per patient were fairly low (Table 3). For instance, all Strep. pneumoniae were susceptible to penicillin, all Staph. aureus to flucloxacillin and all Gram-negative bacteria to imipenem. Resistance developed only sporadically during colonization (data not shown).
Effects of antibiotics on colonization persistence
Systemic antibiotic treatment (with antibiotics for which pathogens were in-vitro susceptible) was associated with reduced persistence of all pathogens except for P. aeruginosa and Acinetobacter spp. (Table 4). The highest relative risk (RR) of non-persistence during effective antibiotic treatment was 3.1 (95% CI 1.4–6.6) for H. influenzae. In this analysis, the effect of effective antibiotics was compared to ineffective antibiotics, being mainly ‘no antibiotics’ for H. influenzae. Significant associations between effective antibiotics and non-persistence of colonization were also observed for Strep. pneumoniae (2.1, 95% CI 1.2–3.6), Staph. aureus (1.6, 95% CI 1.3–2.0), and Enterobacteriaceae (1.5, 95% CI 1.3–1.7).
In the case–control analysis, patients that had acquired colonization with either H. influenzae, Strep. pneumoniae, Staph. aureus or Enterobacteriaceae had had less exposure to effective antibiotics in the days before acquisition was demonstrated (Table 5). No such association could be demonstrated for P. aeruginosa and Acinetobacter spp.
Discussion
The major findings of this observational study are that endotracheal colonization dynamics and the effects of systemic antibiotics hereon differ among bacterial species. This implies that evaluation of bacterial persistence as a marker of ongoing infection or as an endpoint of prevention studies should be pathogen-specific. Early-onset pathogens (such as H. influenzae, Strep. pneumoniae and Staph. aureus) appear to be much more sensitive to intravenously administered antibiotics (with documented in-vitro susceptibility) than typical late-onset pathogens (such as P. aeruginosa and Acinetobacter spp.).
Strengths of our study include the large size of the patient cohort with detailed data on colonization, antibiotic susceptibility of pathogens and antibiotic administration. The latter allowed us to specifically analyze the effects of antibiotics for which the pathogen was susceptible, based on in-vitro susceptibility testing. Limitations, though, include the pragmatic nature of microbiological data collection, as we had to rely on samples obtained for clinical reasons and not on a prospectively implemented surveillance schedule. Nevertheless, on average three cultures were obtained for each of the 715 patients included in this analysis.
Our data confirm previously reported findings on the different time-frames of bacterial colonization in mechanically ventilated patients [11, 12]. Colonization on admission was more frequently observed for early-onset pathogens, and acquired colonization most frequently occurred with typical late-onset pathogens. Our findings strongly suggest that there are differences in the effects of intravenous antibiotics on different bacterial species. This implies that prophylactic use of systemic antibiotics will mainly affect endotracheal colonization with early-onset pathogens. The risk of acquiring colonization with Staph. aureus, Strep. pneumoniae and H. influenzae was reduced by approximately 50% when effective antibiotics were administered. Accordingly, patients with low risk of respiratory tract colonization with Gram-negative bacteria on ICU admission, such as those who have little co-morbidity and are directly admitted to the ICU without long-term hospitalization (e. g., patients with trauma, needing complex surgery, or with acute neurological diseases) could potentially benefit from prophylactic antibiotic use. To the best of our knowledge this concept has been empirically evaluated only once. Sirvent and co-workers randomized 100 mechanically ventilated patients with structural coma to a short course of prophylaxis with cefuroxime (two dosages of 1,500 mg 12 h apart after intubation) or no prophylaxis [13]. If colonized during intubation, most patients were colonized with early-onset pathogens. Cefuroxime prophylaxis was associated with a reduction in the development of microbiologically confirmed VAP from 48% in control patients to 23% in the study group. Sixty-four percent of the VAP episodes were caused by methicillin-sensitive Staph. aureus, H. influenzae and Strep. pneumoniae. In another study previous (short-term) antibiotic treatment in mechanically ventilated patients with head injury appeared protective against initial tracheobronchial colonization with early-onset pathogens, but increased the risk for subsequent lower airway colonization with late-onset pathogens [14]. The other consequence of our findings is that the approach of systemic antibiotic prophylaxis is less likely to be effective for late-onset pathogens, even with antibiotics for which these pathogens are, in vitro, susceptible.
The reason for the observed difference between early-onset and late-onset pathogens, though, remains to be determined. Pathogen-specific characteristics, such as the ability of biofilm formation of P. aeruginosa, or patient-specific characteristics, such as the severity of underlying disease or immune paralysis, could both be involved, but further—more detailed—studies are needed to elucidate this matter.
References
Bonten MJM, Bergmans CJJ (1996) Risk factors for pneumonia, and colonization of respiratory tract and stomach in mechanically ventilated ICU patients. Am J Respir Crit Care Med 154:1339–1346
Bergmans CJJ, Bonten MJM (1997) Indications for antibiotic use in ICU patients: a one-year prospective surveillance. J Antimicrob Chemother 39:527–535
Bigger JW (1944) Treatment of staphylococcal infections with penicillin. Lancet 2:497–500
Kussel E, Kishony R, Balaban NQ, Leibler S (2005) Bacterial persistence: a model of survival in changing environments. Genetics 169:1807–1814
Keren I, Kaldalu N, Spoering A, Wang Y, Lewis K (2004) Persister cells and tolerance to antimicrobials. FEMS Microbiol Lett 230:13–18
Schurink CAM, Visscher S, Lucas PJF, Leeuwen HJ van, Buskens E, Hoff RG, Hoepelman IM, Bonten MJM (2007) A Bayesian decision-support system for diagnosing ventilator-associated pneumonia. Intensive Care Med 33:1379–1386
Murray TS, Egan M, Kazmierczak BI (2007) Pseudomonas aeruginosa chronic colonization in cystic fibrosis patients. Curr Opin Pediatr 19:83–88
Bergmans DC, Bonten MJ, De Leeuw PW, Stobberingh EE (1997) Reproducibility of quantitative cultures of endotracheal aspirates from mechanically ventilated patients. J Clin Microbiol 35:796–798
SPSS Inc., Chicago USA. http://www.spss.com
Gnuplot, interactive data and function plotting utility. http://www.gnuplot.info
Trouillet JL, Chastre J, Vuagnat A, Joly-Guillou ML, Combaux D, Dombret MC, Gibert C (1998) Ventilator-associated pneumonia caused by potentially drug-resistant bacteria. Am J Respir Crit Care Med 157:531–539
Verhamme KM, De Coster W, De Roo L, De Beenhouwer H, Nollet G, Verbeke J, Demeyer I, Jordens P (2007) Pathogens in early-onset and late-onset intensive care unit-acquired pneumonia. Infect Control Hosp Epidemiol 28:389–397
Sirvent JM, Torres A, El-Ebiary M, Castro P, de Batlle J, Bonet A (1997) Protective effect of intravenously administered cefuroxime against nosocomial pneumonia in patients with structural coma. Am J Respir Crit Care Med 155:1729–1734
Ewig S, Torres A, El-Ebiary M, Fàbregas N, Hernández C, González J, Nicolás JM, Soto L (1999) Bacterial colonization patterns in mechanically ventilated patients with traumatic and medical head injury. Am J Respir Crit Care Med 159:188–198
Acknowledgements
This study was supported by a grant from ZonMw (project number 2100.0035), and NWO (project number 634.000.026) for the TimeBayes project. Furthermore, the authors thank Dr. M.A. Leverstein-van Hall, Dr. M.R. Visser and Prof. R.A. Weinstein for useful comments.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Visscher, S., Schurink, C.A.M., Melsen, W.G. et al. Effects of systemic antibiotic therapy on bacterial persistence in the respiratory tract of mechanically ventilated patients. Intensive Care Med 34, 692–699 (2008). https://doi.org/10.1007/s00134-007-0984-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-007-0984-5