Abstract
Objective
To assess the anti-inflammatory effects of recombinant human activated protein C (rhAPC) in a porcine model of acute endotoxemia.
Design and setting
Animal randomized controlled study at the Laboratory of Clinical Institute, Aarhus University Hospital.
Subjects
Eighteen female landrace pigs (30 kg).
Interventions
By pairwise randomization, pigs were given either LPS or LPS and rhAPC. Both groups received a stepwise increasing LPS infusion for 30 min; whereafter the infusion continued at a lower rate (300 min LPS in both groups). The LPS+rhAPC group received rhAPC (100 μg/kg per hour) 15 min before the LPS infusion began and throughout the trial period.
Results
While rhAPC showed no modifying effects on peak plasma levels of pro- or anti-inflammatory cytokines (TNF-α, IL-6, IL-8, IL-10), TNF-α and IL-10 peaked significantly later in the rhAPC-treated animals. The profibrinolytic effects of rhAPC were confirmed by decreased plasminogen activator inhibitor 1 levels, while no differences were found in other coagulation markers, hemodynamic, metabolic, or leukocyte data between the two groups.
Conclusions
We found no significant effect of rhAPC on plasma levels of either pro- or anti-inflammatory cytokines in this porcine model of acute endotoxemia. However, TNF-α and IL-10 peaked significantly later in the rhAPC-treated animals.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sepsis in one of the leading causes of death in the ICU [1, 2]. The deleterious effects of sepsis are due partly to a microbiological-host interaction causing a generalized activation of the immune system, endothelium, and coagulation system. Except for very important measures with source control and adequate antibiotics, treatment of patients with severe sepsis and septic shock is symptomatic and supportive. Protein C has earlier been demonstrated to prevent the lethal effects of Escherichia coli in baboons [3] and to reduce mortality and morbidity in small noncontrolled studies of patients with meningococcal sepsis [4–7]. In 2001 it was shown that treatment with recombinant human activated protein C (rhAPC) has a beneficial effect on mortality and organ dysfunction in critically ill patients with severe sepsis and septic shock [8]. However, the role of rhAPC in the treatment of sepsis is still uncertain [9, 10]. APC has in vitro shown antithrombotic, profibrinolytic, antiapoptotic, and anti-inflammatory properties. Since treatments with other anticoagulants such as antithrombin III and tissue-factor-pathway inhibitor did not have survival benefits in other randomized controlled studies, the positive effect of rhAPC has been attributed to its proposed anti-inflammatory effects [8, 11–13]. Therefore we hypothesized that treatment with rhAPC would attenuate the proinflammatory cytokine response during lipopolysaccharide (LPS) challenge [14].
The aim of this porcine study on acute endotoxemia was therefore to investigate whether intervention with rhAPC would induce significant changes in plasma levels of tumor necrosis factor alfa (TNF-α) and interleukins (IL) −6, −8, and −10. To ensure comparability between the two groups we controlled hemodynamics, ventilation, and blood glucose.
Materials and methods
The National Committee on Animal Research Ethics approved the setup (Copenhagen, Denmark, 27 May, 2002, 561–538), and the work was carried out according to the guidelines in the Guide for the Care and Use of Laboratory Animals. Eighteen female landrace pigs (weight 30 kg) were fasted overnight but had free access to water. They were premedicated intramuscularly with ketamine (10 mg/kg) and midazolam (0.25 mg/kg). Anesthesia was induced intravenously with ketamine (5 mg/kg) and maintained with a continuous intravenous infusion of fentanyl (60 μg/kg per hour) and midazolam (6 mg/kg per hour). The pigs were intubated endotracheally, and the lungs were volume-controlled ventilated by a Servo 900D ventilator (Siemens Elema, Solna, Sweden) with tidal volume of 8 ml/kg, ventilatory rate of 18 bpm, and positive end-expiratory pressure of 5 cmH2O. Inspired oxygen fraction (FIO2) and the ventilatory rate were continuously adjusted throughout the trial to keep PaO2 above 13 kPa and PaCO2 between 4.5 and 6.0 kPa. A pulmonary artery catheter (Edwards Lifescience, Irvine, Calif., USA) was inserted via the external jugular vein for pulmonary artery pressure measurements. Another catheter (5 F, St. Jude Medical, St. Paul, Minn., USA) was inserted into the left carotid artery for continuous monitoring of blood pressure (mean arterial blood pressure, MAP), heart rate (HR), and for blood sampling. A bladder catheter was inserted for urine collection. After induction of anesthesia, endotracheal intubation, and instrumentation the animals were left without any intervention for 45 min.
Respiratory monitoring
Expired minute volume, tidal volume, respiratory rate, peak and mean inspiratory pressures, and FIO2 were obtained continuously from the ventilator monitor throughout the study. Blood samples were collected from the arterial line every 30 min and more frequently during the increasing LPS infusion for analysis of blood gases and acid base status (ABL 700, Radiometer, Copenhagen, Denmark).
Experimental design
Eighteen pigs were studied. Two pigs were studied each day. By pairwise randomization one pig was allocated to the LPS group (n = 9; E. coli 026:β 6, batch; 052K4066, Bacto Lipopolysaccharides, Difco Laboratories, Detroit, Mich., USA) and the other to the LPS plus rhAPC group (n = 9; Drotrecogin alfa, Xigris, Eli Lilly, Lyngby, Denmark) for 5 h and 15 min (Fig. 1). The animals received 20 ml/kg isotonic saline infusion per hour throughout the study period. The LPS group received an additional amount of saline matching the rhAPC infusion in the LPS+rhAPC group (2.5 ml/kg per hour). Hypoglycemia (blood glucose < 3 mmol/l) was treated with intravenous infusion of 5% glucose until normoglycemia was achieved. Severe shivering was treated with intravenous pethidine (10–50 mg). Extreme hypotension (MAP< 30 mmHg) was treated with intravenous epinephrine (0.01–0.05 mg), severe bradycardia (HR < 25) with intravenous atropine (0.1–0.2 mg), and ventricular fibrillation was with defibrillation, intravenous adrenaline, and intravenous amiodarone (150 mg). At study termination the animals were killed by intravenous injection of potassium chloride preceded by intravenous fentanyl. The main investigators were aware of the randomization during the experiments, but the laboratory technicians were blinded during the experiment and during data analysis. Power calculations based on preliminary coagulation data revealed the need for eight animals in each group (β = 0.80 with α = 0.05).
Activated protein C infusion
Infusion of 100 μg kg−1 h−1 rhAPC was started after 45 min and was continued throughout the trial period.
LPS-infusion
The LPS was dissolved in sterile water and diluted in saline one day prior to each experiment to dissolve any precipitate. At 60 min LPS infusion was started at baseline at a rate of 2.5 μg kg−1 h−1 and was increased stepwise to 15 μg kg−1 min−1 during the following 30 min. For the remaining trial period the infusion continued at a rate of 2.5 μg kg−1 h−1. If mean pulmonary artery pressure increased to levels above the mean systemic blood pressure, the LPS infusion was paused until the hemodynamics were stabilized (MAP > 50 mmHg and mean pulmonary artery pressure < 45 mmHg).
Cytokines, blood gases, and acid-base status
Blood for cytokines was sampled at 45 min (baseline), 120, 180, 240, 300, and 360 min. Blood gases, plasma lactate, and glucose were sampled every 30 min.
Cytokines
The protocol is modified from a previously published methods [15]. Fresh-frozen plasma samples (−80 °C) were obtained from EDTA-stabilized blood. In-house time-resolved fluorometric assay was used based on porcine specific matched pairs of anticytokine antibodies in combination with recombinant cytokine standards (R&D Systems, Abingdon, UK; cat. nos. MAB6902, BAF690, AF686, BAF686, MAB5351, BAF535, MAB6931, BAF693). Detection limits were: 0.045–6.25 ng/ml for TNF-α, 0.030–6.25 ng/ml for IL-6, 0.008–6.25 ng/ml for IL-8, and 0.010–6.25 ng/ ml for IL-10. Inter-assay variations were 4–10% and intra-assay variations 5%. All peak levels of cytokines were within the linearity range.
Samples, controls, and standards
All samples were analyzed in a dilution of 50% EDTA plasma and 50% dilution buffer [IL-6, IL-8, and IL-10: PBS, 2% bovine serum albumin (BSA) and 0.05% Tween-20; TNF-α: 1% BSA, and 0.05% Tween-20 in Tris-buffered NaCl, pH 7.3]. Standards were made of recombinant porcine cytokines, and standard curves were made in 50% dilution buffer and 50% pooled cytokine-free sterile-filtered porcine EDTA plasma. Two positive controls were measured in each plate. Standards and controls were measured in duplicates, while samples were measured in triplicates. All plates were run in a blinded manner. Standard curves were created using a four-parameter logistic curve fit (Microcal Origin, Mass., USA) where median sample concentrations were used.
Assay procedure
Microtiter plates (Nunc, Copenhagen, Denmark) were coated with capture antibody in PBS and were incubated for 18 h at 4 °C. Blocking unspecific binding sites was carried out with PBS, pH 7.4 containing 5% nonfat dried milk and 0.1% Tween-20 for 2 h. Plates were washed three times in 50 mM Tham, pH 7.3, 0.2% Tween-20 between all steps hereafter. Standards, samples, and controls were loaded and incubated for 2 h at room temperature and were then incubated with detecting antibody in dilution buffer for 2 h at room temperature. All detecting antibodies were biotinylated. After incubation with Eu3 plus streptavidin for 30 min (1:2000) in Assay Buffer (Wallac, Turku, Finland) 1 h of signal enhancement followed (Enhancement Solution, Wallac). The fluorescence of bound Europium (Eu3+) was measured by assay software (DELFIA, Multicalc, Wallac).
Leukocyte count and differential count
Leukocyte counts were obtained by diluting 25 μl EDTA-stabilized peripheral blood with 475 μl methylvioletacetate. Differential counts were May–Grünwald–Giemsa stained. All counts were performed by the same person using a Bürker–Türk chamber.
APC measurements
APC was measured by Maxygen (Hørsholm, Denmark) using enzyme-linked immunosorbent assay to capture free and non-inhibitor-bound APC. Plates were coated overnight at 4 °C using 5 μg/ml of a monoclonal antibody to human APC (HAPC 1555; kind gift of C. Esmon, Oklahoma Medical Research Foundation, Oklahoma City, Okla., USA). The coating buffer contained 20 mM Hepes pH 7.5, 150 mM NaCl, and 5 mM CaCl2. Plates were washed four times using 300 μl THT washing buffer (0.5 M Tris-HCl, 1 M NaCl, 0.05% Tween-20 and 10 mM CaCl2). Unoccupied sites were blocked with THT washing buffer containing 1% BSA incubated on a plate shaker in room temperature for 1 hour. The samples were again washed using 300 μl THT washing buffer. APC (Xigris), 100 ng/ml, was diluted in a dilution buffer containing THT 0.1% BSA, 0.03 M benzamidine, 10% plasma with 0.014 M citrate, 2.0 U/ml heparin, 20 mM hydroxyethylpiperazine ethanesulfonic acid (HEPES) pH 7.5, and 10 mM CaCl2. The APC were diluted 1:2 in eight following wells while the last well remained unused. The porcine samples were diluted 1:20 in a dilution buffer containing THT, 0.1% BSA, 0.03 M benzamidine, 5.25% plasma with 0.014 M citrate, 2.1 U/ml heparin, 21 mM HEPES pH 7.5, and 10.5 mM CaCl2. As a quality control 50, 10, 2, or 0 ng/ml APC was added directly to the well in THT and 0.1% BSA. The APC, samples, and quality control were incubated in room temperature for 1 h while gently shaking. All samples were washed in washing buffer, and 100 μl Spectrozyme PCa (cat. no. 336, American Diagnostica, Stamford, Conn., USA) was diluted in 0.5 mM in THT, 0.1% BSA, and 10 mM CaCl2 and was added to every well. The samples were incubated in 37 °C and absorbance in all wells was measured at 405 nm after 2 and 20 h.
TAT measurements and PAI-1 measurements
All TAT and plasminogen activator inhibitor (PAI) 1 activity was measured by Maxygen according to manufacture's protocols using Enzygnost TAT microassay (DadeBehringHolding, Liederbach, Germany) and porcine PAI-1 activity assay (Innovative Research, Southfield, Mich., USA).
Statistics
Data were ln-transformed to obtain normal distributions. Peak levels of TNF-α, IL-6, IL-8, and IL-10 were compared using Student's t-test, and time at peak level was analyzed using the Mann–Whitney U-test. PAI-1, TAT, lymphocytes, neutrophils, MAP, pO2, pCO2, lactate, pH, glucose, and cortisol measurements were compared using a multivariate analysis of variance model. All statistical analyses used Stata 9.2 software, and statistical significance was set at p < 0.05. No compensation for multiple comparisons was performed.
Results
Experimental design and control parameters
APC concentrations are shown in Fig. 2. APC was detectable in the rhAPC group but not in the LPS group. There was no significant difference over time or in mean levels of MAP, pO2, pCO2, lactate, pH, glucose, or cortisol between the two groups (all p > 0.05, multivariate analysis of variance). One animal from each group was excluded from the trial because of premature death; an LPS pig died just after anesthesia was induced and an LPS+APC pig 50 min after LPS infusion had commenced. Two animals in the LPS group received intravenous epinephrine and two others intravenous atropine. In the LPS+APC group one pig was given only atropine, and three pigs received both atropine and epinephrine intravenously. Pethidine was given to six animals in both groups (p = 0.42, Mann–Whitney U-test). One animal from the LPS+APC group was defibrillated and received amiodarone. The two groups followed the same fluid protocol, and a significant but equal increase in hemoglobin concentration was seen in both groups (from 45 to 360 min), indicating hemoconcentration.
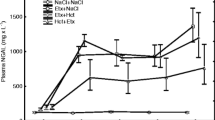
Cytokine data
Plasma cytokine concentrations in the two groups are shown in Fig. 3. There was no significant difference in peak plasma cytokine levels between the two groups (TNF-α, p = 0.65; IL-6, p = 0.79; IL-8, p = 0.56; IL-10, p = 0.82). TNF-α and IL-10 peaked significantly later in the rhAPC-treated animals (p = 0.01 and p = 0.04, respectively) while IL-6 and IL-8 levels did not peak at significantly different time points (p = 0.37 and p = 1.00, respectively).
Coagulation data
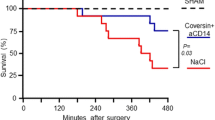
PAI-1 levels differed significantly between the two groups (Fig. 4), with decreased PAI-1 levels in the APC-treated animals (p = 0.004). There was no significant difference in TAT concentrations between the two groups (p = 0.19; Fig. 5).
Leukocyte data
Figure 6 shows the number of lymphocytes and neutrophils in peripheral blood. LPS administration induced a significant decrease in both lymphocytes and neutrophils but without significant differences between the groups (p = 0.10 and p = 0.61, respectively).
Discussion
In this porcine model of acute endotoxemia, rhAPC showed no difference in peak plasma levels of pro- or anti-inflammatory cytokines. However, TNF-α and IL-10 peaked significantly later in the rhAPC-treated animals. The study confirms the profibrinolytic effects of rhAPC demonstrated by decreased PAI-1 levels while no other effects on coagulation markers or metabolic or leukocyte data were detected.
We have previously shown in a similar endotoxemic porcine model that strict normoglycemic control during hyperinsulinemia attenuates the proinflammatory TNF-α response to LPS challenge [15]. Thus, if a cytokine-modulating effect of rhAPC is present, we anticipated detectable changes in plasma levels of the cytokines. In the present setup, however, we were unable to demonstrate any modifying effect of rhAPC on plasma levels of TNF-α, IL-6, IL-8, or IL-10 but did find that rhAPC significantly postponed the TNF-α and IL-10 peak.
These findings agree with previous human and animal studies. In a porcine endotoxemia trial Fourrier et al. [16] administered LPS for 30 min followed by infusion of protein C, antithrombin III, or both. Intervention with protein C increased MAP and systemic vascular resistance, and blunted the rise in lactate levels. No other differences were demonstrated between coagulation factors, cytokines, or leukocytes.
In two rat studies high-dose APC modified plasma cytokine response to high-dose LPS exposure [17, 18]. However, in human endotoxemia neither APC nor protein C zymogen had any effects on plasma cytokines [19–21]. Two of the studies showed increased activated partial thromboplastin time, but none of the three models of low-dose endotoxemia found any profibrinolytic, antithrombotic, or anti-inflammatory effects of APC.
Kalil et al. [19] found higher blood pressure and increased monocyte CD11b levels in APC-treated subjects compared to the placebo group. The difference in bloodpressure, however, was only significant at a single time point during 24 h. Monnet et al. [22] recently showed in a retrospective study that a lower dose of norepinephrine was required to maintain MAP in rhAPC-treated septic shock patients. In our study blood pressure was kept similar in the two groups in order to discern rhAPC effects on the cytokine response, and therefore we cannot assess the rhAPC effects on circulation. We are aware that supratherapeutic doses of APC can have opposing effects on endothelial cell permeability, which may decrease the MAP in treated animals [23]. Hence it appears that APC does not have a major effect on plasma cytokine levels in LPS exposed animals or humans. The finding of a significantly later peak in TNF-α and IL-10 levels in the rhAPC-treated animals indicates that cytokine-modulating effect of rhAPC could be present. However, the mechanism behind this delay is unknown.
The anti-inflammatory mechanisms of APC have also been investigated in in vitro and other animal studies. APC blocks nuclear factor κB nuclear translocation [24] and modulates endothelial cell gene expression into anti-inflammatory and antiapoptotic pathways [25]. Fur thermore, APC attenuates LPS induced TNF-α elaboration and production in mononuclear cells [26, 27]. Finally, APC inhibits leukocyte adhesion to the activated endothelium in vitro and in vivo which may contribute to the anti-inflammatory effects of APC [18, 28, 29]. Caution in interpreting the in vitro results is required since very high doses of APC were used in many of the studies.
In the present investigation the rhAPC infusion began 15 min prior to LPS stimulation whereas rhAPC was infused 2 h before LPS in both human studies. Both setups are indeed different from clinical rhAPC administration, but we chose this dosage (100 μg·kg−1·h−1) to assure that any rhAPC effect on inflammatory and coagulation markers would be revealed. The used rhAPC dose is close to four times higher than the recommended human dose, and the amount was chosen due to pilot studies showing rhAPC effects on coagulation markers. The APC concentrations measured in the LPS+rhAPC group were about 350–400 ng/ml while the levels in human studies have a median range between 40 and 60 ng/ml. The plasma concentrations in our animals were thus higher than could be expected from human data, and the reason for these remains unknown. This is, to our knowledge, the first study of porcine rhAPC data, and one could speculate whether the pharmacodynamics of rhAPC differs from that of native APC in pigs.
The human anti-inflammatory properties of rhAPC in vivo have been demonstrated so far only in severe septic patients as a significantly higher relative decrease in IL-6 plasma levels on days 1, 4, 5, 6, and 7 after rhAPC administration [8]. However, the absolute concentration of IL-6 seems to be similar in the control and intervention groups. Another human study has shown reduced leukocyte accumulation in the airspaces and decreased chemotaxis of neutrophils from bronchoalveolar lavage [30].
The profibrinolytic effect of rhAPC is thought to be mediated via two mechanisms: (a) APC is able to neutralize PAI-1 activity [31], and (b) it can attenuate the generation of a carboxypeptidase B-type enzyme [32], a thrombin activatable fibrinolysis inhibitor. According to Urano et al. [33], the profibrinolytic effects of APC are probably overestimated, but APC attenuates the coagulation-associated enhancement of fibrinolysis. We found this rhAPC effect as a significant decrease in PAI-1 levels in the rhAPC-treated animals. High rhAPC and LPS doses and continuous LPS infusion could be the reason that we were able to show the profibrinolytic effects of APC on PAI-1 in this trial.
The anti-thrombotic properties of APC are mediated in synergy with protein S. The two proteins combine to inactivate factors Va and VIIIa, resulting in decreased thrombin levels, which are the keystone in blood clots. The anticoagulative effects of rhAPC were measured as changes in TAT levels, but no significant difference was observed between the two groups. This could be due to either a type II error, differences in species specificity to rhAPC response, or questionable usefulness of human coagulation assays in porcine trials [34].
This study has limitations. First, the many potential differences between human and animal trials [35]. Although we controlled ventilation tightly and continuously monitored and maintained blood pressure with saline infusion, several factors remain different from human trials: uncontrolled prior contaminated environments, young healthy animals, early treatment, rapid onset of stimuli, and lack of comorbidities. Although many precautions have been taken to optimize this animal study, another contributing factor to our results could be the difference between the porcine and the human coagulation system. Second, we induced a systemic inflammatory condition by infusion of endotoxin, which produces a different picture than infection with microbiological agents. Third, we investigated only a limited number of animals, and, finally, only a few of the many inflammatory markers in plasma were measured.
We do, however, have a reproducible model of acute endotoxemia and organ dysfunction in which we previously have been able to modify the cytokine response by intervention. Since we were unable to modify the plasma cytokine levels with rhAPC in our high-dose endotoxemia model, our results confirm findings reported in the international literature suggesting that anti-inflammatory properties of APC cannot be detected as changes in plasma cytokine levels [36]. However, although data indicate that rhAPC might delay the peak plasma TNF-α and IL-10 levels, the mechanisms and consequences for this delay are unknown and should be addressed in future studies.
Conclusion
We found no significant effect of rhAPC on plasma levels of pro- or anti-inflammatory cytokines in this porcine model of acute endotoxemia, but we did find a significant delay in the peak levels of TNF-α and IL-10. In concordance with earlier studies, we found a modifying effect on the coagulation system confirming the profibrinolytic effects at very high doses of rhAPC. These results indicate that the possible anti-inflammatory effects of APC are not elicited through attenuation of plasma cytokine levels.
References
Brun-Buisson C, Meshaka P, Pinton P, Vallet B (2004) EPISEPSIS: a reappraisal of the epidemiology and outcome of severe sepsis in French intensive care units. Intensive Care Med 30:580–588
Angus DC, Linde-Zwirble WT, Lidicker J, Clermont G, Carcillo J, Pinsky MR (2001) Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med 29:1303–1310
Taylor FB Jr, Chang A, Esmon CT, D'Angelo A, Vigano-D'Angelo S, Blick KE (1987) Protein C prevents the coagulopathic and lethal effects of Escherichia coli infusion in the baboon. J Clin Invest 79:918–925
Faust SN, Levin M, Harrison OB, Goldin RD, Lockhart MS, Kondaveeti S, Laszik Z, Esmon CT, Heyderman RS (2001) Dysfunction of endothelial protein C activation in severe meningococcal sepsis. N Engl J Med 345:408–416
Sajan I, Da-Silva SS, Dellinger RP (2004) Drotrecogin alfa (activated) in an infant with gram-negative septic shock. J Intensive Care Med 19:51–55
White B, Livingstone W, Murphy C, Hodgson A, Rafferty M, Smith OP (2000) An open-label study of the role of adjuvant hemostatic support with protein C replacement therapy in purpura fulminans-associated meningococcemia. Blood 96:3719–3724
Rintala E, Kauppila M, Seppala OP, Voipio-Pulkki LM, Pettila V, Rasi V, Kotilainen P (2000) Protein C substitution in sepsis-associated purpura fulminans. Crit Care Med 28:2373–2378
Bernard GR, Vincent JL, Laterre PF, LaRosa SP, Dhainaut JF, Lopez-Rodriguez A, Steingrub JS, Garber GE, Helterbrand JD, Ely EW, Fisher CJ Jr (2001) Efficacy and safety of recombinant human activated protein C for severe sepsis. N Engl J Med 344:699–709
Mackenzie AF (2005) Activated protein C: do more survive? Intensive Care Med 31:1624–1626
Vincent JL (2006) Sepsis in the ICU: who needs progress? Intensive Care Med 32:609
Warren BL, Eid A, Singer P, Pillay SS, Carl P, Novak I, Chalupa P, Atherstone A, Penzes I, Kubler A, Knaub S, Keinecke HO, Heinrichs H, Schindel F, Juers M, Bone RC, Opal SM (2001) Caring for the critically ill patient. High-dose antithrombin III in severe sepsis: a randomized controlled trial. JAMA 286:1869–1878
Fourrier F, Jourdain M, Tournois A, Caron C, Goudemand J, Chopin C (1995) Coagulation inhibitor substitution during sepsis. Intensive Care Med 21 (Suppl 2):S264–S268
Abraham E, Reinhart K, Opal S, Demeyer I, Doig C, Rodriguez AL, Beale R, Svoboda P, Laterre PF, Simon S, Light B, Spapen H, Stone J, Seibert A, Peckelsen C, De DC, Postier R, Pettila V, Artigas A, Percell SR, Shu V, Zwingelstein C, Tobias J, Poole L, Stolzenbach JC, Creasey AA (2003) Efficacy and safety of tifacogin (recombinant tissue factor pathway inhibitor) in severe sepsis: a randomized controlled trial. JAMA 290:238–247
Nielsen JS, Larsson A, Rix T, Nyboe R, Gjedsted J, Krog J, Ledet T, Tønnesen E (2006) Activated protein C's effects on plasma cytokines during acute endotoxemia in pigs. Intensive Care Med 32(13):74
Brix-Christensen V, Andersen SK, Andersen R, Mengel A, Dyhr T, Andersen NT, Larsson A, Schmitz O, Orskov H, Tonnesen E (2004) Acute hyperinsulinemia restrains endotoxin-induced systemic inflammatory response: an experimental study in a porcine model. Anesthesiology 100:861–870
Fourrier F, Jourdain M, Tournoys A, Gosset P, Mangalaboyi J, Chopin C (1998) Effects of a combined antithrombin III and protein C supplementation in porcine acute endotoxic shock. Shock 10:364–370
Murakami K, Okajima K, Uchiba M, Johno M, Nakagaki T, Okabe H, Takatsuki K (1997) Activated protein C prevents LPS-induced pulmonary vascular injury by inhibiting cytokine production. Am J Physiol 272:L197–L202
Favory R, Lancel S, Chal X, Tissier S, Neviere R (2006) Cardiovascular protective role for activated protein C during endotoxemia in rats. Intensive Care Med 32:899–905
Kalil AC, Coyle SM, Um JY, LaRosa SP, Turlo MA, Calvano SE, Sundin DP, Nelson DR, Lowry SF (2004) Effects of drotrecogin alfa (activated) in human endotoxemia. Shock 21:222–229
Spiel AO, Firbas C, Mayr FB, Leitner JM, Schmidt B, Knobl P, Varadi K, Jilma B (2005) The effects of supra-normal protein C levels on markers of coagulation, fibrinolysis and inflammation in a human model of endotoxemia. Thromb Haemost 94:1148–1155
Derhaschnig U, Reiter R, Knobl P, Baumgartner M, Keen P, Jilma B (2003) Recombinant human activated protein C (rhAPC drotrecogin alfa [activated]) has minimal effect on markers of coagulation, fibrinolysis, and inflammation in acute human endotoxemia. Blood 102:2093–2098
Monnet X, Lamia B, Anguel N, Richard C, Bonmarchand G, Teboul JL (2005) Rapid and beneficial hemodynamic effects of activated protein C in septic shock patients. Intensive Care Med 31:1573–1576
Zeng W, Matter WF, Yan SB, Um SL, Vlahos CJ, Liu L (2004) Effect of drotrecogin alfa (activated) on human endothelial cell permeability and Rho kinase signaling. Crit Care Med 32:S302–S308
White B, Schmidt M, Murphy C, Livingstone W, O'Toole D, Lawler M, O'Neill L, Kelleher D, Schwarz HP, Smith OP (2000) Activated protein C inhibits lipopolysaccharide-induced nuclear translocation of nuclear factor kappaB (NF-kappaB) and tumour necrosis factor alpha (TNF-alpha) production in the THP-1 monocytic cell line. Br J Haematol 110:130–134
Joyce DE, Gelbert L, Ciaccia A, DeHoff B, Grinnell BW (2001) Gene expression profile of antithrombotic protein c defines new mechanisms modulating inflammation and apoptosis. J Biol Chem 276:11199–11203
Hancock WW, Grey ST, Hau L, Akalin E, Orthner C, Sayegh MH, Salem HH (1995) Binding of activated protein C to a specific receptor on human mononuclear phagocytes inhibits intracellular calcium signaling and monocyte-dependent proliferative responses. Transplantation 60:1525–1532
Grey ST, Tsuchida A, Hau H, Orthner CL, Salem HH, Hancock WW (1994) Selective inhibitory effects of the anticoagulant activated protein C on the responses of human mononuclear phagocytes to LPS, IFN-gamma, or phorbol ester. J Immunol 153:3664–3672
Hoffmann JN, Vollmar B, Laschke MW, Inthorn D, Fertmann J, Schildberg FW, Menger MD (2004) Microhemodynamic and cellular mechanisms of activated protein C action during endotoxemia. Crit Care Med 32:1011–1017
Grinnell BW, Hermann RB, Yan SB (1994) Human protein C inhibits selectin-mediated cell adhesion: role of unique fucosylated oligosaccharide. Glycobiology 4:221–225
Nick JA, Coldren CD, Geraci MW, Poch KR, Fouty BW, O'Brien J, Gruber M, Zarini S, Murphy RC, Kuhn K, Richter D, Kast KR, Abraham E (2004) Recombinant human activated protein C reduces human endotoxin-induced pulmonary inflammation via inhibition of neutrophil chemotaxis. Blood 104:3878–3885
Sakata Y, Loskutoff DJ, Gladson CL, Hekman CM, Griffin JH (1986) Mechanism of protein C-dependent clot lysis: role of plasminogen activator inhibitor. Blood 68:1218–1223
Bajzar L, Nesheim ME, Tracy PB (1996) The profibrinolytic effect of activated protein C in clots formed from plasma is TAFI-dependent. Blood 88:2093–2100
Urano T, Castellino FJ, Ihara H, Suzuki Y, Ohta M, Suzuki K, Mogami H (2003) Activated protein C attenuates coagulation-associated over-expression of fibrinolytic activity by suppressing the thrombin-dependent inactivation of PAI-1. J Thromb Haemost 1:2615–2620
Munster AM, Olsen AK, Bladbjerg EM (2002) Usefulness of human coagulation and fibrinolysis assays in domestic pigs. Comp Med 52:39–43
Esmon CT (2004) Why do animal models (sometimes) fail to mimic human sepsis? Crit Care Med 32:S219–S222
Macias WL, Yan SB, Williams MD, Um SL, Sandusky GE, Ballard DW, Planquois JM (2005) New insights into the protein C pathway: potential implications for the biological activities of drotrecogin alfa (activated). Crit Care 9(Suppl 4):S38–S45
Acknowledgements
Maxygen is thankfully acknowledged for their cooperation and work on the coagulation data. The biostatistical skills of Niels Trolle, Ph.D. (Department of Biostatistics, Aarhus University, Aarhus, Denmark), the skilled technical assistance of the technicians Lene Vestergaard (Department of Anesthesiology and Intensive Care, Aarhus University Hospital) and Henrik Sørensen (Clinical Institute, Aarhus University Hospital) are also gratefully acknowledged.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nielsen, J.S., Larsson, A., Rix, T. et al. The effect of activated protein C on plasma cytokine levels in a porcine model of acute endotoxemia. Intensive Care Med 33, 1085–1093 (2007). https://doi.org/10.1007/s00134-007-0631-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-007-0631-1