Abstract
Objective
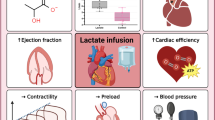
We examined whether lactate availability is a limiting factor for heart function during endotoxic shock, and whether lactate deprivation thus induces heart energy depletion, thereby altering cardiovascular performance. The study goals were to determine whether muscle lactate production is linked to β2-stimulation and to ascertain the effects of systemic lactate deprivation on hemodynamics, lactate metabolism, heart energetics, and outcome in a lethal model of rat's endotoxic shock.
Interventions
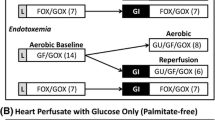
We modulated the adrenergic pathway in skeletal muscle using microdialysis with ICI-118551, a selective β2-blocker. Muscle lactate formation in endotoxic shock was further inhibited by intravenous infusion of ICI-118551 or dichloroacetate (DCA), an activator of pyruvate dehydrogenase (DCA) and their combination.
Results
Muscle lactate formation was decreased by ICI-118551. During endotoxic shock both ICI-118151 and DCA decreased circulating and heart lactate concentrations in parallel with a decrease in tissue ATP content. The combination ICI-118551-DCA resulted in early cardiovascular collapse and death. The addition of molar lactate to ICI-1185111 plus DCA blunted the effects of ICI-118551+DCA on hemodynamics. Survival was markedly less with ICI-118551 than with endotoxin alone.
Conclusion
Systemic lactate deprivation is detrimental to myocardial energetics, cardiovascular performance, and outcome.




Similar content being viewed by others
References
Krishnagopalan S, Kumar A, Parrillo JE (2002) Myocardial dysfunction in the patient with sepsis. Curr Opin Crit Care 8:376–388
Lancel S, Tissier S, Mordon S, Marechal X, Depontieu F, Scherpereel A, Chopin C, Neviere R (2004) Peroxynitrite decomposition catalysts prevent myocardial dysfunction and inflammation in endotoxemic rats. J Am Coll Cardiol 43:2348–2358
Gibot S, Levy B, Neviere R, Cariou A, Lesur O (2004) [Myocardial dysfunction and septic shock]. Med Sci (Paris) 20:1115–1118
James JH, Luchette FA, McCarter FD, Fischer JE (1999) Lactate is an unreliable indicator of tissue hypoxia in injury or sepsis. Lancet 354:505–508
Levy B, Gibot S, Franck P, Cravoisy A, Bollaert PE (2005) Relation between muscle Na+K+ ATPase activity and raised lactate concentrations in septic shock: a prospective study. Lancet 365:871–875
Liggett SB, Shah SD, Cryer PE (1988) Characterization of beta-adrenergic receptors of human skeletal muscle obtained by needle biopsy. Am J Physiol 254:E795–E798
Chatham JC (2002) Lactate—the forgotten fuel! J Physiol 542:333
Salem JE, Stanley WC, Cabrera ME (2004) Computational studies of the effects of myocardial blood flow reductions on cardiac metabolism. Biomed Eng Online 3:15
Tessier JP, Thurner B, Jungling E, Luckhoff A, Fischer Y (2003) Impairment of glucose metabolism in hearts from rats treated with endotoxin. Cardiovasc Res 60:119–130
Rosdahl H, Ungerstedt U, Henriksson J (1997) Microdialysis in human skeletal muscle and adipose tissue at low flow rates is possible if dextran-70 is added to prevent loss of perfusion fluid. Acta Physiol Scand 159:261–262
Hickner RC, Rosdahl H, Borg I, Ungerstedt U, Jorfeldt L, Henriksson J (1992) The ethanol technique of monitoring local blood flow changes in rat skeletal muscle: implications for microdialysis. Acta Physiol Scand 146:87–97
Oberbeck R, Schmitz D, Wilsenack K, Schuler M, Pehle B, Schedlowski M, Exton MS (2004) Adrenergic modulation of survival and cellular immune functions during polymicrobial sepsis. Neuroimmunomodulation 11:214–223
James JH, Wagner KR, King JK, Leffler RE, Upputuri RK, Balasubramaniam A, Friend LA, Shelly DA, Paul RJ, Fischer JE (1999) Stimulation of both aerobic glycolysis and Na(+)-K(+)-ATPase activity in skeletal muscle by epinephrine or amylin. Am J Physiol 277:E176–E186
Clausen T, Flatman JA (1980) Beta 2-adrenoceptors mediate the stimulating effect of adrenaline on active electrogenic Na-K-transport in rat soleus muscle. Br J Pharmacol 68:749–755
Levy B, Mansart A, Bollaert PE, Franck P, Mallie JP (2003) Effects of epinephrine and norepinephrine on hemodynamics, oxidative metabolism, and organ energetics in endotoxemic rats. Intensive Care Med 29:292–300
Saupe KW, Eberli FR, Ingwall JS, Apstein CS (2001) Metabolic support as an adjunct to inotropic support in the hypoperfused heart. J Mol Cell Cardiol 33:261–269
Nakamura K, Kusuoka H, Ambrosio G, Becker LC (1993) Glycolysis is necessary to preserve myocardial Ca2+ homeostasis during beta-adrenergic stimulation. Am J Physiol 264:H670–H678
Mustafa I, Leverve XM (2002) Metabolic and hemodynamic effects of hypertonic solutions: sodium-lactate versus sodium chloride infusion in postoperative patients. Shock 18:306–310
Chiolero RL, Revelly JP, Leverve X, Gersbach P, Cayeux MC, Berger MM, Tappy L (2000) Effects of cardiogenic shock on lactate and glucose metabolism after heart surgery. Crit Care Med 28:3784–3791
Schurr A, Payne RS, Miller JJ, Rigor BM (1997) Brain lactate is an obligatory aerobic energy substrate for functional recovery after hypoxia: further in vitro validation. J Neurochem 69:423–426
Luptak I, Balschi JA, Xing Y, Leone TC, Kelly DP, Tian R (2005) Decreased contractile and metabolic reserve in peroxisome proliferator-activated receptor-alpha-null hearts can be rescued by increasing glucose transport and utilization. Circulation 112:2339–2346
Johannsson E, Lunde PK, Heddle C, Sjaastad I, Thomas MJ, Bergersen L, Halestrap AP, Blackstad TW, Ottersen OP, Sejersted OM (2001) Upregulation of the cardiac monocarboxylate transporter MCT1 in a rat model of congestive heart failure. Circulation 104:729–734
Smith HJ, Halliday SE, Earl DC, Stribling D (1983) Effects of selective (beta-1 and beta-2) and nonselective beta adrenoceptor antagonists on the cardiovascular and metabolic responses to isoproterenol: comparison with ICI 141:292. J Pharmacol Exp Ther 226:211–216
Linderman JK, Dallman PR, Rodriguez RE, Brooks GA (1993) Lactate is essential for maintenance of euglycemia in iron-deficient rats at rest and during exercise. Am J Physiol 264:E662–E667
Ventura-Clapier R, Garnier A, Veksler V (2004) Energy metabolism in heart failure. J Physiol 555:1–13
Dhainaut JF, Huyghebaert MF, Monsallier JF, Lefevre G, Dall'Ava-Santucci J, Brunet F, Villemant D, Carli A, Raichvarg D (1987) Coronary hemodynamics and myocardial metabolism of lactate, free fatty acids, glucose, and ketones in patients with septic shock. Circulation 75:533–541
Kline JA, Thornton LR, Lopaschuk GD, Barbee RW, Watts JA (2000) Lactate improves cardiac efficiency after hemorrhagic shock. Shock 14:215–221
Barbee RW, Kline JA, Watts JA (2000) Depletion of lactate by dichloroacetate reduces cardiac efficiency after hemorrhagic shock. Shock 14:208–214
Stacpoole PW, Harman EM, Curry SH, Baumgartner TG, Misbin RI (1983) Treatment of lactic acidosis with dichloroacetate. N Engl J Med 309:390–396
Gong H, Sun H, Koch WJ, Rau T, Eschenhagen T, Ravens U, Heubach JF, Adamson DL, Harding SE (2002) Specific beta (2) AR blocker ICI 118:551 actively decreases contraction through a G(i)-coupled form of the beta (2) AR in myocytes from failing human heart. Circulation 105:2497–2503
Stacpoole PW, Nagaraja NV, Hutson AD (2003) Efficacy of dichloroacetate as a lactate-lowering drug. J Clin Pharmacol 43:683–691
Gladden LB (2004) Lactate metabolism—a new paradigm for the third millennium. J Physiol 558:5–30
Leverve XM, Mustafa I (2002) Lactate: a key metabolite in the intercellular metabolic interplay. Crit Care 6:284–285
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is discussed in the editorial available at: http://dx.doi.org/10.1007/s00134-006-0524-8
Rights and permissions
About this article
Cite this article
Levy, B., Mansart, A., Montemont, C. et al. Myocardial lactate deprivation is associated with decreased cardiovascular performance, decreased myocardial energetics, and early death in endotoxic shock. Intensive Care Med 33, 495–502 (2007). https://doi.org/10.1007/s00134-006-0523-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-006-0523-9