Abstract
Objective
Two technologies to acquire beat-to-beat stroke volume values exist, pulse contour analysis and esophageal Doppler monitoring. Pulse contour analysis assumes fixed aortic impedance. Esophageal Doppler assumes a constant proportional descending aortic flow and diameter. These assumptions may not be correct as arterial tone or myocardial contractility vary. We tested these relationships in the setting of rapidly changing stroke volumes and different cardiovascular states over a period of 10–15 cardiac cycles.
Design and setting
In a university research facility we compared beat-to-beat changes in stroke volume as measure by aortic root flow probe or conductance catheter to pulse contour analysis and stroke distance as measured by esophageal Doppler.
Subjects
Five purpose-bred research hounds.
Interventions
To obtain a wide range of rapidly changing stroke volumes measurements were made during transient inferior vena cava occlusion. Data were gathered under baseline conditions and during norepinephrine, nitroprusside, and dobutamine infusions.
Measurements and results
The pulse contour stroke volumes and esophageal Doppler stroke distance paralleled flow probe stroke volumes under all conditions (R 2 = 0.89 for all measures). However, the absolute changes and proportional changes and the absolute values for both surrogate measures differed from absolute stroke volumes. Bland-Altman analysis showed no consistent bias or degree of precision across all animals under any given cardiovascular state.
Conclusions
Both pulse contour stroke volumes and esophageal Doppler derived stroke distance estimates yield significant correlations with aortic root flow probe. However, the absolute values, absolute changes, or proportional changes may not reflect actual stroke volumes as cardiovascular state varies, making their use in estimating absolute changes in stroke volume potentially inaccurate.





Similar content being viewed by others
References
Side CD, Gosling RG (1971) Non-surgical assessment of cardiac function. Nature 232:335–336
Singer M, Clarke J, Bennett ED (1989) Continuous hemodynamic monitoring by esophageal Doppler. Crit Care Med 17:447–452
Singer M, Bennett ED (1991) Noninvasive optimization of left ventricular filling using esophageal Doppler. Crit Care Med 19:1132–1137
Valtier B, Cholley BP, Belot JP, de la Coussaye JE, Mateo J, Payen DM (1998) Noninvasive monitoring of cardiac output in critically ill patients using transesophageal Doppler. Am J Respir Crit Care Med 158:77–83
Della Rocca G, Costa MG, Pompei L, Coccia C, Pietropaoli P (2002) Continuous and intermittent cardiac output measurement: pulmonary artery catheter versus aortic transpulmonary technique. Br J Anaesth 88:350–356
Godje O, Thiel C, Lamm P, Reichenspurner H, Schmitz C, Schutz A, Reichart B (1999) Less invasive, continuous hemodynamic monitoring during minimally invasive coronary surgery. Ann Thorac Surg 68:1532–1536
Zollner C, Haller M, Weis M, Morstedt K, Lamm P, Kilger E, Goetz AE (2000) Beat-to-beat measurement of cardiac output by intravascular pulse contour analysis: a prospective criterion standard study in patients after cardiac surgery. J Cardiothorac Vasc Anesth 14:125–129
Godje O, Hoke K, Goetz AE, Felbinger TW, Reuter DA, Reichart B, Friedl R, Hannekum A, Pfeiffer UJ (2002) Reliability of a new algorithm for continuous cardiac output determination by pulse-contour analysis during hemodynamic instability. Crit Care Med 30:52–58
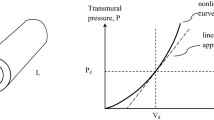
Wesseling K, Jansen J, Settels J, Schreuder J (1993) Computation of aortic flow from pressure in humans using a nonlinear, three-element model. J Appl Physiol 74:2566–2573
Feissel M, Michard F, Mangin I, Ruyer O, Faller JP, Teboul JL (2001) Respiratory changes in aortic blood velocity as an indicator of fluid responsiveness in ventilated patients with septic shock. Chest 119:867–873
Arndt JO, Mikat M, Parasher C (1984) Fentanyl's analgesic, respiratory, and cardiovascular actions in relation to dose and plasma concentration in unanesthetized dogs. Anesthesiology 61:355–361
Flacke JW, Davis LJ, Flacke WE, Bloor BC, Van Etten AP (1985) Effects of fentanyl and diazepam in dogs deprived of autonomic tone. Anesth Analg 64:1053–1059
Hirsch LJ, Rooney MW, Mathru M, Rao TL (1993) Effects of fentanyl on coronary blood flow distribution and myocardial oxygen consumption in the dog. J Cardiothorac Vasc Anesth 7:50–54
Linton NWF, Linton RAF (2001) Estimation of changes in cardiac output from the arterial blood pressure waveform in the upper limb. Br J Anaesth 86:486–496
Monnet X, Rienzo M, Osman D, Anguel N, Richard C, Pinsky MR, Teboul JL (2005) Esophageal Doppler monitoring predicts fluid responsiveness in critically ill ventilated patients. Intensive Care Med 31:1195–1201
Fisher LD, Belle GV (1993) Biostatistics: a methodology for the health sciences, 1st edn. Wiley, New York
Acknowledgements
We thank Linda Santelices for her expert assistance with MATLAB.
Author information
Authors and Affiliations
Corresponding author
Additional information
M.R.P. has the following potential conflicts of interest regarding this study: (a) He received unrestricted funding from both Deltex Inc. and Pulsion Ltd. to perform the clinical trial reported in this manuscript. Both companies received copies of their own data from trial prior to its submission for their critique of the technical aspects of the data collection and analysis. Neither company's input changed any of the data presented or its interpretation. (b) Following this study M.R.P. became a consultant to Arrow International, Edwards LifeSciences, and Lido Ltd., none of which companies' equipment was used in this study, but all these companies compete with Deltex and Pulsion for market share. (c) M.R.P. has received honoraria for lectures on hemodynamic monitoring from Edward LifeSciences and Arrow International. (d) M.R.P. is the inventor of a University of Pittsburgh patented hemodynamic monitoring protocol that uses dynamic changes in aortic pressure and flow to diagnose cardiovascular insufficiency. Thus the limitations of the devices reported in this study will impact on the utility of these approaches. M.R.P. also received a royalty from Arrow International for the use of his patented approach.
Rights and permissions
About this article
Cite this article
Gunn, S.R., Kim, H.K., Harrigan, P.W.J. et al. Ability of pulse contour and esophageal Doppler to estimate rapid changes in stroke volume. Intensive Care Med 32, 1537–1546 (2006). https://doi.org/10.1007/s00134-006-0284-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-006-0284-5