Abstract
Objective
The impact of lung-recruitment maneuvers on heart function at different volemic levels has not been studied in detail. We therefore investigated the effect on central hemodynamics of lung recruitment maneuvers at hypovolemia, normovolemia and hypervolemia in experimental lung injury.
Design
Randomized, controlled, cross-over experimental study.
Setting
Animal laboratory at a university hospital. Participants: Eleven anesthetized and lung-lavaged pigs.
Intervention
The animals were randomized to 10-s lung recruitment maneuvers followed by 30-s maneuvers (40 cm H2O airway pressure) or vice versa, performed under hypovolemia, normovolemia and hypervolemia.
Measurements and main results
Left-ventricular end-diastolic diameter and cardiac output were measured before, during, and 1 min and 5 min after the lung recruitment maneuver and left-ventricular eccentricity index was calculated for before and during the maneuver. Cardiac output and left-ventricular end-diastolic diameter (within parentheses) decreased significantly during both the 10-s and 30-s lung recruitment maneuvers at hypovolemia, by a mean of 89% (35) and 92% (33), at normovolemia by 75% (33) and 86% (32), and at hypervolemia by 56% (32) and 64% (43), respectively. At hypovolemia, cardiac output was increased above baseline 1–5 min following the 30-s maneuver. Left-ventricular eccentricity index increased significantly during the maneuver, indicating right ventricular dysfunction.
Conclusions
In this animal lung injury model, lung recruitment maneuvers significantly decreased left-ventricular end-diastolic volume and cardiac output at hypovolemia. Hypervolemia did partly counteract this compromise. In addition, a marked right-ventricular dysfunction during the maneuver was found.
Similar content being viewed by others
Introduction
Acute lung injury (ALI) with its more severe form, acute respiratory distress syndrome (ARDS), is an inflammatory condition in the lungs causing edema, collapse and hypoxemia [1]. Lung recruitment maneuvers reduce the amount of lung collapse, decrease intra-pulmonary shunt and improve arterial oxygenation in the early form of this condition, as well as in lung collapse induced by anesthesia or surgery [2, 3, 4, 5, 6, 7]. Although many studies on lung recruitment maneuvers have concluded that the hemodynamic side effect is either absent or unimportant, lung recruitment maneuvers produce both high intrathoracic and transpulmonary pressures leading to a decrease in systemic venous return and a probable increase in right ventricular afterload. Both mechanisms hamper right ventricular outflow and, as a consequence, reduce left ventricular filling and cardiac output [8, 9, 10]. Thus, in recent years, many studies have shown that cardiovascular side effects by lung recruitment maneuvers are present in both clinical and experimental settings [6, 11, 12, 13, 14, 15, 16]. We have recently demonstrated in circulatory stable patients immediately after cardiac surgery that lung recruitment maneuvers importantly reduced cardiac output and the left-ventricular end-diastolic volume [17].
Clinically, it is known that the hemodynamic side effects of lung recruitment maneuvers may be augmented by hypovolemia and ameliorated by hypervolemia, and the latter has recently been shown by Odenstedt and coworkers [14] in a porcine lung-injury model. However, no study, as we are aware of, has carefully examined the central hemodynamics and changes in heart function and volumes with echocardiography in combination with continuous registration of pulmonary blood flow during lung recruitment maneuvers at different volemic levels. In particular, the effect of a lung recruitment maneuver at hypovolemia has not, to our knowledge, been studied previously.
We therefore, in an experimental lung injury model, aimed to study the effects of two durations of lung recruitment maneuvers on intrathoracic vascular pressures and flows, as well as on the cardiac function and left ventricular filling during hypovolemia, normovolemia and hypervolemia [18]. In order to avoid any interference from lung volume gain on the circulatory effects by the lung recruitment maneuvers at the different volemic levels, zero end-expiratory pressure was used during the experiment [19].
Materials and methods
The study was approved by the local animal ethics committee. Eleven pigs, 26–39 kg, were pre-medicated with zolepam/tilamine 6 mg/kg, atropine 0.04 mg/kg and xylazine 2.2 mg/kg i.m. Before intubation, a bolus dose of 200 μg fentanyl was given I.V. Tracheal intubation was done orally, and the lungs were ventilated with a Servo 300 (Siemens-Elema, Solna, Sweden), using volume-controlled ventilation, FiO2 0.7 and tidal volume 8 ml/kg. Peak pressure was below 35 cmH2O, and respiratory frequency was set to keep end tidal CO2 38–53 mmHg (5–7 kPa). Anesthesia was maintained with ketamine 20 mg/kg/h, fentanyl 4 μg/kg/h and pancuronium 240 μg/kg/h. An I.V. solution of 2.5% glucose with 70 mmol Na, 45 mmol Cl and 25 mmol acetate (Rehydrex, Kabi Fresenius, Halden, Norway) was administered with a rate of 20 ml/kg the first hour after induction of anesthesia, after which 10 ml/kg/h was given throughout the study period.
Instrumentation, monitoring, measurements and interventions
Catheters were placed in the femoral artery, the carotid artery and the external jugular vein for monitoring of intravascular blood pressures. A pulmonary artery catheter was placed via the external jugular vein to monitor pulmonary artery pressure. In addition, heart rate, ECG and end-tidal CO2 and rectal temperature were monitored.
A median sternotomy was performed and an ultrasound probe connected to a calibrated ultrasonic blood flow meter (T201, Transonic Systems, Ithaca, NY, USA) was placed on the pulmonary artery to measure cardiac output with transit-time ultrasonic technique [19]. In one animal, another ultrasound probe was placed around the ascending aorta for measurement of aortic blood flow (T201, Transonic Systems, Ithaca, NY, USA). In order to assess the volume changes of the left ventricle, echocardiography was performed (Philips Sonos 7500, Philips, Bothwell, WA, USA). A TEE probe (Philips OmniPlane II) was placed in the pericardium on the dorsolateral part of the left ventricle for measuring short axis diastolic and systolic changes of the left ventricle. In one animal, the probe was adjusted so the right ventricular function could be evaluated. After placement of the probes, the sternum was closed. Loops containing three cardiac cycles, recorded before, at the end of, and 1 min and 5 min after each lung recruitment maneuver, were stored digitally. From the stored loops, an investigator, blinded to the intervention, measured left-ventricular end-diastolic and end-systolic diameters. The septo-lateral diameter (D1) and a diameter orthogonal to it (D2) were measured. From these measurements, the fractional shortening and eccentricity index (EI = end-systolicD2/end-systolicD1) were calculated. A high systolic EI represents a flatter intraventricular septum, indicating raised right ventricular pressure [20]. End-expiratory lung volume was measured by sulfur hexafluoride washout [21].
Interventions
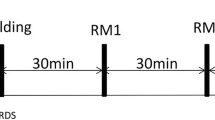
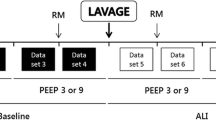
After closure of the sternum, a period of 15 min of ventilation with 125% of initial minute volume was initiated, in order to prevent hypercapnia during the following lung-lavage procedure. The lungs were lavaged with 10 ml/kg of body temperature saline, repeated eight times. After the lung lavage, the initial ventilator settings were used. The circulatory effect of lung recruitment maneuver (LRM) was studied during hypovolemia, normovolemia and hypervolemia, or the reverse order, leaving the normovolemic level to be interpolated between hypovolemia and hypervolemia. The order of volemic status was randomized by sealed envelopes. Blood volume was estimated as 179 × body weight × body weight(−0.27) [22]. When the order of volemic stages was hypovolemia, normovolemia and hypervolemia, hypovolemia was achieved by venesection of 15% of the estimated blood volume, normovolemia by re-transfusion of the tapped blood (which was stored at room temperature in SAGMAN solution) and hypervolemia by infusion of a volume equal to 15% of the estimated blood volume with 3% dextran in Ringer's solution (Ringer-dextran, Pharmalink, Upplands Väsby, Sweden). When the order of volemic stages was reversed, hypervolemia was achieved with infusion of a volume equal to 15% of the blood volume of 3% dextran in Ringer's solution and normovolemia and hypovolemia by venesection of a blood volume equal to 15%, and further 15% of the estimated blood volume, respectively. The infusion or removal of blood was done over a 10-min period and was followed by a 5-min stabilization period before new measurements were made. During each volemic stage, two LRMs were performed with a sustained pressure technique using the CPAP-mode on the ventilator to create an airway pressure of 40 cmH2O for 10 s and 30 s, respectively. The order of the LRMs was randomized, and a second LRM was done 10 min after the first one. After each LRM, the ventilation was set back to the pre-LRM setting with zero end-expiratory airway pressure (Fig. 1).
Arterial, pulmonary-artery and central-venous blood pressures were recorded along with the heart rate throughout the whole study session. Before and at the end of, as well as 1 min and 5 min after the LRMs, echocardiographic short-axis view of the left ventricle and cardiac output were registered. In addition, arterial blood gas measurements were done before and 1 min after the LRM. End-expiratory lung volume was measured before and after the LRM. Although the tracer gas wash-in/wash-out sequence was started 1 min after the LRM, due to the time for equilibration of the tracer gas in the lungs, the actual measurement was made by 2–4 min following the LRM and is registered at 5 min in Table 1.
Statistics
Comparisons between the two durations of LRM were done with Wilcoxon test for means, and comparisons between the three volemic levels were done with nonparametric one-way ANOVA (Kruskal--Wallis test) using SAS 9.1 statistical package (SAS institute, Cary, NC, USA). Comparisons between the different measurement points (before vs end, before vs 1 min after and 5 min after the LRM) were done with Wilcoxon test for means with Bonferroni correction. Results are presented as mean ± SD, if not otherwise indicated. p < 0.05 was considered significant, except for comparisons between the different measurement points, where p < 0.017 was considered significant.
Results
Results are presented from nine animals, as one animal died during the preparation due to unintended right-coronary artery clamping, and one animal developed a septic shock-like condition due to a probable pneumonia and was killed before the main experiment. After lavage and before the experiments, the animals were considered normovolemic, as assessed from blood pressure (mean arterial pressure, MAP > 60 mmHg), heart rate (< 120b/min), urine production and base excess within normal range. The three volemic stages were significantly different regarding pressures and flows obtained before the LRMs.
Cardiac output (Table 1)
During the LRMs, there were significant differences in the decrease in cardiac output (CO) between the three volemic stages, with the most pronounced decrease at hypovolemia (Fig. 2). At normovolemia and hypervolemia, CO was more reduced at the end of the 30-s LRM than at the end of the 10-s LRM. At hypovolemia, we could not find any difference in CO between the two LRM durations, probably due to the very low CO. After the 30-s LRM, there was a rebound increase in CO at hypovolemia, peaking 1 min after the LRM and returning to the pre-LRM level at 5 min (Fig. 3). In one animal, CO was also measured in the aortic root. The change in aortic blood flow was similar to the change in pulmonary artery blood flow, but with a small—less than 1 s—delay (Fig. 2).
Continuous registration of the airway pressure (Paw), the aortic blood flow (CO aorta), pulmonary artery flow (CO pulm) and the systemic arterial blood pressure (AP) at hypovolemia, normovolemia, and hypervolemia before, during and after a 30-s lung recruitment maneuver. The tracings above the horizontal line are obtained from the animal in which we measured both the aortic and pulmonary blood flow, while tracings below the line are registered from a separate animal
Echocardiography (Table 1)
Left ventricular diameters as measured at the end of the LRMs did not change with volemic levels or durations. Fractional shortening decreased and was significantly different between the volemic levels at the end of both LRM durations. In the animal in which right ventricle was assessed, it was totally compressed during the LRM at hypovolemia but was adequately filled at hypervolemia (Figs. 4 and 5). End-systolic eccentricity index increased during the LRM at all three volemic levels, indicating increased right ventricular pressure. The videos from the same pig as in Fig. 4 are found in the electronic supplement. They show a significant left ventricular hypokinesia and paradoxic septal motion during the LRM at all three volemic levels, as well as a compression of the right ventricle during hypovolemia.
Schematic outlines of the same echocardiograms as in Fig. 4
Other cardiovascular parameters (Table 1)
Heart rate prior to LRM was similar at all volemic levels and did not change during the LRMs. However, 1 min after the LRMs at hypovolemia, heart rate increased markedly, returning to pre-LRM levels at 5 min. Mean arterial pressure decreased at the end of the LRM and was significantly different between volemic levels at both LRM durations. One minute after the 30-s LRM at hypovolemia and normovolemia, MAP increased temporarily above the pre-LRM level, returning to the pre-LRM level after 5 min. Central venous pressure increased significantly more during the 10-s LRM than during the 30-s LRM at all three volemic levels, and there were significant differences between all volemic levels at the end of the 30-s LRM. Mean pulmonary-artery pressure increased and was significantly different between the volemic levels at the end of both LRM durations.
Lung lavage
End-expiratory lung volume at zero end-expiratory pressure was decreased from 652 ± 145 ml to 306 ± 60 ml (p < 0.005) and PaO2/FiO2 from 65 ± 5 kPa to 15 ± 8 kPa (p < 0.005) by the lung lavage.
Discussion
This study shows that left-ventricular end-diastolic volume was markedly reduced and confirms that cardiac output is briefly, but importantly, compromised during lung recruitment maneuvers in lung-injured pigs. This compromise was accentuated by hypovolemia and attenuated by hypervolemia.
We designed the present study to examine the immediate circulatory effects of lung recruitment maneuvers, i.e., the increase in intrathoracic pressure. We wanted to avoid any remaining effect of a lung volume gain, since we repeated the maneuver after 10 min. Therefore, we used zero end-expiratory pressure during the experiment. It is well known from experiments that lung collapse occurs immediately after the positive pressure is discontinued, and without PEEP there is no sustained effect of a lung recruitment maneuver [19]. Indeed, we found, as intended, no improvement in lung volume or blood gases. In contrast, PaO2 was reduced 1 min after the maneuver, presumably due to a lingering effect of the impaired circulation during the maneuver. At 10 min, however, PaO2 (not shown) had returned to baseline. With the present design, we cannot prove that any actual lung recruitment had occurred during the maneuver. However, since the pressures used were similar to those used in other experimental studies, in which PEEP had been used and a recruitment effect has been shown, it is highly probable that lung recruitment did occur, but, as expected, the lungs de-recruited quickly [23].
Lung recruitment maneuvers have been proposed in ARDS, during anesthesia and after cardiac surgery. They have been found to improve oxygenation in about 70% of the cases [3, 4, 5, 6, 24]. However, lung recruitment maneuvers have not been proven to decrease major morbidity, length of stay in the ICU, ventilator days or mortality. Also, the cardiovascular side effects of these maneuvers have recently been disclosed [6, 16]. Previous clinical studies that concluded that lung recruitment maneuvers affect hemodynamics only minimally were performed in intravascular volume-loaded patients, and only the vascular pressures and not cardiac output or cardiac performance were measured [5, 7, 24, 25]. However, we found, in agreement with other recent experimental studies, that, even under normovolemia, circulation deteriorated during the maneuver [13, 14, 15]. Hypervolemia somewhat attenuated the negative circulatory effect of the lung recruitment maneuver, confirming the results by Odenstedt et al. [14]. More interesting was the profound drop in cardiac output and blood pressure produced by lung recruitment maneuvers at the slight hypovolemia used in this model, where the filling of both right and left ventricles as assessed by echocardiography (Fig. 4 and Fig. 5) was extremely low, and blood flow almost ceased. This finding, as far as we know, has not been reported previously and suggests that the high intrathoracic and transpulmonary pressures compressed both the right atrium and the pulmonary vessels significantly, impeding the filling of the heart and the outflow from the right ventricle. Thus, there are two major explanations for the reduced cardiac output induced by the lung recruitment maneuvers; first, the transmission of the airway pressure to the pleural space, increasing the intrapleural pressure hampering the venous return and the filling of the right ventricle, and second, the lung distension due to the increase in the transpulmonary pressure compressing the small alveolar vessels and increasing the right-ventricular outflow impedance [17, 20, 26, 27]. Upon examination of Figs. 4–7 and the electronically supplemented videos, it is clear that impaired filling was the dominant mechanism during hypovolemia but that, during normovolemia and hypervolemia, increased outflow impedance, as indicated by a right ventricular dysfunction with an increased eccentricity index and paradoxical movement of the septum, was the major cause for reduced cardiac output. However, eccentricity index was also increased during hypovolemia, suggesting that right-ventricular outflow impedance was probably as pronounced in this condition as during hypervolemia. We believe that the significant decrease in fractional shortening during the lung recruitment maneuvers was not due to a decreased contractility. Fractional shortening is very dependent on preload, which, in this study, changed both with volemic levels and with the lung recruitment maneuvers [28].
Schematic outlines of the same echocardiograms as in Fig. 4
The intense rebound of some minutes' duration, with marked increase of blood flow, blood pressure and heart rate immediately after the lung recruitment maneuvers at hypovolemia (but not at the other volemic levels), is also a new finding. This sympathetic stimulation of the circulation was probably due to baroreceptor reflexes induced by the extremely impaired circulation during the lung recruitment maneuver and resembles the well known increase in arterial pressure found in phase IV of the Valsalva maneuver [29]. The latter effect also correlates well with the severity of the maneuver-induced hypotension [30].
This study has several limitations. First, in order to place the flow and the echocardiographic probes, we did a medial thoracotomy and opened the mediastinum and the pericardium. Chest wall was closed after this procedure, but the transmission of airway pressure to the heart and vascular compartment might be different from the native state. Second, it is an animal experiment with its inherent limitations. In particular, the pulmonary circulatory reactivity in response to hypoxia is more pronounced in pigs than in humans [31]. However, the pigs were not hypoxic during the experiment, and after the lung recruitment maneuver, the intravascular pressures and flow recovered quickly, contradicting the possibility that any active vascular response had occurred during the maneuver. Furthermore, the decrease in cardiac output agrees well with the results by Lim and coworkers, studying dogs, which have less inherent pulmonary vascular reactivity than seen in humans [15]. Thus, we believe that the cardiovascular effects found during the lung recruitment maneuvers in this study are primarily, and not secondarily, due to the procedure-induced elevated intrathoracic pressure and lung volumes.
Although one should be careful about transferring findings in animal experiments to the clinical situation, our study suggests that lung recruitment maneuvers should be used with caution in hypovolemia, and particularly in hypovolemic patients with a heart condition, who may not tolerate the increase in heart work after a lung recruitment maneuver.
Conclusions
Our experimental study shows that lung recruitment maneuvers, using short or longer sustained inflation, significantly hamper cardiac output and filling of the left heart. This effect was exaggerated during hypovolemia and attenuated during hypervolemia. In addition, lung recruitment maneuvers induced right ventricular dysfunction.
References
Bernard GR, Artigas A, Brigham KL, Carlet J, Falke K, Hudson L, Lamy M, LeGall JR, Morris A, Spragg R (1994) Report of the American-European consensus conference on ARDS: definitions, mechanisms, relevant outcomes and clinical trial coordination. The Consensus Committee. Intensive Care Med 20:225–232
Sachdeva SP (1974) Treatment of post-operative pulmonary atelectasis by active inflation of the atelectatic lobe(s) through an endobronchial tube. Acta Anaesthesiol Scand 18:65–70
Rothen HU, Sporre B, Engberg G, Wegenius G, Hedenstierna G (1993) Re-expansion of atelectasis during general anaesthesia: a computed tomography study. Br J Anaesth 71:788–795
Magnusson L, Wicky S, Tyden H, Hedenstierna G (1998) Repeated vital capacity manoeuvres after cardiopulmonary bypass: effects on lung function in a pig model. Br J Anaesth 80:682–684
Dyhr T, Laursen N, Larsson A (2002) Effects of lung recruitment maneuver and positive end-expiratory pressure on lung volume, respiratory mechanics and alveolar gas mixing in patients ventilated after cardiac surgery. Acta Anaesthesiol Scand 46:717–725
Grasso S, Mascia L, Del Turco M, Malacarne P, Giunta F, Brochard L, Slutsky AS, Marco Ranieri V (2002) Effects of recruiting maneuvers in patients with acute respiratory distress syndrome ventilated with protective ventilatory strategy. Anesthesiology 9:795–802
Claxton BA, Morgan P, McKeague H, Mulpur A, Berridge J (2003) Alveolar recruitment strategy improves arterial oxygenation after cardiopulmonary bypass. Anaesthesia 58:111–116
Jardin F, Vieillard-Baron A (2003) Right ventricular function and positive pressure ventilation in clinical practice: from hemodynamic subsets to respirator settings. Intensive Care Med 29:1426–1434
Pinsky MR (1997) The hemodynamic consequences of mechanical ventilation: an evolving story. Intensive Care Med 23:493–503
Permutt S, Bromberger-Barnea B, Bane HN (1962) Alveolar pressure, pulmonary venous pressure, and the vascular waterfall. Med Thorac 19:239–260
Bein T, Kuhr LP, Bele S, Ploner F, Keyl C, Taeger K (2002) Lung recruitment maneuver in patients with cerebral injury: effects on intracranial pressure and cerebral metabolism. Intensive Care Med 28:554–558
Claesson J, Lehtipalo S, Winso O (2003) Do lung recruitment maneuvers decrease gastric mucosal perfusion? Intensive Care Med 29:1314–1321
Nunes S, Rothen HU, Brander L, Takala J, Jakob SM (2004) Changes in splanchnic circulation during an alveolar recruitment maneuver in healthy porcine lungs. Anesth Analg 98:1432–1438
Odenstedt H, Aneman A, Karason S, Stenqvist O, Lundin S (2005) Acute hemodynamic changes during lung recruitment in lavage and endotoxin-induced ALI. Intensive Care Med 31:112–120
Lim SC, Adams AB, Simonson DA, Dries DJ, Broccard AF, Hotchkiss JR, Marini JJ (2004) Transient hemodynamic effects of recruitment maneuvers in three experimental models of acute lung injury. Crit Care Med 32:2378–2384
Fujino Y, Goddon S, Dolhnikoff M, Hess D, Amato MB, Kacmarek RM (2001) Repetitive high-pressure recruitment maneuvers required to maximally recruit lung in a sheep model of acute respiratory distress syndrome. Crit Care Med 29:1579–1586
Nielsen J, Ostergaard M, Kjaergaard J, Tingleff J, Berthelsen PG, Nygard E, Larsson A (2005) Lung recruitment maneuver depresses central hemodynamics in patients following cardiac surgery. Intensive Care Med 31(9):1189–1194
Nielsen J, Nilsson M, Freden F, Alstrom U, Hultman J, Larsson A (2005) Lung recruitment maneuvers seriously affect central hemodynamics during hypovolemia. Crit Care Med 32 (12) [Suppl]:A120
Neumann P, Berglund JE, Mondejar EF, Magnusson A, Hedenstierna G (1998) Dynamics of lung collapse and recruitment during prolonged breathing in porcine lung injury. J Appl Physiol 85:1533–1543
Ryan T, Petrovic O, Dillon JC, Feigenbaum H, Conley MJ, Armstrong WF (1985) An echocardiographic index for separation of right ventricular volume and pressure overload. J Am Coll Cardiol 5:918–927
Larsson A, Linnarsson D, Jonmarker C, Jonson B, Larsson H, Werner O (1987) Measurement of lung volume by sulfur hexafluoride washout during spontaneous and controlled ventilation: further development of a method. Anesthesiology 67:543–550
von Englehardt W (1966) Swine cardiovascular physiology: A review. In: Bustad LK, Mclellan RO (eds) Swine in biomedical research. Frayn, Seattle, pp 307–329
Lim SC, Adams AB, Simonson DA, Dries DJ, Broccard AF, Hotchkiss JR, Marini JJ (2004) Intercomparison of recruitment-maneuver efficacy in three models of acute lung injury. Crit Care Med 32:2371–2377
Lapinsky SE, Aubin M, Mehta S, Boiteau P, Slutsky AS (1999) Safety and efficacy of a sustained inflation for alveolar recruitment in adults with respiratory failure. Intensive Care Med 25:1297–1301
Dyhr T, Bonde J, Larsson A (2003) Lung recruitment manoeuvres are effective in regaining lung volume and oxygenation after open endotracheal suctioning in acute respiratory distress syndrome. Crit Care 7:55–62
Vieillard-Baron A, Loubieres Y, Schmitt JM, Page B, Dubourg O, Jardin F (1999) Cyclic changes in right ventricular output impedance during mechanical ventilation. J Appl Physiol 87:1644–1650
Jardin F, Farcot JC, Boisante L, Curien N, Margairaz A, Bourdarias JP (1981) Influence of positive end-expiratory pressure on left ventricular performance. N Engl J Med 304:387–392
Cheung AT, Savino JS, Weiss SJ, Aukburg SJ, Berlin JA (1994) Echocardiographic and hemodynamic indexes of left ventricular preload in patients with normal and abnormal ventricular function. Anesthesiology 81:376–387
Nishimura RA, Tajik AJ (1986) The Valsalva maneuver and response revisited. Mayo Clin Proc 61:211–217
Sharpey-Schafer EP (1955) Effects of Valsalva's manoeuvre on the normal and failing circulation. Br Med J 4915:693–695
Maggiorini M, Brimioulle S, De Canniere D, Delcroix M, Naeije R (1998) Effects of pulmonary embolism on pulmonary vascular impedance in dogs and minipigs. J Appl Physiol 84:815--821
Acknowledgements
This work was done at the Department of Clinical Physiology at Uppsala University Hospital. The authors wish to thank Agneta Ronéus and Karin Fagerbrink for their excellent assistance in the animal laboratory. The study was supported partly by: The Danish Medical Research Council (Nos. 22-03-0299, 22-04-0420) and the Danish Heart Foundation (No. 04-10-B152-A230-22194).
Author information
Authors and Affiliations
Corresponding author
Additional information
An erratum to this article can be found at http://dx.doi.org/10.1007/s00134-006-0176-8
Rights and permissions
About this article
Cite this article
Nielsen, J., Nilsson, M., Fredén, F. et al. Central hemodynamics during lung recruitment maneuvers at hypovolemia, normovolemia and hypervolemia. A study by echocardiography and continuous pulmonary artery flow measurements in lung-injured pigs. Intensive Care Med 32, 585–594 (2006). https://doi.org/10.1007/s00134-006-0082-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-006-0082-0