Abstract
Objective: The aim of the study was to explore trends and changes in sedation practices for mechanically ventilated patients in Danish intensive care units (ICUs) and to compare sedation practices in 1997 and 2003.
Design: The study was a follow-up survey with a descriptive and comparative cross-sectional multicenter design.
Setting: Questionnaires were mailed in January 2003 to all Danish ICUs providing mechanical ventilation (n=48).
Participants: One head physician at each ICU in Denmark.
Interventions, measurements, and results: Thirty-nine questionnaires were returned, yielding a response rate of 81%, representing 82% of Danish ICU beds. The main findings were a significant increase in the use of sedation scoring systems and a significant reduction of sedation and analgesia in relation to various modalities of mechanical ventilation and disease groups. Other important findings were a significant reduction in the use of benzodiazepines and opioids and a significant increase in the use of propofol in relation to all ventilator modes. The administration routes of sedative agents remained unchanged.
Conclusions: Sedatives and analgesics are still widely used in Danish ICUs. The trend is toward lighter sedation along with a shift from benzodiazepines toward propofol and from morphine toward fentanyl given by continuous infusion. More attention needs to be directed toward sedation standards and scoring systems in order to reduce the risk associated with sedation in mechanically ventilated patients.
Similar content being viewed by others
Introduction
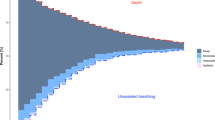
Sedation and analgesia are commonly used for mechanically ventilated patients in the intensive care unit (ICU) in order to provide relief from anxiety and pain. Inadequate as well as excessive sedation may be harmful to the patient. Although suboptimal sedation may potentially increase morbidity, mortality, and cost, the quest for more efficient sedation regimens has not always been considered a clinical priority. Sedation and analgesia are important from both physical and psychological points of view. Newer drugs, newer ventilation and sedation strategies, and newer sedation scoring systems are continually being developed, making it possible to adjust sedation more accurately [1–4]. What constitutes the ideal level of sedation is still controversial, but studies are recommending a shift from deep to lighter sedation, including adjustments during special therapy and diagnostic procedures and in relation to circadian rhythms [5]. National surveys and systematic reviews have assessed the use of sedatives and analgesics and have provided recommendations for optimizing sedation of the intubated patient [6–11]. A national survey of sedation practices in Denmark was conducted in 1997 [12]. The aim of the present study was to explore trends and changes in sedation practices for mechanically ventilated patients in Danish ICUs and to compare sedation practices in 1997 and 2003.
Materials and methods
The study had a descriptive and comparative cross-sectional multicenter design and was a follow-up study to a survey conducted in 1997 [12]. A list of Danish hospitals with at least one consultant anesthesiologist was compiled from the 2002 edition of the Directory of Danish Hospitals. Questionnaires were mailed in January 2003 to the head physician and the head nurse at each ICU, assuming that these persons would provide representative responses regarding sedation practices at that unit. Reminders were mailed after 4 weeks. This article compares physicians’ responses in 1997 (n=49) and 2003 (n=39), while a separate article addresses variations in physicians’ and nurses’ responses in 2003 [13]. The total number of Danish ICUs has been reduced from 53 in 1997 to 48 in 2003 because of hospital mergers during the past 6 years.
The instrument
The questionnaire was a modified version of the instrument used by Christensen and Thunedborg in 1997 [12], which was inspired by Hansen-Flaschen et al. [14]. Because the questionnaire had been tested previously and this was a follow-up study, the present instrument was not retested. The present instrument did not include questions on neuromuscular blocking agents (NMBAs) because their use has been reduced in Denmark due to more sophisticated modalities of mechanical ventilation and the trend toward lighter sedation. Concurrently a recent European study of sedative and analgesic practice chose not to include the use of NMBAs [7]. It should be added at this point that “sedation” is a broad term often used to encompass sedative as well as analgesic treatment in the ICU. Unless specifically stated in this article, “sedation” will be used in its broadest meaning.
The survey included the following parts:
Part 1. Demographic data
Appointment level, years of ICU experience, type of hospital and unit, number of beds, and types of clinical specialties.
Part 2. Formal sedation practice and collaboration
Implementation of written protocols for sedation and sedation withdrawal, subjective scoring system (such as the Ramsay Sedation Scale), objective scoring system (such as the Bispectral Index), frequency of assessment, routine daily interruption of sedation, and management of circadian rhythm.
Part 3. Indication for sedation
Choice of sedation related to type and degree of organ failure and expected duration of treatment.
Part 4. Frequency of sedation and analgesia related to modalities of mechanical ventilation
Use of sedatives and analgesics related to pressure-regulated ventilation (pressure control), volume-regulated ventilation (volume control), and patient-regulated ventilation (pressure support or continuous positive airway pressure).
Part 5. Frequency of sedation and analgesia related to disease
Use of sedatives and analgesics related to acute respiratory distress syndrome (ARDS), chronic obstructive pulmonary disease (COPD), heart failure, and head trauma.
Part 6. Frequency of medications related to modalities of mechanical ventilation
Frequency of use of different groups of sedatives and analgesics related to pressure-regulated ventilation, volume-regulated ventilation, and patient-regulated ventilation.
Part 7. Routes of administration of medications
Use of midazolam, diazepam, propofol, morphine, ketamine, fentanyl, alfentanil, and sufentanil related to continuous and intermittent administration.
Part 8. Frequency of side effects related to sedation
Use of sedatives and analgesics related to delayed awakening, paradoxical agitation, respiratory depression, and gastrointestinal disturbances.
The study protocol and instruments were reviewed and approved by the ICU department head at the anesthesia department at the Copenhagen University Hospital in Glostrup. Consent to participate was implied by the return of the completed questionnaires.
Statistics
The responses to the questionnaire’s parts 2, 3, and 7 were given as “yes” or “no.” The responses to parts 4, 5, 6, and 8 were given on a 4-point scale with scores ranging from 1 to 4, where 1= never, 2= occasionally (<20% of patients), 3= frequently (20–70% of patients), and 4= routinely (>70% of patients) [12–14]. The data were entered into an Excel spreadsheet and analyzed using the Statistical Package for the Social Sciences (SPSS) version 13.0. All data were triple-checked by the authors. The statistical significance was calculated using the chi-square test, and the cut-off level was p<0.05.
Results
Thirty-nine out of 48 questionnaires were answered and returned, yielding a response rate of 81%, with a rate of 84% at university hospitals and 79% at county and local hospitals. The nonresponders were distributed evenly across the country, representing units of varying sizes. The answers represented 281 (82%) of 344 ICU beds; the mean number of beds was 7.2 (range 2–16). Among the respondents, 80% of the physicians had more than 5 years of ICU experience. Eighty-seven percent were head physicians (managers and specialists), and 10% were ward physicians (specialists); one did not disclose his or her appointment level. Among the participating ICUs, 35 (90%) were general medical-surgical units, two were thoracic-surgical units, and two were neurosurgical units.
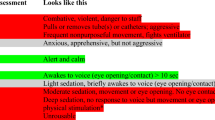
Table 1 shows that there was no significant variation in the use of sedation protocols, use of weaning protocols, or management of circadian rhythm in 1997 and 2003. The use of subjective scoring systems for sedation assessment, however, increased significantly during that period. The preferred scoring system was the Ramsay Sedation Scale [15]. Other scoring systems included Cook and Palma (COOK) [16], the Motor Activity Assessment Scale (MAAS) [17], and the Sedation-Agitation Scale (SAS) [18]. The respondents did not answer how frequently the patients’ sedation level was assessed. Objective scoring systems for evaluation of sedation were reported at only two of the 39 ICUs, while 12 (31%) respondents stated that daily interruption of sedation, a “wake-up call,” was practiced routinely. Symptoms of withdrawal were treated with phenobarbital in 24 (62%) of the departments and with clonidine in 11 (28%).
Table 2 shows a trend toward lighter sedation in 2003 that was related to pressure-regulated and volume-regulated ventilation, as the proportion of patients who were sedated routinely decreased significantly. It remains that some patients were sedated during patient-regulated ventilation. According to the physicians in 2003, the choice of medications was influenced by the type and degree of organ failure as well as the expected duration of treatment.
Table 3 shows the frequency of use of sedation and analgesia in relation to different diagnostic indications for ventilatory treatment. The sedation strategy was unchanged for patients with ARDS, whereas patients with COPD, heart failure, and head trauma were sedated significantly less frequently in 2003.
In Table 4 the frequency of the use of different groups of sedatives and analgesics is presented in relation to different modalities of mechanical ventilation. The table shows a significant reduction in the use of benzodiazepines and opioids and a significant increase in the use of propofol in all ventilator modes in 2003.
Table 5 shows the administration routes of sedatives and analgesics. The data demonstrate that the administration of sedative medications was unchanged from 1997 to 2003. Regarding the choice of agent, the data suggest a reduction in the use of midazolam, diazepam, and morphine as continuous infusions and an increase in the use of propofol and fentanyl.
Finally, Table 6 shows the estimated frequency of side effects related to the use of sedatives and analgesics. The frequency of delayed emergence related to sedatives and analgesics was unchanged in 2003. Paradoxical agitation and respiratory depression related to sedatives were significantly reduced in 2003, whereas respiratory depression and gastrointestinal disorders related to analgesics were unchanged in 2003.
Discussion
The present study was conducted to explore the trends and changes in sedation practices for mechanically ventilated patients in Danish ICUs in 1997 and 2003. In accordance with international recommendations, a trend toward lighter sedation was seen. The main findings were a significant increase in the use of sedation scoring systems and a significant reduction of sedation and analgesia in relation to various disease groups and modalities of mechanical ventilation. Other important findings were a significant reduction in the use of benzodiazepines and opioids, as well as an increase in the use of propofol in relation to all ventilator modes. There was a significant shift from benzodiazepines to propofol as the preferred sedative, and no change regarding the administration routes of medications.
The number of ICUs using subjective sedation scoring systems increased significantly, and many departments reported using the Ramsay Sedation Scale [15]. Although the Ramsay Sedation Scale is the most frequently used instrument in Denmark, it still needs more rigorous validation [19, 20]. The most common sedation scale in other European countries is the Motor Activity Assessment Scale (MAAS) [7], which has been subject to validation but may appear to be more complex [17].
It may have been more difficult to implement sedation protocols than sedation scoring systems in Danish ICUs because the protocols were developed locally, whereas the scoring systems are international. The actual benefit of using a sedation scoring system is unclear in this study, as the participating physicians were unable to provide information regarding the frequency of assessment of sedation level. The reason may be that nurses decide the timing of the assessment [13], but the lack of systematic assessment may prevent optimal titration of medications in relation to patient response and expected outcome.
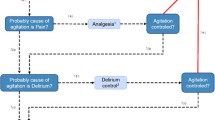
The present study shows a significant reduction in the use of sedatives as well as analgesics in patients with COPD, heart failure, and head trauma. The reduction of analgesics runs counter to the treatment policy of analgosedation, in which analgesia is the first step in the sedation protocol and sedative drugs are considered only after pain has been excluded [21]. Because patients were treated significantly less frequently for pain, it may be inferred that the use of analgesia was either excessive in 1997 or insufficient in 2003. There is a need for more accurate assessment and treatment of pain in ventilated patients.
Newer studies stress that the choice of medication may be less important than the route of administration [4, 9, 22]. The present study shows no significant changes in preferred routes of medication administration over the past 6 years. Some argue that continuous infusions are preferable because peaks and troughs are avoided, whereas others state that intermittent boluses are easier to control and prevent medications from getting out of hand. The controversy that still exists on this subject may explain adherence to earlier practice. More research is needed to determine the optimal route of administration for sedative agents.
Variations exist regarding the use of sedatives and analgesics across national boundaries despite the ongoing development of standards and guidelines [8, 23–25]. The variations may be explained by the timing of drug registration, the primary specialty of the physician, economic considerations, staffing, personal preferences of the ICU staff, and the use of different modalities of verbal and nonverbal communication, such as the staff’s use of touch, the presence of relatives, or the presence of background music [26].
The quest for optimal sedation is still hampered by the bipolar issues of oversedation and undersedation, as demonstrated in other studies [10, 22]. The estimated frequency of side effects described as paradoxical agitation and respiratory depression related to the use of sedative drugs were significantly reduced in 2003. Perhaps this finding is associated with a shift from midazolam to propofol and a trend toward lighter sedation. Other studies are exploring the side effects related to various sedative agents, such as the frequency, characteristics, and outcomes of severe agitation (as measured on the Motor Activity Assessment Scale), which are associated with adverse events and longer ICU stays [27].
The inherent limitation of studies using questionnaires is that they rely on the perceptions and recall of the respondents rather than providing an accurate account of actual events. Although the numbers are small, the validity of this study has been increased by using a comprehensive multicenter design with equal representation at each ICU in the country, where each informant was assumed to provide a reliable estimate of standard practice. The survey conducted in 2003 had a lower response rate than the study in 1997, but it still had a significantly higher response rate than other comparable national surveys. Although the questionnaire could have been improved in 2003, the original format was chosen for purposes of comparison.
Sedation practices vary nationally and internationally. Sedatives and analgesics are still widely used for patients requiring mechanical ventilation in Danish ICUs. The trend is moving toward lighter sedation with a combination of propofol and fentanyl given by continuous infusion, replacing midazolam and morphine as the preferred agents. More homogeneous practice policies may improve treatment and facilitate research. Protocols and scoring systems that improve the quality of sedation and reduce the risk of long-term effects need further development. While more attention needs to be directed toward treatment of pain and prevention of long-term effects of sedation, future research should include the patients’ perspectives and preferences in relation to sedation.
References
Kress JP, Pohlman AS, O’Connor MF, Hall JB (2000) Daily interruption of sedative infusions in critically ill patients undergoing mechanical ventilation. N Engl J Med 342:1471–1477
Ely EW, Truman B, Shintani A, Thomason JW, Wheeler AP, Gordon S, Francis J, Speroff T, Gautam S, Margolin R, Sessler CN, Dittus RS, Bernard GR (2003) Monitoring sedation status over time in ICU patients: reliability and validity of the Richmond Agitation-Sedation Scale (RASS). JAMA 289:2983–2991
Brattebo G, Hofoss D, Flaatten H, Muri AK, Gjerde S, Plsek PE (2002) Effect of a scoring system and protocol for sedation on duration of patients’ need for ventilator support in a surgical intensive care unit. Br Med J 324:1386–1389
Kollef MH, Levy NT, Ahrens TS, Schaiff R, Prentice D, Sherman G (1998) The use of continuous i.v. sedation is associated with prolongation of mechanical ventilation. Chest 114:541–548
Lerch C, Park GR (1999) Sedation and analgesia. Br Med Bull 55:76–95
Rhoney DH, Murry KR (2002) National survey on the use of sedatives and neuromuscular blocking agents in the pediatric intensive care unit. Pediatr Crit Care Med 3:129–133
Soliman HM, Mélot C, Vincent J-L (2001) Sedative and analgesic practice in the intensive care unit: the results of a European survey. Br J Anaesth 87:186–192
Nasraway SA, Jacobi J, Murray MJ, Lumb PD (2002) Sedation, analgesia, and neuromuscular blockade of the critically ill adult: revised clinical practice guidelines for 2002. Crit Care Med 30:117–118
Izurieta R, Rabatin JT (2002) Sedation during mechanical ventilation: a systematic review. Crit Care Med 30:2644–2648
Ostermann ME, Keenan SP, Seiferling RA, Sibbald WJ (2000) Sedation in the intensive care unit: a systematic review. JAMA 283:1451–1459
Guldbrand P, Berggren L, Brattebo G, Ronholm E, Winso E (2004) Survey of routines for sedation of patients on controlled ventilation in Nordic intensive care units. Acta Anaesthesiol Scand 48:944–950
Christensen BV, Thunedborg LP (1999) Use of sedatives, analgesics and neuromuscular blocking agents in Danish ICUs 1996/97: a national survey. Intensive Care Med 25:186–191
Egerod I, Christensen BV, Johansen L (2005) Nurses’ and physicians’ sedation practices in Danish ICUs in 2003. A national survey. Intensive Crit Care Nurs [28 May; Epub head of print]
Hansen-Flaschen JH, Brazinsky S, Basile C, Lanken PN (1991) Use of sedating drugs and neuromuscular blocking agents in patients requiring mechanical ventilation for respiratory failure: a national survey. JAMA 266:2870–2875
Ramsay MA, Savege TM, Simpson BR, Goodwin R (1974) Controlled sedation with alphaxalone-alphadolone. Br Med J 2(920):656–659
Cook S, Palma O (1989) Propofol as a sole agent for prolonged infusion in intensive care. J Drug Dev 4(suppl 2):65–67
Devlin JW, Boleski G, Mlynarek M, Nerenz DR, Peterson E, Jankowski M, Horst HM, Zarowitz BJ (1999) Motor Activity Assessment Scale: a valid and reliable sedation scale for use with mechanically ventilated patients in an adult surgical intensive care unit. Crit Care Med 27:1271–1275
Simmons LE, Riker RR, Prato BS, Fraser GL (1999) Assessing sedation during intensive care unit mechanical ventilation with the Bispectral Index and Sedation-Agitation Scale. Crit Care Med 27:1499–1504
De Jonghe B, Cook D, Appere-De-Vecchi C, Guyatt G, Meade M, Outin H (2000) Using and understanding sedation scoring systems: a systematic review. Intensive Care Med 26:275–285
Hansen-Flaschen JH, Cowen J, Polomano RC (1994) Beyond the Ramsay scale: need for a validated measure of sedating drug efficacy in the intensive care unit. Crit Care Med 22:732–733
Walder B, Tramèr MR (2004) Analgesia and sedation in critically ill patients. Swiss Med Wkly 134:333–346
de Wit M, Epstein SK (2003) Administration of sedatives and level of sedation: comparative evaluation via the Sedation-Agitation Scale and the Bispectral Index. Am J Crit Care 12:343–348
Jacobi J, Fraser GL, Coursin DB, Riker RR, Fontaine D, Wittbrodt ET, Chalfin DB, Masica MF, Bjerke HS, Coplin WM, Crippen DW, Fuchs BD, Kelleher RM, Marik PE, Nasraway SA Jr, Murray MJ, Peruzzi WT, Lumb PD; Task Force of the American College of Critical Care Medicine (ACCM) of the Society of Critical Care Medicine (SCCM), American Society of Health-System Pharmacists (ASHP), American College of Chest Physicians (2002) Clinical practice guidelines for the sustained use of sedatives and analgesics in the critically ill adult. Crit Care Med 30:119–141
MacLaren R, Plamondon JM, Ramsay KB, Rocker GM, Patrick WD, Hall RI (2000) A prospective evaluation of empiric versus protocol-based sedation and analgesia. Pharmacotherapy 20:662–672
Shapiro BA, Warren J, Egol AB, Greenbaum DM, Jacobi J, Nasraway SA, Schein RM, Spevetz A, Stone JR (1995) Practice parameters for intravenous analgesia and sedation for adult patients in the intensive care unit: an executive summary. Crit Care Med 23:1596–1600
Vincent JL (1997) Communication in the ICU. Intensive Care Med 23:1093–1098
Woods JC, Mion LC, Connor JT, Viray F, Jahan L, Huber C, McHugh R, Gonzales JP, Stoller JK, Arroliga AC (2004) Severe agitation among ventilated medical intensive care unit patients: frequency, characteristics and outcomes. Intensive Care Med 30:1066–1072
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Egerod, I., Christensen, B.V. & Johansen, L. Trends in sedation practices in Danish intensive care units in 2003: a national survey. Intensive Care Med 32, 60–66 (2006). https://doi.org/10.1007/s00134-005-2856-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-005-2856-1