Abstract
Objective: To evaluate the effects of early short-term, isovolaemic haemofiltration at 45 ml/kg/h on physiological and clinical outcomes in patients with septic shock. Design: Retrospective study before and after a change of unit protocol (study period 8 years). Setting: Intensive care unit of metropolitan hospital. Patients: Eighty patients with septic shock. Interventions: Introduction of a new septic shock protocol based on early isovolaemic haemofiltration (EIHF). In the pre-EIHF period (before), 40 patients received conventional supportive therapy. In the post-EIHF period (after), 40 patients received EIHF at 45 ml/kg/h of plasma-water exchange over 6 h followed by conventional continuous venovenous haemofiltration (CVVH). Anticoagulation policy remained unchanged. Measurements and main results: The two groups were comparable for age, gender and baseline APACHE II score. Delivered haemofiltration dose was above 85% of prescription in all patients. PaO2/FiO2 ratio increased from 117±59 to 240±50 in EIHF, while it changed from 125±55 to 160±50 in the control group ( p <0.05). In EIHF patients, mean arterial pressure increased (95±10 vs 60±12 mmHg; p <0.05), and norepinephrine dose decreased (0.20±2 vs 0.02±0.2 µg/kg/min; p <0.05). Among EIHF patients, 28 (70%) were successfully weaned from the ventilator compared with 15 (37%) in the control group ( p <0.01). Similarly, 28-day survival was 55% compared with 27.5% ( p <0.05). Length of stay in the ICU was 9±5 days compared with 16±4 days ( p <0.002). Conclusions: In patients with septic shock, EIHF was associated with improved gas exchange, haemodynamics, greater likelihood of successful weaning and greater 28-day survival compared with conventional therapy.
Similar content being viewed by others
Introduction
Multiple organ dysfunction syndrome (MODS) [1] is the most frequent cause of death in patients admitted to intensive care units with severe sepsis. Its mortality exceeds 50% despite full organ support [2, 3, 4,5]. Treatment of the underlying cause, drainage of the septic focus, antibiotics, maintenance of organ perfusion and restoration of homeostasis represent conventional practice. More recently, activated protein C has been shown to improve mortality in some of these patients [6].
Beyond the presence of severe vasodilation requiring vasopressor support, the two most common organs affected by MODS are lung and kidney [7]. Both organs might develop injury and dysfunction because of the systemic effect of a variety of immunomodulating substances (humoral mediators) released into the circulation during severe infection [8,9]. If this paradigm is correct, treatment with techniques such as high volume haemofiltration (HVHF) that can non-selectively affect a wide range of such modulators might prove beneficial if applied early and at an appropriate level of intensity.
Recent studies have provided support for this conceptual framework [10,11]. However, such studies have either been uncontrolled, have focussed on short-term physiological gains and have not formally considered the effect of such therapy on lung function.
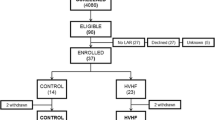
We hypothesized that early isovolaemic haemofiltration (EIHF) at 45 ml/kg/h of plasma-water exchange over 6 h might be beneficial in ICU patients with septic shock, lung injury and acute renal failure (MODS) and compared 40 patients (control group) who received conventional treatment to 40 similar patients (intervention group) who received EIHF after a change of unit protocol.
Patients and methods
The hospital ethics committee approved the study, and informed consent was obtained from the next of kin from the time when the new protocol was implemented (early 1999).
Design: this was a single-centre retrospective study of treatment conducted over an 8-year period (January 1996 to January 2004). Patients were included if they met the necessary inclusion criteria.
Inclusion criteria for all patients included the presence of septic shock defined by:
-
1.
At least two criteria for SIRS
-
2.
A clinically identified focus of infection
-
3.
A high cardiac output and low systemic vascular resistance state
-
4.
The exclusion of other conditions potentially responsible for shock such as hypovolaemia, acute heart failure, anaphylaxis or pulmonary embolus
-
5.
Acute renal injury (ARI) [15] with oliguria, despite fluid resuscitation and furosemide administration in the previous 24 h
-
6.
Acute lung injury (ALI) [12] with a lung injury score >2.5
Exclusion criteria were:
-
1.
Established acute renal failure [15]
-
2.
Previous history of pulmonary disease (FEV1 <30% predicted)
-
3.
Severe cardiac disease (NYHA classes III and IV)
-
4.
Advanced stage IV malignancy
-
5.
Advanced AIDS with pulmonary infection
-
6.
Expected death within the next 24 h
-
7.
Lack of commitment to full and prolonged organ support
-
8.
Admission following cardiac arrest with no evidence of neurological recovery
-
9.
Pregnancy
-
10.
Lactation
-
11.
Age <16 years
-
12.
Randomisation or inclusion in an interventional trial
General principles of patient care
A source of infection was actively sought in all patients and treated appropriately. Broad-spectrum antibiotic therapy was started early and adjusted as microbiological data became available and microbiological patient care was discussed daily with infectious-disease consultants.
For all patients, clinical data including the primary diagnosis, type of surgical procedure and the presence and degree of organ dysfunction was assessed by the sequential organ failure assessment (SOFA) score [13]. Shock was treated using a standard existing protocol for haemodynamic management with initial optimisation of volume under the guidance of central venous pressure (CVP). Fluid balance was calculated by subtracting urinary volume, gastric residual volumes, and fluid loss from drains from the total volume of fluids infused (colloids, crystalloids and dextrose). A minimum mean arterial pressure (MAP) of 65–75 mmHg was pursued. When MAP was lower, the adequacy of fluid resuscitation was reassessed by means of central venous pressure or pulmonary artery occlusion pressure (PAOP) measurements and corrected by crystalloid or colloid infusions and/or the initiation of vasopressor therapy. The goal of fluid resuscitation was of maintaining a CVP>10 cmH2O or a PAOP >12 mmHg. If these goals were achieved but the cardiac index remained low (<2.5 l/min/m2), further fluid boluses were given and cardiac output re-measured to diagnose a persistent fluid-responsive relative low cardiac output state. Anaemia was corrected to a Hb>10 g/dl. Therapy with vasoactive medication (dopamine was used as the initial vasopressor followed by norepinephrine) was initiated when the MAP remained <65 mmHg or the cardiac index remained relatively low despite optimised fluid loading. A pulmonary artery catheter was positioned in all patients requiring vasoactive support. We started with dopamine, which was titrated between 3 µg/kg/min and 20 µg/kg/min. Norepinephrine, which was titrated from 0.2–2 µmcg/kg/min, was added if the patient remained hypotensive despite dopamine at a dose of 20 µg/kg/min. Dobutamine was added whenever the cardiac index of>2.5 l/min/m2 was not achieved. Epinephrine was added if a mean arterial pressure of >65 mmHg and cardiac index of >2.5 l/min/m2 were not achieved and titrated from 0.1–1 µg/kg/min.
Ventilatory management in all patients followed a protective-ventilation strategy of maintaining low inspiratory driving pressures (<20 cm of water above PEEP with low tidal volumes <7–8 ml/kg) and preferential use of limited airway pressure over regulation of arterial carbon dioxide levels.
Parenteral nutritional support was by a standard solution of amino acids, 50% fat and 50% glucose, vitamins, electrolytes and trace elements when enteral nutrition was not possible or was contraindicated.
Approach to haemofiltration in two study groups
Prior to the introduction of the Early Isovolaemic Haemofiltration (EIHF) protocol in sepsis, patients received extracorporeal support only for conventional indications (see above). In fact, haemofiltration was only initiated if patients fulfilled classic criteria for renal replacement therapy reported in the literature [14,15].
After the introduction of the EIHF protocol, 40 patients were treated by early Isovolaemic haemofiltration within 12 h of admission to ICU. A double lumen catheter was inserted in the femoral, and sometimes internal jugular, vein and therapy was started utilizing the EQUAsmart continuous renal replacement therapy (CRRT) machine (Medica, Mirandola, Italy), the Aquarius machine (Edwards Lifesciences, Irvine, CA, USA) and Multifiltrate Machine (Fresenius Medical Care, Bad Homburg, Germany). Heparin (infused pre-filter) was used in those patients requiring anticoagulation. Some patients did not receive anticoagulation (12 in the control and 13 in the intervention group). According to our unit policy, low-risk patients were treated with the standard protocol of low-dose pre-filter heparin infusion at a dose of 5 IU/kg/h. In those patients considered at high risk, as determined by abnormal coagulation tests, the amount of heparin was reduced or heparin was withdrawn. Our practice pattern concerning anticoagulation did not change throughout the study period. Filters and circuit were changed every 24 h. Replacement fluids containing bicarbonate (32 mmol/l) as buffer were infused in predilution mode to maintain fluid balance. Blood flow ranged from 150–250 ml/min. The prescribed dose was 45 ml/kg/h of plasma water exchange over 6 h with neutral fluid balance followed by conventional continuous venovenous haemofiltration (CVVH). A 0.8 m2 polysulfone haemofilter (Medisulfone, Medica, Mirandola, Italy) was used in all patients after rinsing and priming with heparinised saline solution (5,000 IU/l). The filter was changed every 24 h according to unit policy, and solute transport was achieved by pure convection. Treatment was repeated from a minimum of 3 days and up to a maximum of 9 days with an average of 5 days. RRT support was otherwise continued in isovolaemic mode also in the other remaining 18 h at conventional (20 ml/kg/h) CVVH rates thereafter. In the 40 control patients, the treatment dose (20 ml/kg/h) was chosen based on the average dose delivered in routine clinical practice, and replacement fluid was delivered via a volumetric intravenous infusion pump at a controlled rate at the same mode. Since convective clearance in predilution mode is reduced by a fraction corresponding to the percentage dilution occurring in the pre-filter line, we programmed an ultrafiltration rate 20% higher than the prescribed clearance, in order to account for the relative reduction induced by predilution and to achieve the desired treatment dose. The prescribed dose was 45 ml/kg/h of plasma water exchange over 6 h (actual delivery was 55 ml/kg/h of UF rate to compensate for the effect of predilution on solute clearance).
Severity of disease at admission was estimated by the APACHE (Acute Physiology and Chronic Health Evaluation) II score [16]. The primary end point was improvement of pulmonary function defined by the PaO2/FiO2 ratio 48 h after treatment. Secondary end points were:
-
1.
Successful weaning from mechanical ventilation defined by extubation and ventilator independence for at least >24 h
-
2.
Recovery of renal function defined by restoration of diuresis (>800 ml/24 h) [15]
-
3.
Duration of ICU stay
-
4.
Duration of hospital stay
-
5.
Survival at 28 days
Statistical analysis
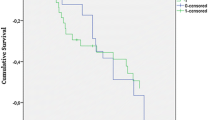
The data are expressed as means ± standard deviation (SD). Comparisons of nominal variables were by means of Fisher’s exact test and of numerical variables by the Mann–Whitney test. Survival data were compared using the Kaplan-Meier estimate and the Mantel-Cox log rank test. Significance was accepted for a two-sided p value of <0.05. The SPSS 11.0.1 (SPSS, Chicago, IL) statistical software package was used.
Results
The diagnostic and clinical characteristics of the study patients are presented in T.S1 (available as Electronic Supplementary Material) and Table 1. Gender distribution was similar (31 males in the EIHF group compared with 29 in the control group). The two groups were comparable for age, sex, baseline APACHE II score, sepsis-related organ failure assessment score and source of infection. Initial (first 12 h) volume resuscitation (37.8±9 ml/kg of body weight vs 40±7 ml/kg) was also similar.
Analysis of the delivery versus prescription ratio was carried out every 24 h by the nephrologists in charge and, in all cases, the delivered dose was higher than 85% of the prescribed therapy.
The number of patients treated without anticoagulation was similar in the two groups (12 in the control group and 13 in the intervention group). The use of extracorporeal therapy in the absence of anticoagulation did not result in significant differences in the delivery/prescription ratio, since, by policy, the circuit was changed every 24 h with a down time in the range of 30 min.
Physiological baseline and outcome data are shown in Table 2. They show that, in the EIHF group from time 0 to time 48 h, there was a significant improvement in gas exchange as shown by the PaO2/FiO2 ratio. Also, the cardiac index, mean arterial pressure and systemic vascular resistance increased significantly ( p <0.001), while norepinephrine dose decreased significantly ( p <0.001). In the control group, no such changes were observed and the norepinephrine dose could not be reduced. Furthermore, urine output increased significantly with EIHF compared with controls.
Clinical outcome data are summarised in Table 3. Twenty-eight-day survival curves are reported for the two groups in Fig. 1. While predicted mortality was similar in the two groups (Table 3), survival was significantly better in the EIHF group. While in the intervention group (EIHF) every patient received extracorporeal therapy, in the control group 12 patients (30%) developed ARF [15] (definition of ARF fulfilled on median day 3 of sepsis; IQR:1–5 days) and only nine (75%) were treated with RRT (the indication was ARF and not sepsis). Duration of ventilation was shorter for the EIHF group than in the control group as were length of ICU and hospital stay ( p <0.001).
Discussion
The major finding of this study is that, in patients with septic shock, ALI and oliguric ARI, a protocol change to include EIHF was associated with improved recovery of gas exchange and urine production. It was also associated with earlier weaning from mechanical ventilation, shortened duration of ICU stay and increased survival. These results are provocative and require careful analysis. This study has several strengths. It is the first study to compare the clinical effects of EIHF in septic patients with ALI in the absence of fully established ARF to a control group. A previous study by Honore et al. [10] reported strong benefits in refractory septic shock but did not have a control group, as all patients were treated with short-term high-volume haemofiltration (ST-HVHF). Also, it did not focus on ALI. It was, however, prospective in design, much stronger in dose and dramatic in effect.
A controlled study by Cole et al. [17] only focussed on the short-lived physiological effects of high-volume haemofiltration (HVHF). A further report on a large series of patients by Oudemans van Straaten also offered no control patients [18]. Finally, a recent trial by Bouman and colleagues that was small but randomised and controlled did not focus on the effect of the technique in septic patients but rather on the timing of intervention in a broad group of mostly cardiothoracic surgery patients [19].
Most of our findings carry a high level of significance ( p <0.01), making it unlikely that they represent an alpha error. Furthermore, they show a beneficial effect on all major clinical outcome measures, suggesting a consistent effect. All patients were treated in the same unit and by the same group of ICU specialists; the baseline features of the patients were well balanced, and no patients in the more recent cohort were treated with recombinant human activated protein C (rhAPC). Thus, confounding treatment-related variables appear less likely to have played a major part in this study: Moreover, manipulations of fluid status appear unlikely to explain our findings, as resuscitation with fluids was similar in nature and magnitude and fluid balance was comparable. Finally, EIHF was conducted in isovolaemic mode in all cases.
We recognize, however, that this study has all the inherent limitations of retrospective investigations. They include possible selection bias, the effect of overall improvements in patient care over the duration of the study (8 years), limited availability of potentially important information (such as details of acid-base changes) and investigator commitment to the study technique inclusive of a potential nonspecific increase in patient care (so-called Hawthorne effect). All of these factors may be responsible for our findings and limit the scope and implications of our observations. Nonetheless, patient identification was according to pre-specified criteria; baseline and outcome information is numerical and objective in nature and the outcome measures robust and not subject to manipulation. Furthermore, we are not aware of striking improvements in patient outcomes in our unit over the same time period or of the development or applications of novel therapeutic approaches that might independently explain our findings.
Our observations must also be seen within the context of previous studies, which suggest a possible beneficial effect of HVHF in septic patients. The strongest one of these was conducted by Honore and colleagues [10]. These investigators found that, if short-term HVHF was applied to patients with refractory septic shock, according to time and dose delivered, close to 50% showed a dramatic improvement. Cole et al. [17] reported that, when HVHF was used in patients with septic shock, norepinephrine requirements decreased significantly as did the blood levels of several inflammatory mediators. In another study of ARF, Ronco et al. [20] found that, in ICU patients with combined sepsis and ARF, there was a trend toward increased survival when higher doses of CVVH were applied. These observations are consistent with our study, reflecting the possibility of a true biological effect. They are also consistent with the paradigm (the humoral theory of sepsis) that provides a rationale for blood purification therapies in sepsis [21, 22, 23, 24, 25,26].
No contrary evidence currently exists for HVHF in septic shock. However, other studies of lower dose intervention such as CVVH at 2 l/h of ultrafiltration [27] or low-grade continued plasma filtration [28] have failed to show a benefit of blood purification in sepsis. It is of interest that we find a similar outcome in these patients to those reported in a previous study of 45 ml/kg/h of ultrafiltration dose in patients with ARF [20]. This is despite the fact that, according to APACHE II scoring, this cohort was significantly sicker. This observation might reflect the limitations of the APACHE II scoring system but might also be taken to suggest that the benefits of higher dose treatment might be particularly strong in septic patients. It is thus possible that the interaction of pathophysiological state, timing and dose of treatment are important in determining the efficacy of treatment.
Carefully assessing both survival curves, a significant change in survival appears to occur at about 2 weeks, when, in most of the studies using HVHF, the so-called “non-responders” or “non-survivors” appear to die within 24 h from refractory shock [10] or within 72 h from early MOF [29]. It may well be that in our study, EIHF did not only work by removing proinflammatory mediators, thus explaining the haemodynamic changes, but also by removing anti-inflammatory mediators with a restoration of immune competence [30]. This might explain the “late” difference in mortality between groups and is consistent with the peak concentration hypothesis [31] and the possible effect of prolonging the initial EIHF effect by following up with standard CVVH 24 h a day. In fact, while the high volume exchange of plasma water may be beneficial in removing substantial amounts of mediators, the continuity of the extracorporeal therapy may be important to cut the peaks of both proinflammatory and anti-inflammatory mediators in the circulation and resetting the immune system to a more physiological level of function.
Our observations, together with those of others, suggest that it may now be time for a moderately large phase IIb randomised multicentre controlled trial of early-HVHF in ICU patients with sepsis. Such a trial is likely to be costly but necessary to justify a larger phase III study, given the cost of therapy and the technical demands associated with it.
A final comment should be made on the operational characteristics of the haemofiltration therapy. If prospective studies on high volume haemofiltration are to be designed, both blood flow and the surface area of filters should be increased. This will have the important result of reducing filtration fraction and at the same time, improving efficiency due to the increased KoA (permeability × surface area product) of the filter. It should be pointed out, however, that higher surface areas are only beneficial if the blood flow is sufficiently high; otherwise the curve of ultrafiltration and that of clearance reach a plateau, which is determined by insufficient blood flow and not by the small surface of the membrane.
In summary, we report the results of a retrospective study describing the effect of EIHF in septic shock patients with ALI and ARI in a single unit after a change of protocol was introduced. Our observations suggest a possible beneficial effect on both pulmonary and renal function, as well as survival. Taken in the context of other studies, they also suggest that a multicentre randomised controlled trial of early and higher dose haemofiltration is now justified.
References
Brivet FG, Kleinknecht DJ, Loirat P, Landais PJ (1996) Acute renal failure in intensive care units—causes, outcome, and prognostic factors of hospital mortality; a prospective, multicenter study. French Study Group on Acute Renal Failure. Crit Care Med 24(2):192–198
de Mendonca A, Vincent JL, Suter PM,Moreno R, Dearden NM, Antonelli M, Takala J, Sprung C, Cantraine F (2000) Acute renal failure in the ICU: risk factors and outcome evaluated by the SOFA score. Intensive Care Med 26(7):915–921
Wheeler AP, Bernard GR (1999) Treating patients with severe sepsis. N Engl J Med 21 340(3):207–214
Liano G, Pascual J (1996) Acute renal failure. Madrid Acute Renal Failure Study Group. Lancet 17:347:479
Tonelli M, Manns B, Feller-Kopman D (2002) Acute renal failure in the intensive care unit: a systematic review of the impact of dialytic modality on mortality and renal recovery. Am J Kidney Dis 40:875–885
Bernard GR, Vincent JL, Laterre PF, LaRosa SP, Dhainaut JF, Lopez-Rodriquez A, Steingrub JS, Garber GE, Helterbrand JD, Ely EW, Fisher CJ for the Recombinant Human Activated Protein C Worldwide Evaluation in Severe Sepsis (PROWESS) Study Group (2001) Efficacy and safety of recombinant human activated protein C for severe sepsis. New Engl J Med 344:699–709
Noble JS, MacKirdy FN, Donaldson SI, Howie JC (2001) Renal and respiratory failure in Scottish ICUs. Anaesthesia 56:124–129
Kramer AA, Postler G, Salhab KF, Mendez C, Carey LC, Rabb H (1999) Renal ischemia/reperfusion leads to macrophage-mediated increase in pulmonary vascular permeability. Kidney Int 55(6):2362–2367
Rocker GM, Morgan AG, Shale D (1988) Pulmonary oedema and renal failure. Nephrol Dial Transplant 3:244–246
Honore PM, Jamez J, Wauthier M et al (2000) Prospective evaluation of short-term, high-volume isovolemic hemofiltration on the hemodynamic course and outcome inpatients with intractable circulatory failure resulting from septic shock. Crit Care Med 28:3581–3587
Bellomo R, Kellum JA, Gandhi CR, Pinsky MR (2000)The effect of intensive plasma water exchange by hemofiltration on hemodynamics and soluble mediators in canine endotoxemia. Am J Respir Crit Care Med 161:1429–1436
Bernard GR, Artigas A, Brigman KL, Carlet G, Falke K, Hudson L, Lamy M, Le Gall JR, Morris A, Spragg R (1994) The American-European Consensus Conference on ARDS. Definitions, mechanisms, relevant outcomes, and clinical trial coordination. Am J Respir Crit Care Med 149:818–824
Vincent JL, Moreno R, Takala J, Willatts S, de Mendonca A, Bruining H, Reinhart CK, Suter PM, Thijs LG (1996) The SOFA (Sepsis-related Organ Failure Assessment) score describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Med. Intensive Care Med 22:707–710
Bellomo R, Ronco C (1998) Indications and criteria for initiating renal replacement therapy in the intensive care unit. Kidney Int 53 [Suppl 66]: S106–109
Bellomo R, Kellum J, Ronco C (2001) Acute renal failure: time for consensus. Intensive Care Med 27:1685–1688
Knaus WA, Draper EA, Wagner DP, Zimmerman JE (1985) APACHE II: A severity of disease classification system. Crit Care Med 13:818–829
Cole L, Bellomo R, Journois D, Davenport P, Baldwin I, Tipping P (2001) High-volume hemofiltration in human septic shock. Intensive Care Med 27:978–986
Oudemans van Straaten HM, Bosman RJ, van der Spoe JI, Zandstra DF (1999) Outcome of critically ill patients treated with intermittent high-volume haemofiltration: a prospective cohort analysis. Intensive Care Med 25:814–821
Bouman CS, Oudemans van Straaten HM, Tijssen J (2002) Effects of early high-volume continuous venovenous hemofiltration on survival and recovery of renal function in intensive care patients with acute renal failure: a prospective randomized trial. Crit Care Med 30:2205–2211
Ronco C, Bellomo R, Homel P, Brendolan A, Dan M, Piccinni P, La Greca G (2000) Effects of different doses in continuous veno-venous haemofiltration on outcomes of acute renal failure: a prospective randomised trial. Lancet 356(9223):26–30
De Vriese AS, Colardyn FA, Philippe JJ, Vanholder RC, De Sutter JH, Lameire NH (1999)Cytokine removal during continuous hemofiltration in septic patients. J Am Soc Nephrol 10(4):846–853
Li Wan, Rinaldo Bellomo, David Di Giantomasso, Claudio Ronco (2003) The pathogenesis of septic acute renal failure. Curr Opin Crit Care 9:496–502
Van Biesen W, Vanholder R, Lameire N (2003) Dialysis strategies in critically ill acute renal failure patients Curr Opin Crit Care 9:491–495
Busund R, Koukline V, Utrobin U, Nedashkovsky E (2002) Plasmapheresis in severe sepsis and septic shock: a prospective, randomised, controlled trial. Intensive Care Med 28(10):1434–1439
Ronco C, Brendolan A, Lonnemann G (2002) A pilot study of coupled plasma filtration with adsorption in septic shock. Crit Care Med 30:1250–1255
Tetta C, Gianotti L, Cavaillon JM et al(2000). Coupled plasmafiltration-adsorption in a rabbit model of endotoxic shock. Crit Care Med 28:1526–1533
Cole L, Bellomo R, Silvester W, Reeves JH (2000) A prospective, multicenter study of the epidemiology, management, and outcome of severe acute renal failure in a “closed” ICU system. Am J Respir Crit Care Med 162:191–196
Reeves JH, Butt WW, Shann F, and the Plasmafiltration in Sepsis Study Group (1999) Continuous plasmafiltration in sepsis syndrome. Crit Care Med 27:2096–2104
Joannes-Boyau O, Rapaport S, Bazin R, Fleureau C, Janvier G (2004) Impact of high-volume hemofiltration on hemodynamic disturbance and outcome during septic shock. ASAIO J 50(1):102–109
Yekebas EF, Strate T, Zolmaid S, Eisemberger CF, Erbersdobler A, Saalmuller A, Steffani K, Busch C, Elsner HA (2002) Impact of different modalities of continuous venovenous hemofiltration on sepsis-induced alterations in experimental pancreatitis. Kidney Int 62(5):1806–1818
Ronco C, Bonello M, Bordoni V, Ricci Z, D’Intini V, BellomoR, Levi NW (2004) Extracorporeal therapies in non-renal disease: treatment of shock and the peak concentration hypothesis. Blood Purif 22(1):164–174
Acknowledgements
We are indebted to several dedicated physicians and nurses in our ICU and Nephrology Department for their support and to Luca Marinoni for his help with data analysis and management.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article refers to the editorial http://dx.doi.org/10.1007/s00134-005-2866-z
Electronic Supplementary Material
Rights and permissions
About this article
Cite this article
Piccinni, P., Dan, M., Barbacini, S. et al. Early isovolaemic haemofiltration in oliguric patients with septic shock. Intensive Care Med 32, 80–86 (2006). https://doi.org/10.1007/s00134-005-2815-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-005-2815-x