Abstract
Objective
Esophageal Doppler allows continuous monitoring of stroke volume index (SVI) and corrected flow time (FTc). We hypothesized that variations in stroke output index SOI (SVI/FTc) during volume expansion can predict the hemodynamic response to subsequent fluid loading better than the static values.
Design and setting
Prospective study in the intensive care unit of a university hospital.
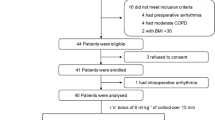
Patients
Fifty-one patients with circulatory failure were monitored by esophageal Doppler.
Interventions
Patients who responded to a first fluid challenge received a second one. Patients who responded to both were classified as responders-responders, and those who did not respond to the second as responders-nonresponders. In these two groups we compared ΔSVI, ΔFTc, and ΔSOI during each fluid challenge and also static values at the end of each fluid challenge.
Measurements and results
After the first fluid challenge ΔSOI and ΔSVI were significantly higher in patients who responded to subsequent volume expansion than in patients who no longer responded. ROC curves showed that ΔSOI was a better predictor of fluid responsiveness than ΔSVI. During volume expansion a ΔSOI value of 11% discriminated between responders and nonresponders to subsequent volume expansion with a sensitivity of 91% and a specificity of 97%. There was no significant difference between the two groups for FTc value at the end of first fluid challenge.
Conclusions
Analysis of ΔSOI during fluid challenge predicts response to subsequent fluid challenge and FTc is not a reliable indicator of cardiac preload.




Similar content being viewed by others
References
Dellinger RP, Carlet JM, Gerlach H, Ramsey G, Levy M (2004) Surviving sepsis campaign guidelines for management of severe sepsis and septic shock. Crit Care Med 32:858–873
Arieff AI (1999) Fatal postoperative pulmonary edema: pathogenesis and literature review. Chest 115:1371–1377
Michard F, Boussat S, Chemla D, Anguel N, Mercat A, Lecarpentier Y, Richard C, Pinsky MR, Teboul JL (2000) Relation between respiratory changes in arterial pulse pressure and fluid responsiveness in septic patients with acute circulatory failure. Am J Respir Crit Care Med 162:134–138
Slama M, Masson H, Teboul JL, Arnould ML, Nait-Kaoudjt R, Colas B, Peltier M, Tribouilloy C, Susic D, Frohlich E, Andrejak M (2004) Monitoring of respiratory variations of aortic blood flow velocity using esophageal Doppler. Intensive Care Med 30:1182–1187
Slama M, Masson H, Teboul JL, Arnout ML, Susic D, Frohlich E, Andrejak M (2002) Respiratory variations of aortic VTI: a new index of hypovolemia and fluid responsiveness. Am J Physiol Heart Circ Physiol 283:1729–1733
Feissel M, Michard F, Mangin I, Ruyer O, Faller JP, Teboul JL (2001) Respiratory changes in aortic blood velocity as an indicator of fluid responsiveness in ventilated patients with septic shock. Chest 119:867–873
Reuter DA, Kirchner A, Felbinger TW, Weis FC, Kilger E, Lamm P, Goetz AE (2003) Usefulness of left ventricular stroke volume variation to assess fluid responsiveness in patients with reduced cardiac function. Crit Care Med 31:1399–1404
Reuter DA, Felbinger TW, Schmidt C, Kilger E, Goedje O, Lamm P, Goetz AE (2002) Volume variations for assessment of cardiac responsiveness to volume loading in mechanically ventilated patients after cardiac surgery. Intensive Care Med 28:392–398
Krishnamurthy B, McMurray TJ, McClean E (1997) The peri-operative use of the oesophageal Doppler monitor in patients undergoing coronary artery revascularisation. A comparison with the continuous cardiac output monitor. Anaesthesia 52:624–629
Leone D, Servillo G, De Robertis E, Rossano F, Tufano R (1998) Monitoring cardiac output: esophageal doppler vs thermodilution. Minerva Anestesiol 64:351–356
Baillard C, Cohen Y, Fosse JP, Karoubi P, Hoang P, Cupa M (1999) Haemodynamic measurements (continuous cardiac output and systemic vascular resistance) in critically ill patients: transoesophageal Doppler versus continuous thermodilution. Anaesth Intensive Care 27:33–37
Keyl C, Rodig G, Lemberger P, Hobbhahn J (1996) A comparison of the use of transoesophageal Doppler and thermodilution techniques for cardiac output determination. Eur J Anaesthesiol 13:136–142
Sinclair S, James S, Singer M (1997) Intraoperative intravascular volume optimisation and length of hospital stay after repair of proximal femoral fracture: randomised controlled trial. BMJ 315:909–912
Conway DH, Mayall R, Abdul-Latif MS, Gilligan S, Tackaberry C (2002) Randomised controlled trial investigating the influence of intravenous fluid titration using oesophageal Doppler monitoring during bowel surgery. Anaesthesia 57:845–849
Venn R, Steele A, Richardson P, Poloniecki J, Grounds M, Newman P (2002) Randomized controlled trial to investigate influence of the fluid challenge on duration of hospital stay and perioperative morbidity in patients with hip fractures. Br J Anaesth 88:65–71
Gan TJ, Soppitt A, Maroof M, El Moalem H, Robertson KM, Moretti E, Dwane P, Glass PS (2002) Goal-directed intraoperative fluid administration reduces length of hospital stay after major surgery. Anesthesiology 97:820–826
American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference (1992) Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Crit Care Med 20:864–874
Legall J, Lemeshow S, Saulnier F (1993) New Simplified Acute Physiology Score (SAPS II) based on a European/North American Multicenter Study. JAMA 270:2957–2963
Hanley JA, McNeil BJ (1983) A method of comparing the areas under receiver operating characteristic curves derived from the same cases. Radiology 148:839–843
Madan AK, UyBarreta VV, Aliabadi-Wahle S, Jesperson R, Hartz RS, Flint LM, Steinberg SM (1999) Esophageal Doppler ultrasound monitor versus pulmonary artery catheter in the hemodynamic management of critically ill surgical patients. J Trauma 46:607–611
DiCorte CJ, Latham P, Greilich PE, Cooley MV, Grayburn PA, Jessen ME (2000) Esophageal Doppler monitor determinations of cardiac output and preload during cardiac operations. Ann Thorac Surg 69:1782–1786
Michard F, Teboul JL (2002) Predicting fluid responsiveness in ICU patients: a critical analysis of the evidence. Chest 121:2000–2008
Lefrant JY, Bruelle P, Aya AG, Saissi G, Dauzat M, de La Coussaye JE, Eledjam JJ (1998) Training is required to improve the reliability of esophageal Doppler to measure cardiac output in critically ill patients. Intensive Care Med 24:347–352
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Vallée, F., Fourcade, O., De Soyres, O. et al. Stroke output variations calculated by esophageal Doppler is a reliable predictor of fluid response. Intensive Care Med 31, 1388–1393 (2005). https://doi.org/10.1007/s00134-005-2768-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-005-2768-0