Abstract
Objective
To study the effects of two levels of positive end-expiratory pressure (PEEP), 2 cmH2O above the lower inflection point of the inspiratory limb and equal to the point of maximum curvature on the expiratory limb of the pressure-volume curve, in gas exchange, respiratory mechanics, and lung aeration.
Design and setting
Prospective clinical study in the intensive care unit and computed tomography ward of a university hospital.
Patients
Eight patients with early acute lung injury.
Interventions
Both limbs of the static pressure-volume curve were traced and inflection points calculated using a sigmoid model. During ventilation with a tidal volume of 6 ml/kg we sequentially applied a PEEP 2 cmH2O above the inspiratory lower inflection point (15.5±3.1 cmH2O) and a PEEP equal to the expiratory point of maximum curvature (23.5±4.1 cmH2O).
Measurements and results
Arterial blood gases, respiratory system compliance and resistance and changes in lung aeration (measured on three computed tomography slices during end-expiratory and end-inspiratory pauses) were measured at each PEEP level. PEEP according to the expiratory point of maximum curvature was related to an improvement in oxygenation, increase in normally aerated, decrease in nonaerated lung volumes, and greater alveolar stability. There was also an increase in PaCO2, airway pressures, and hyperaerated lung volume.
Conclusions
High PEEP levels according to the point of maximum curvature of the deflation limb of the pressure-volume curve have both benefits and drawbacks.
Similar content being viewed by others
Introduction
Lung protective ventilation in acute lung injury (ALI) is based on the use of small tidal volumes and high levels of positive end-expiratory pressure (PEEP) [1]. The aims of this strategy are to avoid end-inspiratory overdistension and cyclic changes in alveolar aeration, which are known mechanisms of ventilator-induced lung injury [2]. Studies have demonstrated the benefits, in terms of mortality, of a reduction in tidal volumes [3, 4], but the optimal PEEP level is not known. Some studies have addressed the effects of arbitrary PEEP increments in ALI with consistent results; both recruitment and overdistension increase with PEEP.
The static pressure-volume curves of the respiratory system have been used as a tool to set the ventilator [5]. An approach based on the so-called lower inflection point (LIP) of the inspiratory limb of the static pressure-volume curve has been tested in one trial [3], but other authors have proposed the use of the deflation limb of the pressure-volume curve for PEEP setting [6, 7]. The point of maximum curvature (PMC) of this limb is related to a higher aeration (increase in normally aerated lung) and recruitment (decrease in nonaerated lung) with no significant increments in hyperinflated lung in static conditions [8] and during high frequency oscillatory ventilation [9], but there are no clinical studies using this point as PEEP level during conventional mechanical ventilation.
We hypothesized that use of the PMC would allow individual titration of the PEEP level during early ALI, resulting in increased recruitment and alveolar stability without increasing hyperinflation. Therefore the aim of this study was to compare the effects of two different PEEP levels, based on the inspiratory LIP or expiratory PMC of the pressure-volume curve, in gas exchange, lung mechanics, and changes in gas distribution in the lungs, using computed tomography (CT). Some of the results of this study have been previously reported in the form of an abstract [10].
Methods and materials
Study protocol was approved by the regional ethics committee. Informed consent was obtained by each patient’s next of kin. We screened 32 consecutive patients between September 2003 and February 2004 who met ALI criteria [11]. Exclusion criteria were: younger than 18 years, more than 3 days from ALI diagnosis or more than 5 days of mechanical ventilation, presence of air leaks, brain injury, severe hemodynamic impairment (hypotension nonresponsive to vasoactive drugs), and chronic respiratory diseases (based on medical history). We excluded 24 patients (age 52.6±19.1 years, Acute Physiology and Chronic Health Evaluation II 19.1±7.6, PaO2/FIO2 150±72): 18 due to prolonged ventilation (mostly ALI secondary to nosocomial infections), 3 to air leaks, and 3 to severe hemodynamic compromise). Thus 8 patients were studied; their demographic and clinical data are shown in Table 1.
Protocol overview
Patients were under deep sedation (midazolam and fentanyl) and relaxed (vecuronium bromide), with arterial pressure, electrocardiographic, and pulse-oxymetry monitoring throughout the study. They were ventilated [tidal volume 7.2±2 ml/kg predicted body weight, PEEP (12.4±3.7 cmH2O) and respiratory rate (17±5 breaths/min) according to the responsible physician] in volume-controlled mode with constant flow using an Evita 4 ventilator (Drager, Lübeck, Germany). Data from the ventilator was acquired and stored in a computer using VentView software (Drager). After inclusion the patient’s demographic and clinical data were obtained, and a pressure-volume curve between airway pressures from 0 to 35 cmH2O was traced as previously described [8]. Briefly, after standardization of lung volume history with three sighs (tidal volume of 10 ml/kg), the ventilator was switched to continuous positive airway pressure mode, and the airway pressure decreased to 0 cmH2O, allowing a complete deflation. After this the airway pressure was increased from 0 to 35 cmH2O in steps of 5 cmH2O. This sequence was used to trace the inspiratory limb of the pressure-volume curve. Then basal ventilation was restored for 5 min. To trace the deflation limb of the curve the ventilator was again switched to continuous positive airway pressure mode, with an airway pressure of 0 cmH2O until complete exhalation. The airway pressure was then raised to 35 cmH2O, and decreased in steps of 5 cmH2O until 0 cmH2O. FIO2 was 1 during this procedure. Each change in airway pressure was carried out only when flow reached the zero level, to ensure static conditions. LIP and PMC were calculated from these curves (see below).
Tidal volume was then set to 6 ml/kg predicted body weight, respiratory rate adjusted to maintain minute ventilation, and PEEP fixed at LIP +2 cmH2O. In less than 3 h following the curve tracing patients were transferred to the CT ward and connected there to another Evita ventilator with the same monitoring and data acquisition system as in the ICU. An Oxylog 2000 ventilator (Drager) was used during the transportation, keeping the same ventilatory parameters. Derecruitment was prevented during ventilator disconnections by means of a clamp in the endotracheal tube. Inspired oxygen fraction was set at 1 during transport and CT. After an equilibrium time of 15 min on the CT table arterial pressures and heart rate were noted, an arterial blood sample was drawn for gas analysis (Rapidlab 840, Bayer Diagnostics, Barcelona, Spain), and end-expiratory and end-inspiratory occlusions were performed to measure compliance and resistance. Total resistance was partitioned into intrinsic and additional resistance [12]. CT was then carried out (see below). After this the PEEP was raised to the PMC, keeping constant other ventilatory settings, and all the measurements were repeated after another equilibrium time of 15 min.
Pressure-volume curve analysis
Data pairs of pressure and volume were fitted to a sigmoidal model modified from the equation proposed by Venegas and coworkers [7]. The equation for this model is Vol=b/{1+ EXP [−(Paw−c)/d]}, where Vol is volume, Paw is airway pressure, b is the upper asymptote of the curve, c is the pressure where curvature changes sign, and d is the pressure range where most of the volume change occurs (Fig. 1). This model allows an objective and reproducible calculation of the inflection points as follows: On the inspiratory limb LIP was equal to c−1.317d and the upper inflection point to c+1.317d. On the deflation limb PMC was calculated as c+1.317d. These points correspond to the pressure where the curve has its maximal upward or downward curvature. Fitting was performed using the least squares method. Mean R2 values were 0.991±0.007 and 0.994±0.007 (for the inspiratory and expiratory limbs, respectively).
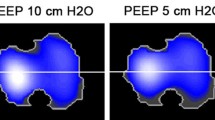
Computed tomography
The lungs were studied at three arbitrary levels selected at the middle of the upper, medium, and lower lobes of the right lung in a frontal view taken at a PEEP level equal to the LIP. Images 1 mm thick were taken at 120 kV and 335 mA/s. Voxel volume was 0.42 µl (0.65×0.65×1 mm). These levels were kept constant throughout the protocol. One slice per lung level was acquired during prolonged end-expiratory and end-inspiratory pauses, with a 4- to 5-min interval between them. Images were saved in DICOM format and analyzed using the software ImageJ with the 16-bit histogram plugin (National Institutes of Health, USA; freely available at http://rsb.info.nih.gov/ij/). The contour of each lung was drawn by one researcher (G.M.A.), blinded to the airway pressure applied, and the histogram from −1000 to +100 HU was obtained and transferred to a spreadsheet (Excel, Microsoft, Redmond, Wash., USA). Lung tissue was divided into four compartments using previously published thresholds [13]: hyperinflated (−1000 to −900 HU), normally aerated (−899 to −500 HU), poorly aerated (−499 to −100 HU), and nonaerated (−99 to +100 HU). The volume of these compartments was calculated in each slice by multiplying the number of voxels by the voxel volume (0.42 µl).
Statistics
All results are expressed as mean ±SD. Normal distribution of the data was assessed by the Kolgomorov-Smirnov test. Gas exchange, compliance, resistance, heart rate, and blood pressure values were compared using the t test for paired samples. Data derived from CT were compared using an analysis of variance, with three within-group factors: lung level studied (upper, medium, or lower lobes), tidal cycle phase (end-inspiration or end-expiration), and PEEP level (LIP or PMC). This test was repeated for each lung compartment. When significant, post-hoc tests were carried out using Bonferroni’s correction. Differences at a p level lower than 0.05 were considered significant. All calculations were performed using SPSS 11.0 software (SPSS, Chicago, Ill., USA).
Results
Ventilatory management
Patients were ventilated with a tidal volume of 368±72 ml and a respiratory rate of 21±2 breaths per minute. Airway pressures corresponding to LIP and PMC were 14.1±3.2 and 24±4.5 cmH2O respectively, and therefore studied PEEP levels (set at the closest integer number) were 15.5±3.1 and 23.5±4.1 cmH2O (p<0.05 for the difference). The upper inflection point of the inspiratory curve was placed at 27.6±2.6 cmH2O. There were no changes in blood pressures (mean arterial pressures 88±24 vs. 82±18 mmHg) or heart rate (101±28 vs. 103±31 beats per minute) when PEEP was raised from LIP+2 cmH2O to the PMC.
Gas exchange
Ventilation above PMC was related to an increase in PaO2 (269±94 vs. 166±62 mmHg, p<0.05) and in PaCO2 (54±7 vs. 51±7 mmHg, p<0.05) when compared to ventilation above the LIP. There were no changes in arterial pH (7.25±0.1 vs. 7.26±0.1 respectively, p=0.7).
Lung mechanics
All airway pressures were higher during ventilation above PMC (Table 2). There were no significant changes in auto-PEEP, static compliance, or in total, intrinsic, or additional resistances.
Computed tomography
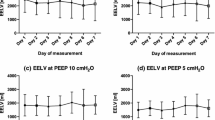
We found no regional differences in the changes in hyperinflation, aeration, or recruitment between the three lung levels studied, and we therefore present mean values of pooled data. When PEEP was raised to the PMC, there was an increase in the volume of hyperaerated and normally aerated lung tissue (Fig. 2A, B). The differences along the respiratory cycle were not statistically significant. The changes in volume of poorly aerated lung were not significant (Fig. 2C). The volume of nonaerated lung decreased during ventilation above the PMC, with a significant difference between end-expiration and end-inspiration only during ventilation above the LIP (Fig. 2D). To distinguish between recruiters and nonrecruiters we plotted recruitment achieved with PEEP against the increase in hyperaeration (Fig. 3). All patients showed an increment in both recruitment and hyperaeration.
Changes in volume of hyperaerated (A), normally aerated (B), poorly aerated (C), and nonaerated (D) lung along the respiratory cycle with positive end-expiratory pressure set at the inspiratory lower inflection point plus 2 cmH2O (circles, dotted line) and at the expiratory point of maximum curvature (squares, continuous line). *p<0.05 (post-hoc test)
There was a linear relationship between the increase in PaO2 and the decrease in expiratory poorly aerated plus nonaerated volume with the PEEP change (r=0.85, p=0.007, slope −0.021, y-intercept −25.6 mmHg; Fig. 4). This relationship was not significant only when changes in nonaerated lung were controlled for (r=0.61, p=0.10, slope −0.0062; y-intercept 47.7 mmHg). There was no significant relationship between the changes in PaCO2 and the hyperaerated lung volume (p=0.65 and p=0.73 for expiratory and inspiratory hyperaeration, respectively).
Discussion
The main finding of this study is that the use of the PMC on the deflation limb of the pressure-volume curve as PEEP level in ALI is related to an increase in oxygenation, recruitment, and alveolar stability and to an increase in hyperinflated lung tissue and signs of overstretching compared to a PEEP level above the LIP of the inflation limb of the curve. Although the deflation limb of the pressure-volume curve has been proposed as a better marker of “optimal” PEEP, these results show that the use of PMC keeping tidal volume constant has both benefits and drawbacks.
Limitations of the study
Our methodology is subject to some limitations: First, the sample size was small. Since only eight patients were included, the study may have been underpowered to detect differences between ALI subgroups (i.e., pulmonary vs. extrapulmonary [14], diffuse vs. focal [15]) with a different response to PEEP increments. Second, the pressure-volume curve shows some variability with time [16] and ventilatory pattern [17] and can change if chest wall mechanics are taken into account [18]. We therefore cannot exclude that our results would change with different techniques, mathematical models, or ventilatory strategies. Third, To reduce radiation exposure we studied only three CT lung slices per pressure level. As injured lungs are heterogeneous [19], our results may have differed if we had acquired a whole-lung scan [20]. However, changes in aeration were similar at each lung level, and therefore we consider that the trends would be the same in a whole-lung scan. In the same sense, a FIO2 value different from 1 would have decreased the total volume of nonaerated tissue (due to the atelectasis seen with pure oxygen ventilation). Finally, the equilibrium time for each PEEP trial was limited to minimize risks. A period of 15 min may not enough to ensure a complete steady state in variables such as PaCO2 or recruitment, and a longer time may have yielded even greater differences. The PEEP order was not randomized, nor were recruitment maneuvers performed to avoid transient effects in recruitment other than those caused by the PEEP increment.
Changes in recruitment
PEEP is an expiratory phenomenon aimed at maintaining the recruitment achieved during inspiration. The limbs of the pressure-volume curve have a good correlation with recruitment and derecruitment [8, 21, 22], and LIP is the marker of the start of this recruitment. However, ventilation occurs along the deflation limb of the pressure-volume curve, specially in recruited lungs [23]. and some authors have proposed the use of the PMC as a marker of the PEEP level that completely avoids the loss of aeration [6]. This can explain the findings of improved end-expiratory aeration with PEEP levels above the LIP in some clinical studies [24, 25] and agrees with mathematical models of injured lungs [7, 16] and with our results. Moreover, as in experimental settings [26] high PEEP levels decrease alveolar instability (defined as changes in recruitment in each tidal cycle), a known mechanism of ventilator-induced lung injury [27]. The decreased tidal recruitment may be partially responsible of the trend to a lower respiratory system compliance during ventilation with PEEP at the PMC [24].
The functional consequence of the improvement in aeration and recruitment was an increase in PaO2. The relationship between changes in oxygenation and changes in recruitment was statistically significant only when changes in poorly aerated and nonaerated lung were added, as found by other authors [28]. It is possible that at high PEEP levels the shift from nonaerated to poorly aerated zones makes these zones with low ventilation/perfusion ratios more important in gas exchange than at low levels of PEEP (where the true shunt across nonaerated areas is the main determinant of oxygenation).
Changes in hyperinflation
Ventilation using high PEEP levels cause also hyperinflation of some zones [29, 30, 31]. Inhomogeneities in lung injury and ventilation distribution are responsible for the risk of overdistension of healthy alveoli with pressure levels required to keep injured zones aerated [32]. This result is also explained by mathematical models that consider not only recruitment but also overstretching [33].
Hyperinflation (gas overfilling) is different from overdistension (increased alveolar wall tension) [21]. CT may underestimate hyperinflation when there is an excess of lung tissue (as in ALI) [34], or when thick CT slices are used [15]. It must be noted that the hyperaerated volume in end-expiration with PEEP at the PMC was higher than that in end-inspiration using a PEEP at LIP +2 cmH2O, in spite of a lower airway pressure (24 vs. 27.3 cmH2O). The recruitment caused by high PEEP and plateau pressure can unmask hyperaerated zones due to a lower alveolar heterogeneity and a lower density to be averaged inside the voxel (less partial volume artifacts).
Although these issues raise concerns about the use of CT to monitor hyperaeration and overdistension, the high plateau pressure (above the inspiratory upper inflection point), the increase in PaCO2 and the trend to a lower compliance suggest that there is significant overstretching during ventilation above the PMC. The only way to decrease ventilator-induced lung injury at such high pressures is to reduce tidal volume. This can be decreased using the inspiratory upper inflection point as maximum plateau pressure [35], with no changes in oxygenation but an increase in PaCO2. The extreme of this strategy is high-frequency oscillatory ventilation, where the use of PMC has been used as a marker of optimal pressure [9].
Changes in hemodynamics
We did not observe changes in arterial pressures or heart rate during the study. High PEEP levels can impair cardiac output and right ventricular function [36], especially in hypovolemic patients (patients in the study were given fluids until a systolic arterial pressure variation lower than 10%). The short study period, the absence of other measurements, and the increase in PaCO2 may have masked some hemodynamic changes. When high airway pressures are applied, a careful circulatory monitoring and management is essential [37].
Clinical implications
Among the various strategies for mechanical ventilation setting in ALI the use of pressure-volume curves has been proposed as a method to set PEEP according to the individual characteristics of the respiratory system [38]. The evidence of increased recruitment with PEEP levels above the LIP, derived from mathematical models [7, 39] and from experimental [21] and clinical [22, 24, 25, 40] studies, led to an increasing interest on the deflation limb of the curve. This approach has it own weakness [38]: the expiratory pressure-volume curve is the result of not only derecruitment but also the changes in aeration and airway closure. More importantly, pressure-volume curves have not been shown superior to other strategies to set PEEP. A recent study compared high vs. low PEEP using a FIO2-PEEP table to set the ventilator, and found no differences in survival [41].
To our knowledge, the PMC had not previously been tested as PEEP level in a clinical setting before. The only study in patients dealing with PEEP setting according to the deflation limb of the pressure-volume curve was conducted by Holzapfel et al. [42]. They found a good correlation between the true expiratory inflection point (where curvature changes sign) and the lowest PEEP level that achieves the maximum decrease in pulmonary shunt. In a saline-lavage animal model [43], PEEP set at the PMC was related to more hypercapnia and a trend to more lung injury than a PEEP level at LIP +2 cmH2O, with no benefits in oxygenation.
Thus high pressure levels required to decrease two mechanisms of ventilator-induced lung injury (an increase in nonaerated lung tissue and tidal changes in aeration) increase a third one (overstretching). More studies dealing with the relative importance of each of these mechanisms are required in order to analyze the optimal PEEP level as a risk/benefit issue.
Conclusions
The benefits and drawbacks of PEEP found in this study are similar to those found in other studies using arbitrary PEEP levels. The use of pressure-volume curves has been proposed for years as a tool to titrate PEEP to improve oxygenation and, more importantly, to decrease ventilator-induced lung injury. However, we failed to find a safe level for PEEP at the PMC of the expiratory pressure-volume curve.
References
Brower RG, Rubenfeld GD (2003) Lung-protective ventilation strategies in acute lung injury. Crit Care Med 31:S312–S316
Dreyfuss D, Saumon G (1998) Ventilator-induced lung injury: lessons from experimental studies. Am J Respir Crit Care Med 157:294–323
Amato MB, Barbas CS, Medeiros DM, Magaldi RB, Schettino GP, Lorenzi-Filho G, Kairalla RA, Deheinzelin D, Munoz C, Oliveira R, Takagaki TY, Carvalho CR (1998) Effect of a protective-ventilation strategy on mortality in the acute respiratory distress syndrome. N Engl J Med 338:347–354
Acute Respiratory Distress Syndrome Network (2000) Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med 342:1301–1308
Putensen C, Baum M, Hormann C (1993) Selecting ventilator settings according to variables derived from the quasi-static pressure/volume relationship in patients with acute lung injury. Anesth Analg 77:436–447
Hickling KG (2001) Best compliance during a decremental, but not incremental, positive end- expiratory pressure trial is related to open-lung positive end- expiratory pressure: a mathematical model of acute respiratory distress syndrome lungs. Am J Respir Crit Care Med 163:69–78
Venegas JG, Harris RS, Simon BA (1998) A comprehensive equation for the pulmonary pressure-volume curve. J Appl Physiol 84:389–395
Albaiceta GM, Taboada F, Parra D, Luyando LH, Calvo J, Menendez R, Otero J (2004) Tomographic study of the inflection points of the pressure-volume curve in acute lung injury. Am J Respir Crit Care Med 170:1066–1072
Goddon S, Fujino Y, Hromi JM, Kacmarek RM (2001) Optimal mean airway pressure during high-frequency oscillation: predicted by the pressure-volume curve. Anesthesiology 94:862–969
Albaiceta GM, Luyando LH, Parra D, Menendez R, Calvo J, Taboada F (2003) Inspiratory vs expiratory limb of the pressure-volume curve for the positive end-expiratory pressure setting in acute lung injury (abstract). Crit Care 8:25
Bernard GR, Artigas A, Brigham KL, Carlet J, Falke K, Hudson L, Lamy M, LeGall JR, Morris A, Spragg R (1994) Report of the American-European consensus conference on ARDS: definitions, mechanisms, relevant outcomes and clinical trial coordination. The Consensus Committee. Intensive Care Med 20:225–232
D’Angelo E, Calderini E, Tavola M, Bono D, Milic-Emili J (1992) Effect of PEEP on respiratory mechanics in anesthetized paralyzed humans. J Appl Physiol 73:1736–1742
Gattinoni L, Pesenti A, Avalli L, Rossi F, Bombino M (1987) Pressure-volume curve of total respiratory system in acute respiratory failure. Computed tomographic scan study. Am Rev Respir Dis 136:730–736
Gattinoni L, Pelosi P, Suter PM, Pedoto A, Vercesi P, Lissoni A (1998) Acute respiratory distress syndrome caused by pulmonary and extrapulmonary disease. Different syndromes? Am J Respir Crit Care Med 158:3–11
Vieira SR, Nieszkowska A, Lu Q, Elman M, Sartorius A, Rouby JJ (2005) Low spatial resolution computed tomography underestimates lung overinflation resulting from positive pressure ventilation. Crit Care Med 33:741–749
Mehta S, Stewart TE, MacDonald R, Hallett D, Banayan D, Lapinsky S, Slutsky A (2003) Temporal change, reproducibility, and interobserver variability in pressure-volume curves in adults with acute lung injury and acute respiratory distress syndrome. Crit Care Med 31:2118–2125
Nishida T, Suchodolski K, Schettino GP, Sedeek K, Takeuch M, Kacmarek RM (2004) Peak volume history and peak pressure-volume curve pressures independently affect the shape of the pressure-volume curve of the respiratory system. Crit Care Med 32:1358–1364
Pereira C, Bohe J, Rosselli S, Combourieu E, Pommier C, Perdrix JP, Richard JC, Badet M, Gaillard S, Philit F, Guerin C (2003) Sigmoidal equation for lung and chest wall volume-pressure curves in acute respiratory failure. J Appl Physiol 95:2064–2071
Rouby JJ, Puybasset L, Nieszkowska A, Lu Q (2003) Acute respiratory distress syndrome: lessons from computed tomography of the whole lung. Crit Care Med 31:S285–S295
Lu Q, Malbouisson LM, Mourgeon E, Goldstein I, Coriat P, Rouby JJ (2001) Assessment of PEEP-induced reopening of collapsed lung regions in acute lung injury: are one or three CT sections representative of the entire lung? Intensive Care Med 27:1504–1510
Pelosi P, Goldner M, McKibben A, Adams A, Eccher G, Caironi P, Losappio S, Gattinoni L, Marini JJ (2001) Recruitment and derecruitment during acute respiratory failure: an experimental study. Am J Respir Crit Care Med 164:122–130
Crotti S, Mascheroni D, Caironi P, Pelosi P, Ronzoni G, Mondino M, Marini JJ, Gattinoni L (2001) Recruitment and derecruitment during acute respiratory failure: a clinical study. Am J Respir Crit Care Med 164:131–140
Rimensberger PC, Cox PN, Frndova H, Bryan AC (1999) The open lung during small tidal volume ventilation: concepts of recruitment and “optimal” positive end-expiratory pressure. Crit Care Med 27:1946–1952
Jonson B, Richard JC, Straus C, Mancebo J, Lemaire F, Brochard L (1999) Pressure-volume curves and compliance in acute lung injury: evidence of recruitment above the lower inflection point. Am J Respir Crit Care Med 159:1172–1178
Maggiore SM, Jonson B, Richard JC, Jaber S, Lemaire F, Brochard L (2001) Alveolar Derecruitment at Decremental Positive End-Expiratory Pressure Levels in Acute Lung Injury. Comparison with the lower inflection point, oxygenation, and compliance. Am J Respir Crit Care Med 164:795–801
Halter JM, Steinberg JM, Schiller HJ, DaSilva M, Gatto LA, Landas S, Nieman GF (2003) Positive end-expiratory pressure after a recruitment maneuver prevents both alveolar collapse and recruitment/derecruitment. Am J Respir Crit Care Med 167:1620–1626
Steinberg JM, Schiller HJ, Halter JM, Gatto LA, Lee HM, Pavone LA, Nieman GF (2004) Alveolar instability causes early ventilator-induced lung injury independent of neutrophils. Am J Respir Crit Care Med 169:57–63
Malbouisson LM, Muller JC, Constantin JM, Lu Q, Puybasset L, Rouby JJ (2001) Computed tomography assessment of positive end-expiratory pressure-induced alveolar recruitment in patients with acute respiratory distress syndrome. Am J Respir Crit Care Med 163:1444–1450
Bugedo G, Bruhn A, Hernandez G, Rojas G, Varela C, Tapia JC, Castillo L (2003) Lung computed tomography during a lung recruitment maneuver in patients with acute lung injury. Intensive Care Med 29:218–225
Puybasset L, Gusman P, Muller JC, Cluzel P, Coriat P, Rouby JJ (2000) Regional distribution of gas and tissue in acute respiratory distress syndrome. III. Consequences for the effects of positive end-expiratory pressure. CT Scan ARDS Study Group. Adult Respiratory Distress Syndrome. Intensive Care Med 26:1215–1227
Dambrosio M, Roupie E, Mollet JJ, Anglade MC, Vasile N, Lemaire F, Brochard L (1997) Effects of positive end-expiratory pressure and different tidal volumes on alveolar recruitment and hyperinflation. Anesthesiology 87:495–503
Nieszkowska A, Lu Q, Vieira S, Elman M, Fetita C, Rouby JJ (2004) Incidence and regional distribution of lung overinflation during mechanical ventilation with positive end-expiratory pressure. Crit Care Med 32:1496–1503
Markhorst DG, van Genderingen HR, van Vught AJ (2004) Static pressure-volume curve characteristics are moderate estimators of optimal airway pressures in a mathematical model of (primary/pulmonary) acute respiratory distress syndrome. Intensive Care Med 30:2086–2093
Gattinoni L, Caironi P, Pelosi P, Goodman LR (2001) What has computed tomography taught us about the acute respiratory distress syndrome? Am J Respir Crit Care Med 164:1701–1711
Roupie E, Dambrosio M, Servillo G, Mentec H, el Atrous S, Beydon L, Brun-Buisson C, Lemaire F, Brochard L (1995) Titration of tidal volume and induced hypercapnia in acute respiratory distress syndrome. Am J Respir Crit Care Med 152:121–128
Schmitt JM, Vieillard-Baron A, Augarde R, Prin S, Page B, Jardin F (2001) Positive end-expiratory pressure titration in acute respiratory distress syndrome patients: impact on right ventricular outflow impedance evaluated by pulmonary artery Doppler flow velocity measurements. Crit Care Med 29:1154–1158
Bruhn A, Hernandez G, Bugedo G, Castillo L (2004) Effects of positive end-expiratory pressure on gastric mucosal perfusion in acute respiratory distress syndrome. Crit Care 8:R306–R311
Jonson B (2005) Elastic pressure-volume curves in acute lung injury and acute respiratory distress syndrome. Intensive Care Med 31:205–212
Hickling KG (1998) The pressure-volume curve is greatly modified by recruitment. A mathematical model of ARDS lungs. Am J Respir Crit Care Med 158:194–202
Richard JC, Maggiore SM, Jonson B, Mancebo J, Lemaire F, Brochard L (2001) Influence of tidal volume on alveolar recruitment. Respective role of PEEP and a recruitment maneuver. Am J Respir Crit Care Med 163:1609–1613
Brower RG, Lanken PN, MacIntyre N, Matthay MA, Morris A, Ancukiewicz M, Schoenfeld D, Thompson BT (2004) Higher versus lower positive end-expiratory pressures in patients with the acute respiratory distress syndrome. N Engl J Med 351:327–336
Holzapfel L, Robert D, Perrin F, Blanc PL, Palmier B, Guerin C (1983) Static pressure-volume curves and effect of positive end-expiratory pressure on gas exchange in adult respiratory distress syndrome. Crit Care Med 11:591–597
Takeuchi M, Goddon S, Dolhnikoff M, Shimaoka M, Hess D, Amato MB, Kacmarek RM (2002) Set positive end-expiratory pressure during protective ventilation affects lung injury. Anesthesiology 97:682–692
Acknowledgements
The authors thank all the nursing and technician personnel in the Intensive Care Unit and CT Ward of the Hospital Universitario Central de Asturias for their help. We also thank Ana Villagrá for her suggestions about the manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
This work was supported by a grant from Fondo de Investigación Sanitaria (PI03/0833) and Red GIRA (G03/063)
Rights and permissions
About this article
Cite this article
Albaiceta, G.M., Luyando, L.H., Parra, D. et al. Inspiratory vs. expiratory pressure-volume curves to set end-expiratory pressure in acute lung injury. Intensive Care Med 31, 1370–1378 (2005). https://doi.org/10.1007/s00134-005-2746-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-005-2746-6