Abstract
Objective
To test the following two hypotheses during weaning failure: (a) mixed venous oxygen saturation (SvO2) does not decrease in patients whose oxygen consumption does not increase, and (b) blood lactate may increase in patients who demonstrate substantial decreases in SvO2.
Design and setting
A prospective observational and physiological study in a 30-bed university intensive care unit.
Patients and participants
18 patients who failed weaning and 12 patients who succeeded weaning (controls).
Measurements and results
Hemodynamics, global tissue oxygenation, cardiovascular response (cardiac index/oxygen extraction diagram), and blood lactate were measured in ventilator-supported patients undergoing a spontaneous breathing trial. In patients who failed without having increased their oxygen consumption (n=9) the increase in oxygen delivery was accompanied by a decrease in oxygen extraction (by 15±4%). In patients who failed (n=9) having increased their oxygen consumption (by >10%) this increase was met mainly by an increase in oxygen extraction (by 30±7%). SvO2 increased by 2±1% in the former patients, whereas it decreased by 20±5% in the latter. Arterial lactate increased (range 2.3–3.1 mM/l) in only three patients who failed to have increased oxygen consumption and exhibited heart failure and the highest decreases in SvO2 (by 12–39%).
Conclusions
Patients whose SvO2 does not decrease during weaning failure do not have increased oxygen consumption probably due to respiratory center depression in some of them. Patients whose SvO2 decreases have increased oxygen consumption.
Similar content being viewed by others
Introduction
Discontinuation of ventilator support is difficult in about 20% of ventilated patients, presenting a great challenge for clinicians largely because the pathophysiological determinants of weaning failure are multiple, complex, and inadequately understood [1, 2]. To define the importance of hemodynamic performance and global tissue oxygenation in determining weaning outcome, mixed venous oxygen saturation (SvO2) was continuously recorded in ventilator-supported patients during a trial of spontaneous breathing [2]. On discontinuation from the ventilator SvO2 fell progressively in the patients who failed the trial (due to a combination of a relative decrease in oxygen delivery and an increase in oxygen extraction by the tissues) whereas it did not change in those patients who succeeded [2].
However, we have observed during monitoring of weaning trials that some patients fail to wean without having decreased SvO2. Although hemodynamics and tissue oxygenation of these patients have never been reported, one should expect that oxygen extraction does not increase. Theoretically this may occur with or without an increase in oxygen consumption during the failing weaning trial compared to the previous state of ventilator support. If oxygen consumption were increased, the only way that oxygen extraction would not increase would be a substantial and proportional increase in cardiac output and oxygen delivery. Nevertheless, it is well known that weaning can potentially place an excessive cardiovascular burden on the heart [1, 2, 3], but such a proportional increase in cardiac output is not expected. Moreover, based on exercise physiology and on the consideration of weaning as a kind of exercise [3], such a response is unlikely. This is because patients with overt heart failure have increased oxygen consumption during exercise by predominant increases in oxygen extraction, but healthy volunteers by combined increases in cardiac output and oxygen extraction [4, 5, 6]. Since increased oxygen extraction is always observed when oxygen consumption increases, we hypothesized that during weaning failure SvO2 does not decrease (i.e., oxygen extraction does not increase) in patients whose oxygen consumption does not increase.
During weaning failure the oxygen cost of breathing may increase to such an extent that the strenuously working respiratory muscles may “steal” oxygen and blood from other tissues [1, 7]. If cardiac output is limited, and the increase in oxygen consumption during weaning is not met by an increase in cardiac output and oxygen delivery, blood flow to regional tissue beds may be compromised [1], inducing severe tissue hypoperfusion and lactate production. Studies in animals [8] and humans during either acute respiratory failure [9] or weaning failure [10, 11] provide support in favor of this mechanism. However, to our knowledge, blood lactate levels have not been assessed during weaning. We hypothesized that during weaning failure blood lactate increases in patients who demonstrate substantial decreases in SvO2.
The aim of this study was to test the previous two hypotheses during weaning failure, i.e., (a) SvO2 does not decrease in patients whose oxygen consumption does not increase, and (b) blood lactate may increase in patients who demonstrate substantial decreases in SvO2. Therefore we evaluated weaning failure patients with variable SvO2 and oxygen consumption and assessed their cardiovascular responses and blood lactate. The results of this study have been presented in part in abstract form [12].
Methods
Patients
Thirty clinically stable patients who were intubated and mechanically ventilated for at least 48 h were prospectively studied (Table 1). Inclusion criteria for study entry were: (a) the underlying cause of acute respiratory failure had resolved and the primary physician had considered the patients ready to wean, and (b) presence of systemic and pulmonary artery (PA) catheters inserted as part of patient management. Patients with cardiac pacemakers were excluded. All consecutive patients fulfilling these criteria were included in the study. Fewer than 5% of patients in our intensive care unit have a PA catheter in place during weaning. This is due partly to the fact that our intensive care unit is a general one, and that patients in whom a PA catheter is an almost standard part of patient management (e.g., after cardiac surgery) are not usually admitted. Nearly all patients included in the present study had been several days on mechanical ventilation (MV) and had difficult weaning with repeatedly failing weaning trials (Table 1). The systemic and PA catheters were inserted by the patients’ physicians to support the weaning process. The appropriate institutional ethics committee approved the study, and informed written consent was obtained (see also ESM, part 1a).
Measurements
To obtain hemodynamic measurements the proximal and distal ports of the PA catheter and the systemic artery catheter were connected to strain-gauge manometers that provided continuous measurements of right atrial pressure, and pulmonary and systemic arterial pressures, respectively. The PA occlusion pressure (Ppao) and thermodilution cardiac output were determined. For gas exchange measurements blood samples were drawn from the arterial line and the distal port of the PA catheter. SvO2 was continuously recorded (Oximetrix 3). Calculations of hemodynamic [e.g., systemic vascular resistance (SVR)] and oxygenation [e.g., oxygen delivery (TO2)] variables were performed (see also ESM, parts 1b and 1c). Arterial blood lactate concentration was measured by the end-point enzymatic technique (normal values <2 mmol/l [13]; see also ESM, part 1b).
Protocol
Patients were placed in semirecumbent position and were ventilated in the assist-control mode. Patients then underwent a spontaneous breathing trial (subsequently called trial) via a T-piece circuit. Trials lasted for 2 h unless the patient met the a priori defined criteria of weaning failure at an earlier point of time [2, 14, 15] (see ESM for the criteria, part 1d). Patients who met these criteria during the 2-h trial were returned to MV and were designated as the weaning failure group. Patients successfully completing the trials were extubated; patients who sustained spontaneous breathing for more than 24 h were designated the weaning success group [16] and served as controls. During the trial 18 patients met the criteria of weaning failure after 59±6 min and were returned to MV; 12 patients successfully completed the trial and were extubated after 115±2 min, without presenting signs of respiratory distress during the next 24 h.
Measurements were performed during MV, immediately before disconnection from the ventilator (MV), and at 5 min (Start), 1 h, and 2 h (End) after the beginning of the trial; if the patient met the criteria of weaning failure before the end of the 2-h trial, measurements were made during the last minute of the trial (End). Arterial lactate was also measured 2 h after extubation or resumption of MV in patients who succeeded or failed weaning, respectively.
Data analysis
Cardiovascular response to weaning was evaluated by interpreting the relationship between cardiac index (CI) and oxygen extraction ratio (O2ER) during the spontaneous breathing trials. In patients whose oxygen consumption (VO2) increased a higher relative increase in O2ER than in CI on a CI/O2ER diagram was considered as indicative of the presence of heart failure, whereas an equal or a lower relative increase in O2ER than in CI was considered as response indicative of sufficiently preserved cardiac function [5, 17]. Since the errors in calculating VO2 from Fick’s equation (which was used in this study) are between 5% and 10% [18], we considered that increases in VO2 greater than 10% at the end of the trial compared with MV would represent true increases in VO2 [19].
Continuous SvO2 measurements were analyzed [2]. Two-way analysis of variance followed by Tukey’s “honestly significantly different” test for post-hoc comparisons, t test, Fisher’s exact test, and Pearson’s test were used as needed. Values are means ±SE (see also ESM, part 1e).
Results
The results of patients who succeeded weaning and their comparison with the results of patients who failed are included in the ESM, part 2. Patients who failed were divided into two groups according to VO2 responses during the trial: those in whom VO2 increased by 10% or less, remained unchanged, or decreased at the end of the trial compared to MV (“failure-noVO2 increase group”), and those patients in whom VO2 increased by more than 10% at the end of the trial compared to MV (“failure-VO2 increase group”). Nine patients were included in each group (Table 1).
Respiratory variables
Maximum inspiratory pressure was similar in the failure-noVO2 increase group and the failure-VO2 increase group (33.9±5.3 vs. 33.1±3.6, p=0.9). During the trial breath components were similar in the two groups except minute ventilation, which was lower in the failure-noVO2 increase group than in the failure-VO2 increase group (Table 2; see also ESM, part 2a).
Mixed venous oxygen saturation
Whereas SvO2 was not significantly different between the failure-noVO2 increase group and the failure-VO2 increase group during MV, during the trial SvO2 did not change in the failure-noVO2 increase group whereas it decreased in the failure-VO2 increase group (Table 2). At the end of the trial SvO2 had increased by 2±1% in the failure-noVO2 increase group but decreased by 20±5% in the failure-VO2 increase group (p=0.001). In every patient of the failure-noVO2 increase group SvO2 had either increased, remained unchanged, or decreased more than 5% at the end of the trial compared to MV, whereas in every patient of the failure-VO2 increase group SvO2 decreased by at least 5% (see ESM, part 2b, for data on gas exchange).
Cardiovascular response and tissue oxygenation
The interrelationships between VO2, TO2, and O2ER are demonstrated in Fig. 1. Cardiovascular response and tissue oxygenation during weaning in patients who failed (all patients lumped together) and those who succeeded were similar, i.e., the increase in VO2 was met by (insignificant) increases in both TO2 and O2ER (Fig. 1A).
Relationships between oxygen delivery and oxygen consumption in patients who failed (all patients combined; open circles) and patients who succeeded weaning (closed circles, A), and in the subgroups of patients who failed, i.e., the failure-noVO2 increase group (open squares) and the failure-VO2 increase group (open triangles, B). Beginning and end of arrows Mean values during mechanical ventilation and at the end of the spontaneous breathing trial, respectively. The linear relationships represent isopleths of oxygen extraction ratio. See text for interpretation
Cardiovascular and tissue oxygenation responses in the subgroups of patients who failed were different (Fig. 1B, Table 2). In the failure-noVO2 increase group the increase in TO2 was accompanied by a decrease in O2ER (by 15±4%), whereas in the failure-VO2 increase group the increase in VO2 was met mainly by an increase in O2ER (by 30±7%; p<0.0001 vs. failure-noVO2 increase group). The CI/O2ER ratio, an index of adequate compensation by both central and peripheral compensatory mechanisms [20], increased in the failure-noVO2 increase group during the trial but did not change in the failure-VO2 increase group (p=0.01; two-way analysis of variance).
In all patients of the failure-noVO2 increase group the cardiovascular response to weaning should be considered as compatible with adequately preserved cardiac function (Fig. 2A). In the failure-VO2 increase group four patients (nos. 22, 23, 25, 29) with a history of heart disease had cardiovascular response indicative of the presence of heart failure, i.e., a higher relative increase in O2ER than in CI (Fig. 2B). The other patients had cardiovascular response compatible with sufficiently preserved cardiac function (see also ESM, part 2d).
Relationship between oxygen extraction ratio and cardiac index in the subgroups of patients who failed, i.e., the failure-noVO2 increase group (open squares, A) and the failure-VO2 increase group (open triangles, B). Beginning and end of arrows Individual data of each patient during mechanical ventilation and at the end of the spontaneous breathing trial, respectively. Numbers correspond to individual patient number in Table 1. Line starting from the origin of the cardiac index/oxygen extraction diagram and meeting the normal values of cardiac index and oxygen extraction of 3 l/min per m2 and 25%, respectively, was extrapolated to represent a line of reference [17], i.e., the line where patients raising their oxygen consumption by equal increases in both cardiac index and oxygen extraction would fall. The curvilinear relationships represent isopleths of constant oxygen consumption for a given hemoglobin value. See text for interpretation
Arterial blood lactate
Lactate levels did not change in the failure-noVO2 increase group during the trial compared to MV, whereas lactate increased in the failure-VO2 increase group at the end of the trial (Table 2). Nevertheless, substantial lactate increases (>2 mmol/l) at the end of the trial were detected in only three patients of the failure-VO2 increase group (nos. 23, 25, 29; Fig. 3). Two hours after resumption of MV in patients who failed arterial lactate had decreased (p=0.008) and had returned to levels similar to those observed during MV (see also ESM, part 2e).
Arterial lactate levels during mechanical ventilation, at the end (last minute) of the spontaneous breathing trial, and 2 h after the trial in patients who succeeded (A) and patients who failed (altogether) weaning (B). Closed circles Measurements in patients who succeeded; open squares measurements in patients of the failure-noVO2 increase group; open triangles measurements in patients of the failure-VO2 increase group; small horizontal solid lines mean values; horizontal dotted lines arterial lactate upper normal limit (2 mmol/l). See text for interpretation
Hemodynamics
Except for Ppao, which was higher in the failure-VO2 increase group than in the failure-noVO2 increase group during the trial, hemodynamic variables were not significantly different between the two groups (Table 2). The four patients in the failure-VO2 increase group (nos 22, 23, 25, 29), who exhibited the highest decreases in SvO2 (range 12–39%) and increases in O2ER (range 6–16%) at the end of the trial compared to MV, and also demonstrated on the CI/O2ER diagram a cardiovascular response indicative of the presence of heart failure, had a Ppao amounting to 14–17 mmHg during MV that increased to 22–28 mmHg at the end of the trial.
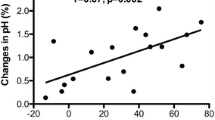
In the failure-noVO2 increase group the difference between the values at the end of the trial with those during MV in PaCO2 (ΔPaCO2) was positively related to ΔTO2 (r=0.81, p<0.01; Fig. 4A) and ΔCI (r=0.83, p<0.01), and inversely related to ΔSVR (r=−0.83, p<0.01). On the other hand, in the failure-VO2 increase group, ΔPaCO2 was inversely related to ΔTO2 (r=−0.83, p<0.01; Fig. 4B).
Discussion
The principal findings of this study were: (a) in the failure-noVO2 increase group the increase in TO2 was accompanied by a decrease in O2ER, whereas in the failure-VO2 increase group the increase in VO2 was met mainly by an increase in O2ER, (b) SvO2 did not decrease in the failure-noVO2 increase group, whereas SvO2 decreased in the failure-VO2 increase group, and (c) lactate increases were detected in a minority of the failure-VO2 increase group who exhibited the highest decreases in SvO2 and demonstrated on the CI/O2ER diagram a cardiovascular response indicative of the presence of heart failure.
The present study emphasizes the variability in circulatory and global tissue oxygenation responses in weaning failure, demonstrating for the first time that several patients (those who do not exhibit substantial increases in VO2) fail to wean without having decreased SvO2 or increased O2ER while others (as previously reported [2]) have decreased SvO2 and increased O2ER. This study clarifies that among the latter some have cardiovascular response to weaning indicative of the presence of heart failure whereas others have a response compatible with sufficiently preserved cardiac function. The present study also shows for the first time that patients with a cardiovascular response compatible with heart failure and demonstrating the highest SvO2 decreases exhibit hyperlactatemia (blood lactate 2–5 mmol/l [13]).
Oxygen consumption
The increase in VO2 during the trial in the failure-VO2 increase group, expressing the oxygen cost of transition from assist-control MV to spontaneous breathing (oxygen cost of breathing), represented 25% of the VO2 at the end of the trial and was due mainly to respiratory muscle recruitment [21]. The hypercapnia observed was accompanied by strong respiratory muscle activation and respiratory distress during the failing trial. The inverse relationship between the increase in PaCO2 and TO2 (Fig. 4B) suggests that hypercapnia was probably the result of inadequate oxygen delivery to the strenuously working respiratory muscles leading to hypoventilation. Similar results (i.e., increased oxygen cost of breathing, averaging 24–27% of VO2), have been reported in patients who fail to wean [21, 22].
From a first consideration, unchanged VO2 during the spontaneous breathing trial in the failure-noVO2 increase group suggests that patients of this group failed to wean without having significantly augmented respiratory muscle activity. Similar results have been reported previously, where patients failed to wean without having increased VO2 [2, 21, 23]. Indeed, a small percentage of patients fail to wean without having increased inspiratory muscle load, suggesting depression of the respiratory control system [14, 24]. Another potential explanation of the lack of increase in VO2 is some stress or asynchrony related to MV that is alleviated by weaning [19]. Moreover, calculation of VO2 from Fick’s equation is associated with errors up to 10% [18]. Therefore although increases in the measured VO2 of more than 10% at the end of the weaning trial should represent true increases in VO2 [19], increases of 10% or less or even small decreases in the measured VO2 may represent errors in measurement despite small true increases in VO2. The change in the measured VO2 during the weaning trial is not sensitive enough to detect small increases in respiratory muscle activity, and some patients of the failure-noVO2 increase group may actually have had respiratory muscle recruitment that could not be detected by VO2. Nevertheless, investigation of the exact cause of weaning failure by measuring respiratory muscle/center activity was beyond the aim of the present study. It should be emphasized that calculation of VO2 from Fick’s equation during weaning has notable advantages over the other two methods of measuring VO2 from respiratory gases. The first method, collecting expired gas in a Douglas bag, is unreliable when inspired oxygen fraction is equal to or higher than 0.4 [22], and in some of our patients this fraction is 0.4–0.6; the second method, measuring inspired and expired gases with a metabolic monitor (indirect calorimetry), is quite inaccurate since changes in ventilation during weaning alter CO2 stores and prevent the maintenance of a steady state [19].
Cardiovascular response
In the failure-noVO2 increase group the increase in CI resulted in decreased O2ER. The increase in CI was probably due in part to the increase in PaCO2 through its effect on reducing SVR, as suggested by the relationship between the increase in CI (or TO2; Fig. 4A) and PaCO2, and the inverse relationship between the increase in PaCO2 and SVR. Indeed, the main effect of acute hypercapnia on the cardiovascular system is an increment in cardiac output because of vasodilation and tachycardia [25, 26]. In addition to a theoretical, direct negative inotropic effect of hypercapnia [26], the combined effects of acute hypercapnia on heart rate, SVR, and contractility result in a net increment in cardiac output in the absence of significant cardiac disease [25, 26]. Therefore the adequate increase in CI of the failure-noVO2 increase group in response to acute hypercapnia is indicative of sufficiently preserved cardiac function during weaning failure in this group. However, since VO2 did not increase, the presence of occult heart failure cannot be totally excluded.
Clinical implications
The various cardiovascular responses detected in patients who fail to wean suggest different therapeutic approaches to improve weaning outcome. In the failure-VO2 increase group patients (detected by SvO2 decreases of 5% or greater) who have increased work of breathing measures to reduce it in a subsequent trial by treating reversible causes [1] seem reasonable. In the subgroup of patients exhibiting heart failure treatment with vasodilators or inotropic agents could help by decreasing Ppao and/or increasing cardiac output. This averts tissue hypoxia during weaning. In contrast, among the failure-noVO2 increase group patients (detected by SvO2, which either increases, remains unchanged, or decreases by less than 5%), some patients exhibit hypoventilation associated with possible respiratory center depression; reasons potentially responsible for this depression [1, 24] should be sought and treated.
References
Vassilakopoulos T, Zakynthinos S, Roussos C (1996) Respiratory muscles and weaning failure. Eur Respir J 9:2383–2400
Jubran A, Mathru M, Dries D, Tobin M (1998) Continuous recordings of mixed venous oxygen saturation during weaning from mechanical ventilation and the ramifications thereof. Am J Respir Crit Care Med 158:1763–1769
Pinsky MR (2000) Breathing as exercise: the cardiovascular response to weaning from mechanical ventilation. Intensive Care Med 26:1164–1166
Sutton JR, Reeves JT, Wagner PD, Groves BM, Cymerman A, Malconian MK, Rock PB, Young PM, Walter SD, Houston CS (1988) Operation Everest II: oxygen transport during exercise at extreme simulated altitude. J Appl Physiol 64:1309–1321
Weber KT, Janicki JS, McElroy PA, Reddy HK (1988) Concepts and applications of cardiopulmonary exercise testing. Chest 93:843–847
Herrlin B, Sylven C (1991) Increased arterial oxygen content-an important compensatory mechanism in chronic moderate heart failure. Cardiovasc Res 25:384–390
Magder S, Erian R, Roussos C (1986) Respiratory muscle blood flow in oleic acid-induced pulmonary edema. J Appl Physiol 6:1849–1856
Viires N, Sillye G, Aubier M, Rassidakis A, Roussos C (1983) Regional blood flow distribution in dogs during induced hypotention and low cardiac output: spontaneous breathing versus artificial ventilation. J Clin Invest 72:935–947
Gil A, Carrizosa F, Herrero A, Martin J, Gonzalez J, Jareno A, Rivero J (1998) Influence of mechanical ventilation on blood lactate in patients with acute respiratory failure. Intensive Care Med 24:924–930
Mohsenifar Z, Hay A, Hay J, Lewis MI, Koerner SK (1993) Gastric intramural pH as a predictor of success or failure in weaning patients from mechanical ventilation. Ann Intern Med 119:794–798
Bouachour G, Guiraud MP, Gouello JP, Roy PM, Alquier P (1996) Gastric intramucosal pH: an indicator of weaning outcome from mechanical ventilation in COPD patients. Eur Respir J 9:1868–1873
Routsi C, Zakynthinos S, Kaltsas P, Metafa M, Kazi D, Gonis A, Sotiropoulou C, Roussos C (1999) Lactate elevation during weaning trials from mechanical ventilation (abstract). Am J Respir Crit Care Med 159:A371
Mizock BA, Falk JL (1992) Lactic acidosis in critical illness. Crit Care Med 20:80–93
Jubran A, Tobin M (1997) Pathophysiologic basis of acute respiratory distress in patients who fail a trial of weaning from mechanical ventilation. Am J Respir Crit Care Med 155:906–915
Esteban Α, Frutos F, Tobin ΜJ, Alia I, Solsona JF, Valverdu I, Fernandez R, De La Cal A, Benito S, Tomas R, Carriedo D, Macias S, Blanco J (1995) Α comparison of four methods of weaning patients from mechanical ventilation. Ν Engl J Med 332:345–350
Yang KL, Tobin MJ (1991) A prospective study of indexes predicting the outcome of trials of weaning from mechanical ventilation. Ν Engl J Med 324:1445–1450
Silance P-G, Simon C, Vincent JL (1994) The relation between cardiac index and oxygen extraction in acutely ill patients. Chest 105:1190–1197
De Backer D, Moraine JJ, Berre J, Kahn RJ, Vincent JL (1994) Effects of dobutamine on oxygen consumption in septic patients: direct vs indirect determinations. Am J Respir Crit Care Med 150:95–100
De Backer D, El Haddad P, Preiser JC, Vincent JL (2000) Hemodynamic responses to successful weaning from mechanical ventilation after cardiovascular surgery. Intensive Care Med 26:1201–1206
Yalavatti GS, De Backer D, Vincent JL (2000) Assessment of cardiac index in anemic patients. Chest 118:782–787
Field S, Kelly SM, Macklem ΡΤ (1982) The oxygen cost of breathing in patients with cardiorespiratory disease. Am Rev Respir Dis 126:9–13
Brochard L, Hart Α, Lorino Η, Lemaire F (1989) Inspiratory pressure support prevents diaphragmatic fatigue during weaning from mechanical ventilation. Am Rev Respir Dis 139:513–521
Berry PR, Pontoppidan H (1968) Oxygen consumption and blood gas exchange during controlled and spontaneous ventilation in patients with respiratory failure. Anesthesiology 29:177–178
Marini JJ (1986) The physiologic determinants of ventilator dependence. Respir Care 31:271–282
Mas A, Saura P, Joseph D, Blanch L, Baigorri F, Artigas A, Fernandez R (2000) Effects of acute moderate changes in PaCO2 on global hemodynamics and gastric perfusion. Crit Care Med 28:360–365
Feihl F, Perret C (1994) Permissive hypercapnia: how permissive should we be? Am J Respir Crit Care Med 150:1722–1737
Conflict of interest:
No information supplied
Author information
Authors and Affiliations
Corresponding author
Additional information
This article refers to the editorial available at http://dx.doi.org/10.1007/s00134-005-2698-x
Electronic Supplementary Material
Rights and permissions
About this article
Cite this article
Zakynthinos, S., Routsi, C., Vassilakopoulos, T. et al. Differential cardiovascular responses during weaning failure: effects on tissue oxygenation and lactate. Intensive Care Med 31, 1634–1642 (2005). https://doi.org/10.1007/s00134-005-2699-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-005-2699-9