Abstract
Objective
Heat shock protein 70 (HSP-70) is protective against cellular and tissue injury. Increased serum HSP-70 levels are associated with decreased mortality in trauma patients. Glutamine (Gln) administration increases serum and tissue HSP-70 expression in experimental models of sepsis. Gln has been safely administered to critically ill patients and can improve clinical outcomes, but the effect of Gln administration on HSP-70 expression in humans is unknown. We examined whether Gln-supplemented parenteral nutrition (PN) increases serum HSP-70 levels in critically ill patients.
Design and setting
Randomized, controlled, double-blind study in surgical intensive care units (SICU) in a university hospital.
Patients
29 patients admitted to the SICU and requiring PN for more than 7 days.
Interventions
Patients received either Gln-PN (containing alanyl-glutamine dipeptide; 0.5 g/kg per day; n=15) or standard Gln-free PN (control-PN) that was iso-nitrogenous to Gln-PN (n=14). Serum HSP-70 concentrations were measured at enrollment and at 7 days. Clinical outcome measures were also determined.
Results
HSP-70 concentrations were unchanged in control-PN subjects from baseline to day 7. In marked contrast, Gln-PN subjects demonstrated significantly higher (3.7-fold) serum HSP-70 concentrations than control subjects. In Gln-PN patients there was a significant correlation between increases in HSP-70 levels over baseline and decrease in ICU length of stay.
Conclusions
Gln-PN significantly increases serum HSP-70 in critically ill patients. The magnitude of HSP-70 enhancement in Gln-treated patients was correlated with improved clinical outcomes. These data indicate the need for larger, randomized trials of the Gln effect on serum and tissue HSP-70 expression in critical illness and relationship to clinical outcomes.
Similar content being viewed by others
Introduction
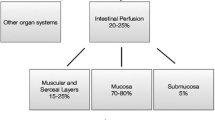
It has long been recognized that enhanced expression of heat shock protein 70 (HSP-70) protects proteins from damage, allows restoration of function to damaged proteins, and prevents cellular injury and death [1, 2, 3, 4, 5]. Further, enhanced expression of HSP-70 in experimental models of sepsis, shock, and critical illness attenuates the proinflammatory response, reduces organ injury, and improves survival [5]. Of note, recent data demonstrate that cellular levels of HSP-70 are markedly decreased in clinical sepsis in critically ill patients [6, 7]. Further, clinical data have revealed that serum HSP-70 concentrations measured early after severe trauma are positively correlated with increased survival [8]. However, laboratory enhancers of HSP-70, including sublethal heating, sodium arsenite, and adenoviral transfection, are not practical for clinical administration.
A number of studies have shown that parenteral administration of the amino acid glutamine (Gln) as a component of nutrition support is safe and improves clinical outcomes in critically ill patients [9, 10, 11, 12]. In addition, we have shown that Gln markedly enhances cell survival against a variety of stressful stimuli by a mechanism involving enhanced HSP-70 expression [13, 14]. Further, we have shown that administration of intravenous Gln upregulates HSP-70 expression in multiple organs in a rat model of endotoxemia [15] and significantly improves survival. We have also shown that parenteral Gln enhances HSP-70 in the serum of rodents following polymicrobial sepsis induced by cecal/ligature puncture, and that this response is associated with decreased mortality in this model [16]. Thus administration of intravenous Gln may be a practical method to increase HSP-70 in the circulation and tissues of critically ill patients. Further, the protective effects of this HSP-70 may represent a mechanism for the improved clinical outcomes observed with Gln administration in certain groups of critically ill patients [17].
The aims of the current studies were: (a) to examine whether intravenously administered Gln, as a component of parenteral nutrition (PN) support increases serum HSP-70 levels in critically ill adults admitted to a surgical intensive care unit and (b) to determine the relationship between serum HSP-70 responses and important clinical outcomes in these individuals.
Methods
This clinical trial was approved by the Institutional Review Board of Emory University, Atlanta, Georga, USA, and all patients or their legal representative provided informed consent. The data reported here are derived from a subgroup of adult subjects participating in a double-blind, randomized study of Gln dipeptide-supplemented PN in postoperative patients requiring admission to a surgical intensive care unit (SICU) necessitating PN at Emory University Hospital (EUH), Atlanta. Subjects were selected based on the availability of serum for analysis for HSP-70. In approximately one-half of the subjects (selected randomly and in a blinded fashion) additional serum was drawn for analysis of HSP-70. The randomization of patients was concealed and double-blinded in nature. All data for HSP-70 expression were analyzed in a blinded fashion. Serum for HSP-70 concentrations was obtained at entry and 7 days after initiation of either Gln-supplemented PN or standard Gln-free PN in 29 patients with a history of necrotizing pancreatitis requiring surgical débridment or colonic, cardiac, or vascular surgery.
Eligible subjects were those admitted to the EUH SICUs. Inclusion criteria were: (a) signed informed consent, (b) age 18–80 years, (c) SICU care required after pancreatic, coronary artery bypass grafting (CABG), cardiac valve, nonneurological vascular, or colonic surgery, (d) subject deemed by primary physicians and the EUH Nutrition and Metabolic Support Service likely to require PN for more than 7 days at entry, (e) subject without evidence of acute, uncontrolled infection or history of clinical sepsis in previous 24 h, and (f) no evidence of active malignancy, significant hepatic dysfunction (total bilirubin >4.0 mg/dl or more than fivefold elevation in serum transaminase concentrations), or significant renal dysfunction (evolving acute renal failure or on dialysis). Exclusion criteria were: (a) study PN not given for 5 or more consecutive days after initiation and (b) evidence of developing hepatic failure. The subjects were block-randomized by the EUH research pharmacist on the basis of type of operation to: (a) the control group, whose subjects received standard, Gln-free PN (STD-PN) and (b) the experimental group, whose subjects received isocaloric, isonitrogenous, Gln dipeptide-supplemented PN (Gln-PN). Patients were required to receive Gln-supplemented or control PN for at least 7 days to be included in data analysis.
The control PN amino acid (AA) formula was a standard, Gln-free AA solution (15% Clinisol, Baxter, Deerfield, Ill., USA), given at a daily dose of 1.5 g/kg. The Gln group received PN containing 0.5 g/kg per day l-alanyl-l-Gln dipeptide (Dipeptiven, 20% alanyl-Gln dipeptide solution; Fresenius-Kabi, Bad Homburg, Germany) added to 1.0 g/kg per day 15% Clinisol AA solution (total 1.5 g/kg per day). This dose of l-alanyl-l-Gln dipeptide provides 23 g l-Gln daily for a 70 kg subject (two-thirds of AG is the Gln moiety). The feeding goals were total daily calorie intake of 1.3 ×basal energy expenditure (predicted by the Harris-Benedict equation) from PN plus enteral intake, as tolerated, and total daily amino acid/protein intake of 1.5 mg/kg. PN dextrose comprised 70% of PN non-AA kilocalories, and intravenous fat emulsion (20% Intralipid, Kabi) comprised 30% of PN non-AA kilocalories. Blood for serum creatinine and bilirubin levels was drawn at enrollment and several times weekly throughout study period and the maximal weekly value determined. After enrollment blood was also drawn in the morning between 0800 and 1000 hours for baseline plasma Gln levels, C-reactive protein (CRP), and HSP-70 concentrations to assess extent of systemic inflammation and the HSP-70 response to Gln dipeptide-supplemented PN. These determinations were repeated at 7 days after entry. Plasma Gln levels were obtained using standard methods with a Beckman amino acid analyzer at Emory University. CRP concentrations were determined by the EUH Laboratory using standard methods. Serum HSP-70 analyses were performed by a specific enzyme-linked immunosorbent assay kit method (EKS 700, Stressgen, Victoria, B.C., Canada). All samples were analyzed in duplicate. Clinical outcome variables (hospital and ICU length of stay, LOS, and days on mechanical ventilation) were determined in a blinded fashion from day 1 of study until hospital discharge.
In the 29 subjects for whom additional serum was obtained for HSP-70 analysis all patients completed more then 7 days of parenteral nutrition. Thus this analysis included all eligible patients and is an intention-to-treat analysis. Baseline characteristics of study participants are shown in Table 1; the baseline characteristics of the study group as a whole (n=59 patients) are also included in Table 1. As can be observed from the data, the selected subgroup for whom serum for HSP-70 was available was very similar in all respects to the entire study group. The only difference is that that the subgroup of patients in whom serum HSP-70 was evaluated were slightly younger then the averages of the entire study group (see Table 1). The Gln-PN and control-PN groups were well matched at study entry with respect to age, baseline inflammation state (serum CRP concentration), body mass index, and hospital day at entry to study. There were also no significant differences in type of surgery between groups. Perhaps, most importantly, the APACHE II scores between the Gln-PN and control-PN subgroups were nearly identical, and this was also true when these two subgroups were compared to the entire study group of 59 patients. Nutritional intake information for the two subgroups is included in Table 2. Information for the entire study groups is also included. There were no differences with regard to the average number of days PN was provided, intravenous total and protein calories, or enteral intake. Although Gln-PN patients in the studied subgroup received fewer enteral calories, this difference was not statistically significant from the control-PN subgroup. There were no significant differences between the studied subgroups and the entire study population of 59 patients. However, in the studied subgroup there was a trend towards the Gln-PN subgroup receiving fewer enteral calories the entire Gln group. Plasma Gln concentrations were measured at initiation of the study and at day 7 posttreatment.
Unless otherwise specified, data are presented as arithmetic means and standard deviations or as arithmetic means and 95% confidence intervals (95% CI) for continuous variables and as percentage of participants for categorical variables. Serum HSP-70 levels were highly skewed and exhibited a mean-variance relationship on the original scale. The distribution of HSP-70 was more symmetric on a logarithmic scale and log-transformation stabilized the variance across groups and time, and thus the log-transformed HSP-70 values were used in the analysis, and data are presented as geometric means with 95% CIs on the original scale. Change in HSP-70 concentrations from baseline to day 7 on the logarithmic scale is interpreted as the proportional change on the original scale. Serum HSP-70 levels, proportional change in HSP-70 levels, and clinical outcomes were compared between Gln and control subjects using independent samples t tests for continuous data (log transformed data for HSP-70) and Pearson’s χ2 tests for categorical data. The independent-samples t test applied to log-transformed data is used to compare the ratio of geometric means. Spearman’s rank correlation coefficients were used to examine the association between clinical outcome measures and HSP-70. The level of statistical significance was set at α=0.05. Statistical analyses were performed using SPSS release 12.0 for Windows (SPSS, Chicago, Ill., USA).
Results
A significant increase in Gln concentration was noted in the Gln-PN group 7 days after treatment (Fig. 1). No adverse events deemed related to administration of Gln dipeptide occurred. The geometric mean serum HSP-70 levels for study participants are shown in Table 3 and are also displayed in Fig. 2. Blood HSP-70 concentrations were similar in the two groups at baseline, but after 7 days the HSP-70 levels were 3.7-fold higher (95% CI 1.2–11.9, p=0.029) in patients receiving Gln than in patients receiving placebo. This was due to a 3.4-fold greater proportional increase (ratio of geometric means 3.4, 95% CI 1.5–7.7, p=0.005) in serum HSP-70 in patients receiving Gln compared to placebo. Further, circulating HSP-70 concentrations increased 6.9-fold (95% CI 3.5–13.7) in patients receiving Gln compared to a 2.0fold increase (95% CI 1.2–2.4) in patients receiving placebo.
There were no significant differences in hospital or SICU LOS or ventilator days or maximal serum total bilirubin or creatinine levels between patients treated with Gln in PN and control PN participants (Table 4). However, changes in HSP-70 concentration from baseline to day 7 of study were significantly associated with these clinical outcome measures in patients receiving Gln dipepetide-supplemented PN (Table 5). The strongest correlations were observed for the relative percent change in HSP-70. Greater relative increases in HSP-70 concentrations were significantly associated with fewer ICU days (Spearman’s ρ=−0.649, p=0.009) and fewer ventilator days (Spearman’s ρ=−0.551, p=0.033). The relationship between the number of ICU days and relative increase in HSP-70 is displayed in Fig. 3 for Gln and control subjects. Greater relative increases in HSP-70 were significantly associated with fewer ICU days for Gln subjects (Spearman’s ρ=−0.649, p=0.009) but not for control subjects (Spearman’s ρ=0.418, p=0.155). Trends were observed for absolute changes in HSP-70 expression being correlated with renal function, as defined by maximum measured creatinine concentration (Spearman’s ρ=−0.476, p=0.07). No significant correlations were noted between HSP-70 levels and outcome in the control-PN treated group (Table 5).
Discussion
These results are, to our knowledge, the first demonstration that parenteral Gln administration upregulates serum HSP-70 concentrations in humans. Specifically, we show that 7 days of Gln administration increased serum HSP-70 levels compared to responses in clinically matched subjects requiring SICU care and receiving a PN formulation that was iso-nitrogenous and isocaloric. These results reveal that parenteral Gln can enhance not only mean serum HSP-70 levels after 7 days, but also the change in serum HSP-70 from baseline vs. control subjects receiving standard, Gln-free PN. In addition, our results show that in patients receiving Gln, the increase in serum HSP-70 over baseline was correlated with a decrease in ICU length of stay and days on the ventilator. A trend towards a decrease in the maximum serum creatinine concentration was also seen in patients receiving Gln when correlated with the absolute increase in HSP-70 over baseline. Although this was a small study, these initial pilot data show promise for Gln being the first clinically relevant enhancer of HSP-70 in critical illness.
The physiological role of serum HSP-70 has yet to be determined. However, the significance of serum HSP-70 expression has been examined in a number of settings. Data in severely traumatized patients reveal a direct correlation between serum HSP-70 levels at hospital admission and survival to discharge. That study demonstrated that serum HSP-70 levels are independent of the severity of injury. Patients presenting with an Injury Severity Score higher than 16 and a low HSP-70 level at admission had a mortality rate twice as high as historical controls of similar ages [8]. In addition, no deaths occurred in patients with serum HSP-70 levels greater then 15 ng/ml. The average HSP-70 level at presentation in our patients were lower than in the previous study [8] and not different between Gln treated and the control patients. Differences in clinical condition (i.e., acute trauma vs. postoperative critical illness), illness severity, hospital LOS prior to entry, nutrient intake, assay employed or other factors may be responsible for the differences in HSP-70 levels between the earlier study and the current trial. Our observation that PN supplemented with Gln markedly increases serum HSP-70 levels in SICU patients studied an average of 14 days after hospital admission raises the question of whether Gln administration has a similar effect if given acutely at presentation to the emergency room or intensive care unit.
The origin of serum HSP-70 is being widely debated. Traditionally HSP-70 has been believed to be released from necrotic cells and not apoptotic cells [18]. However, recent data indicate that HSP-70 can be secreted from viable cells as a number of cell types have been shown to release HSP-70 [19, 20, 21]. The answer to this question remains unclear. The precise function of serum HSP-70 is also unclear. Recent in vitro studies have suggested that extracellular HSP-70 activates the immune system and signal through a CD-14 [22] and toll-like receptors 2 and 4 [23] dependent pathway to induce the release of proinflammatory cytokines. However, some investigators have expressed concern that these in vitro effects may be due to lipopolysaccharide contamination of the recombinant HSP-70 preparations, as lipopolysaccharide and HSP each signal through toll-like receptor 4 [24, 25]. An alternative view is that extracellular HSP-70 stimulates an anti-inflammatory Th2 response and induces Cd4+ T-cells releasing anti-inflammatory cytokines such as interleukin (IL) 10 [18]. This is supported by a study of serum HSP-70 levels in CABG vs. patients studied “off-pump,” in which the off-pump patients who had lower levels of serum HSP-70 had a higher levels of IL-6, a proinflammatory cytokine. More importantly, “on-pump” CABG patients who had the highest serum HSP-70 concentrations also had increased blood concentrations of IL-10, whereas the “off-pump” patients who had low concentrations of HSP-70 and no increase in IL-10 release [26]. Given these data, it appears that HSP-70 may be part of an immunoregulatory response that potentially downregulates the inflammatory response.
The dose of Gln dipeptide utilized in this trial was based on results of previous safety and efficacy studies of Gln-supplemented PN [9, 20, 11, 12]. The Gln-PN group received a lower dose of essential amino acids than the control-PN group did. No data regarding essential amino acid intake effecting serum HSP-70 response are currently available. Recent studies have indicated that parenteral and enteral Gln can improve clinical outcomes when administered to certain critically ill and injured patients [9, 11, 12, 27, 28]. However, the mechanism of this benefit is not yet understood [17]. It is possible that Gln-mediated enhancement of HSP-70 expression is an important mechanism of the Gln protective effects. This is supported by data from our laboratory indicating that Gln can protect gut epithelial cells against injury [13]. This protection is lost if HSP-70 expression is inhibited either by quercetin (an inhibitor of HSP-70 expression) or by specific antisense inhibition of the HSP-70 gene [13, 14]. Further, we have data in the cecal/ligature puncture model of polymicrobial sepsis that Gln induces pulmonary and serum HSP-70 and prevents mortality from sepsis [29]. This survival benefit is lost if Gln-mediated increases in HSP-70 are blocked by preadministration of quercetin [29].
In summary, these data indicate that PN supplemented with alanyl-Gln dipeptide at a daily dose of 0.5 mg/kg can increase serum concentrations of HSP-70 after 7 days in critically ill patients. This is the first demonstration of a safe, nontoxic enhancer of serum HSP-70 in humans. Although our data cannot confirm a causal effect of HSP-70 responses, and the study was not powered to detect changes in clinical outcome between the Gln and control group, our data indicate that Gln-mediated increases in HSP-70 over baseline levels are significantly correlated with decreased in ICU length of stay and days on mechanical ventilation. It is important to note that ventilator days and ICU length stay are likely linked, and thus the ICU length of stay has been focused on in our analysis. Additional studies to define the effects of enteral and parenteral Gln administration on serum and tissue HSP-70 levels and which are designed to examine cellular and tissue induction of HSP-70 and clinical outcomes in critically ill patients are indicated.
References
Benjamin IJ, McMillan DR (1998) Stress (heat shock) proteins: molecular chaperones in cardiovascular biology and disease. Circ Res 83:117–132
De Maio A (1999) Heat shock proteins: facts, thoughts, and dreams. Shock 11:1–12
Ribeiro SP, Villar J, Downey GP, Edelson JD, Slutsky AS (1994) Sodium arsenite induces heat shock protein-72 kilodalton expression in the lungs and protects rats against sepsis. Crit Care Med 22:922–929
Ribeiro SP, Villar J, Downey GP, Edelson JD, Slutsky AS (1996) Effects of the stress response in septic rats and LPS-stimulated alveolar macrophages: evidence for TNF-alpha posttranslational regulation. Am J Respir Crit Care Med 154:1843–1850
Ribeiro SP, Villar J, Slutsky AS (1995) Induction of the stress response to prevent organ injury. New Horiz 3:301–311
Schroeder S, Lindemann C, Hoeft A, Putensen C, Decker D, von Ruecker AA, Stuber F (1999) Impaired inducibility of heat shock protein 70 in peripheral blood lymphocytes of patients with severe sepsis. Crit Care Med 27:1080–1084
Schroeder S, Bischoff J, Lehmann LE, Hering R, von Spiegel T, Putensen C, Hoeft A, Stuber F (1999) Endotoxin inhibits heat shock protein 70 (HSP70) expression in peripheral blood mononuclear cells of patients with severe sepsis. Intensive Care Med 25:52–57
Pittet JF, Lee H, Morabito D, Howard MB, Welch WJ, Mackersie RC (2002) Serum levels of Hsp 72 measured early after trauma correlate with survival. J Trauma 52:611–6117
Wischmeyer PE, Lynch J, Liedel J, Wolfson R, Riehm J, Gottlieb L, Kahana M (2001) Glutamine administration reduces Gram-negative bacteremia in severely burned patients: a prospective, randomized, double-blind trial versus isonitrogenous control. Crit Care Med 29:2075–2080
Ziegler TR, Young LS, Benfell K, Scheltinga M, Hortos K, Bye R, Morrow FD, Jacobs DO, Smith RJ, Antin JH, et al (1992) Clinical and metabolic efficacy of glutamine-supplemented parenteral nutrition after bone marrow transplantation. A randomized, double-blind, controlled study. Ann Intern Med 116:821–828
Griffiths RD, Jones C, Palmer TE (1997) Six-month outcome of critically ill patients given glutamine-supplemented parenteral nutrition. Nutrition 13:295–302
Novak F, Heyland DK, Avenell A, Drover JW, Su X (2002) Glutamine supplementation in serious illness: a systematic review of the evidence. Crit Care Med 30:2022–2029
Wischmeyer PE, Musch MW, Madonna MB, Thisted R, Chang EB (1997) Glutamine protects intestinal epithelial cells: role of inducible HSP70. Am J Physiol 272:G879–G884
Musch MW, Hayden D, Sugi K, Straus D, Chang EB (1998) Cell-specific induction of hsp72-mediated protection by glutamine against oxidant injury in IEC18 cells. Proc Assoc Am Physicians 110:136–139
Wischmeyer PE, Kahana M, Wolfson R, Ren H, Musch MM, Chang EB (2001) Glutamine induces heat shock protein and protects against endotoxin shock in the rat. J Appl Physiol 90:2403–2410
Wischmeyer PS, Serkova KN (2004) Glutamine attenuates multiple pathways of sepsis-induced injury and improves survival following peritonitis: role of heat stress protein pathway manipulation. Presented at Society for Critical Care Medicine
Preiser JC, Wernerman J (2003) Glutamine, a life-saving nutrient, but why? Crit Care Med 31:2555–2556
Pockley AG (2003) Heat shock proteins as regulators of the immune response. Lancet 362:469–476
Liao DF, Jin ZG, Baas AS, Daum G, Gygi SP, Aebersold R, Berk BC (2000) Purification and identification of secreted oxidative stress-induced factors from vascular smooth muscle cells. J Biol Chem 275:189–196
Child DF, Williams CP, Jones RR, Hudson PR, Jones M, Smith CJ (1995) Heat shock protein studies in type 1 and type 2 diabetes and human islet cell culture. Diabet Med 12:595–599
Hightower LE, Guidon PT Jr (1989) Selective release from cultured mammalian cells of heat-shock (stress) proteins that resemble glia-axon transfer proteins. J Cell Physiol 138:257–266
Asea A, Kraeft SK, Kurt-Jones EA, Stevenson MA, Chen LB, Finberg RW, Koo GC, Calderwood SK (2000) HSP70 stimulates cytokine production through a CD14-dependant pathway, demonstrating its dual role as a chaperone and cytokine. Nat Med 6:435–442
Vabulas RM, Ahmad-Nejad P, Ghose S, Kirschning CJ, Issels RD, Wagner H (2002) HSP70 as endogenous stimulus of the Toll/interleukin-1 receptor signal pathway. J Biol Chem 277:15107–15112
Wallin RP, Lundqvist A, More SH, von Bonin A, Kiessling R, Ljunggren HG (2002) Heat-shock proteins as activators of the innate immune system. Trends Immunol 23:130–135
Gaston JS (2002) Heat shock proteins and innate immunity. Clin Exp Immunol 127:1–3
Dybdahl B, Wahba A, Haaverstad R, Kirkeby-Garstad I, Kierulf P, Espevik T, Sundan A (2004) On-pump versus off-pump coronary artery bypass grafting: more heat-shock protein 70 is released after on-pump surgery. Eur J Cardiothorac Surg 25:985–992
Garrel D (2004) The effect of supplemental enteral glutamine on plasma levels, gut function, and outcome in severe burns. JPEN J Parenter Enteral Nutr 28:123
Houdijk AP, Rijnsburger ER, Jansen J, Wesdorp RI, Weiss JK, McCamish MA, Teerlink T, Meuwissen SG, Haarman HJ, Thijs LG, van Leeuwen PA (1998) Randomised trial of glutamine-enriched enteral nutrition on infectious morbidity in patients with multiple trauma. Lancet 352:772–776
Wischmeyer PE, Singleton KD (2003) Post-treatment with single dose of glutamine attenuates IL-18 expression and reduces polymicrobial sepsis-induced mortality. Crit Care Med 31:A11
Acknowledgements
This work was supported by National Institutes of Health grants R03 DK54823 (T.R.Z.), K23 RR018379-01 (P.E.W.), and General Clinical Research Center grant M01 RR00039, and Fresenius-Kabi (T.R.Z.). The authors thank Mr. George Cotsonis of the Emory General Clinical Research Center for statistical analysis and the nurses of the Emory University Hospital SICUs for their care of the research subjects.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ziegler, T.R., Ogden, L.G., Singleton, K.D. et al. Parenteral glutamine increases serum heat shock protein 70 in critically ill patients. Intensive Care Med 31, 1079–1086 (2005). https://doi.org/10.1007/s00134-005-2690-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-005-2690-5