Abstract
Objective
This study evaluated the outcome of treatment according to the Lund concept in children with severe traumatic brain injury and investigated whether the preset goals of the protocol were achieved.
Design and setting
A two-center retrospective study in neurointensive care units at university hospitals.
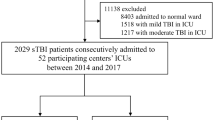
Patients
Forty-one children with severe traumatic brain injury from blunt trauma and arriving at hospital within 24 h after injury. Median age was 8.8 years (range 3 months–14.2 years), Glasgow Coma Scale 7 (3–8), and Injury Severity Score 25 (16–75). All children had pathological findings on initial computed tomography. All developed intracranial hypertension, and survivors required intensive care longer than 72 h.
Interventions
Treatment according to the principles of the Lund concept.
Measurements and results
Neurosurgery was required in 46% of the children. Survival rate was 93% and favorable outcome (Glasgow Outcome Score 4 or 5) was 80% at long-term follow-up (median 12 months postinjury, range 2.5–26). The preset physiological and biochemical goals were achieved in over 90% of observations.
Conclusions
Treating pediatric patients with severe traumatic brain injury, according to the Lund concept, results in a favorable outcome when the protocol is followed.
Similar content being viewed by others
Introduction
Despite preventive measures traumatic brain injury (TBI) remains the major injury-related mortality and morbidity factor among children [1]. Increased survival due to improved intensive care and new, aggressive treatment modalities such as decompressive craniectomy, hypertonic saline, and hypothermia have been reported [2, 3, 4, 5, 6]. Clinical outcome studies related to specific protocols are rare [7, 8].
The Lund concept is an intracranial pressure (ICP) targeted therapy based on physiological principles for volume regulation of the intracranial compartment [9]. The physiological and biochemical effects of the treatment protocol have been evaluated in experimental and clinical studies since 1994 [10, 11, 12, 13, 14]. Decreased mortality in combination with increased favorable outcome has been reported in clinical studies [15, 16, 17]. The primary aim of this study was to evaluate the outcome of treatment according to the Lund concept in a pediatric population with severe TBI. The secondary aim was to investigate whether the preset physiological and biochemical goals of the treatment protocol were achieved.
Patients and methods
This was a retrospective, two-center study of pediatric patients with severe TBI treated by the Lund concept. All medical records for children with the diagnosis of severe TBI and/or ICP monitoring were retrieved and evaluated. These records were collected from the university hospitals of Sahlgrenska and Umeå, Sweden, between January 1993 and December 2002. Both are trauma centers specially equipped and staffed to accommodate pediatric and adult neurotrauma patients, serving a metropolitan area and having regional medical responsibility for a vast rural area, about 2.5 million persons in total. The local ethics committees of the two hospitals approved the study, and written informed consent was obtained to allow review of medical charts.
Inclusion criteria were: (a) age under 15 years; (b) medical history of severe blunt head trauma; (c) arrival at hospital within 24 h after injury; (d) Glasgow Coma Scale (GCS) of 8 or less and/or Reaction Level Scale (RLS) or 3 or higher at the time of sedation and intubation; (e) need for intensive care longer than 72 h in survivors; (f) intubation due to their head trauma before arrival at the intensive care unit; and (g) treatment according to the principles of the Lund concept. Thirty-eight children fulfilled all of the inclusion criteria. Three more children developed intracranial hypertension and were treated by the Lund concept; these were included although not all of the inclusion criteria were fulfilled (one arrived at hospital 26 h after injury due to transportation problems; two required securing of the airway before transportation and were intubated as RLS 2). Median age of the 41 patients (15 girls and 26 boys) was 8.8 years (range 3 months–14.2 years). Median RLS was 4 (2–8) in the 41 patients and median GCS 7 (3–8) in 39 patients. Coma scoring by GCS could not be performed accurately in two patients; both had impaired consciousness (RLS 2), but age (3 months old) and facial fractures caused difficulty in verbal response scoring. According to pediatric GCS these two children should be classified as 8 or below [18]. We therefore considered these patients to be eligible for the study.
Five more children were admitted with severe TBI during 1993–1999. They were not treated according to the Lund concept and therefore not eligible for this study. The median GCS of these five children was 7 (3–7).
Median arrival time at the hospital was 5 h (0.5–26) from the time of the accident. All children had pathological findings on the initial CT, performed within a median of 1.5 h after injury (1–4.5 h). Injuries were due to motorvehicle accidents (including snowmobiles) in 61% and to falls in 27%; there were multiple injuries in 58%. In 5% we found blunt abdominal trauma, in 32% extracranial fractures, in 17% lung contusions, and in 7% vertebral fractures; none had cervical spine lesions. Severity of injuries was evaluated by the Injury Severity Score (ISS) [19, 20, 21]; median ISS in the overall population was 25 (16–75). The major features of the study population are summarized in Table 1.
Data for determining GCS and RLS were retrieved from medical charts by the time of intubation. RLS is the most commonly used coma scale in Sweden [22]. The time point for coma scoring was chosen because adequate coma grading cannot be performed after sedation and intubation [23]. An independent nurse evaluated outcome on the Glasgow Outcome Scale (GOS). Interview was performed when no follow-up data in medical charts were retrieved. The outcome was scored from charts for 27 children from interviews for 13 children; one patient was lost to follow-up, who according to the Swedish National Register of 2004 is still alive. GOS was determined in survivors at a median of 12 months postinjury (2.5–26).
Physiological data were collected from the time of arrival at the intensive care unit (ICU) and until removal of ICP monitoring. Bedside monitors were used for continuous monitoring of physiological parameters. Systolic arterial pressure (SAP), mean arterial pressure (MAP), diastolic arterial pressure, ICP, cerebral perfusion pressure (CPP), heart rate, oxygen saturation, and end-tidal CO2 were documented at least hourly. Obvious artifacts due to technical procedures were excluded from analysis. Serum sodium and potassium, hemoglobin, and arterial blood gases were recorded two to six times daily. Serum albumin was documented daily, with some exceptions. ICP was monitored with an intraparenchymal sensor (Camino 1993–1996, Codman MicroSensor™ 1996–2002) or an intraventricular catheter. The intraparenchymal sensor was calibrated before insertion. The intraventricular catheter zero-pressure baseline was set at the preauricular level. Blood pressure was measured invasively with the zero-pressure baseline set at heart level. Computed tomography (CT) of the brain was performed whenever necessary due to the patient’s condition. CT of the brain was repeated approx. 24 h after trauma even without any signs of deterioration.
Treatment
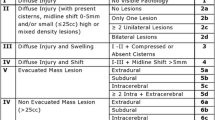
The algorithm presented in Fig. 1 describes the treatment process and the different parts of the therapy. ICP higher than 20 mmHg was the threshold for intervention and escalation of treatment. CPP of 40 mmHg was allowed [9].
Neurosurgery
Therapeutic cerebrospinal fluid drainage or evacuation of hematoma and contusion were performed to reduce intracranial content and thereby ICP. Decompressive craniectomy was conducted only in desolate situations (Fig. 1).
Normovolemia and fluid balance
Serum albumin (≥35 g/l) and red-packed cells infusions (hemoglobin ≥110 g/l) were used to maintain normovolemia and normal colloid osmotic pressure and to ensure adequate cerebral oxygenation [9, 24]. Serum sodium (135–150 mmol/l) was actively maintained within limits. Crystalloid fluid restriction and loop-diuretics were used to achieve a neutral fluid balance. Hypotension (<70 mmHg + 2× age) of systolic arterial pressure was aggressively avoided [9, 15, 24] (Fig. 1).
Normotension
Normotension, according to age, was defined in accordance with standard ranges [25]. After establishment of normovolemia a combined increase in ICP and CPP was treated by normalization of blood pressure. To normalize blood pressure and reduce the capillary hydrostatic pressure without any substantial cerebral vasodilatation a combination of metoprolol (max. 0.3 mg/kg per 24 h) and clonidine (max. 0.8 µg/kg per 24 h) was used. Decreased hydrostatic capillary pressure in combination with preservation of normal colloid osmotic pressure induces transcapillary fluid absorption [10, 11].
Sedation and reduction in stress response
Reduction in stress response and cerebral energy metabolism were achieved by continuous infusions of midazolam and fentanyl. Drug doses were adjusted so the patient was comfortable on the ventilator and able to cough on stimuli. If ICP remained continuously above 20 mmHg, a low dose of thiopental (0.5–3 mg/kg per hour) was added. The dose was adjusted to a Δ wave pattern, monitored by electroencephalography. Awakening tests were not performed.
Normoventilation
Normoventilaton was kept (PaCO2 4.5–5.5 kPa) as standard. Hyperventilation (PaCO2 <4.5 kPa) was only used if symptoms of cerebral herniation occurred. PaO2 was kept higher than 12 kPa. Positive end expiratory pressure (4–8 cmH2O) was maintained to avoid atelectasis.
Additional treatments
Dihydroergotamine (DHE) induces a venous vasoconstriction and reduces ICP by decreasing intracranial blood volume. It causes precapillary vasoconstriction and lowers the capillary hydrostatic pressure. DHE was the last pharmacological step in controlling intracranial hypertension [12] (Fig. 1). The starting dose was 0.6–0.8 µg/kg per hour, and the dose gradually reduced during 5 days. DHE was discontinued if peripheral circulation became compromised. From 1998 an infusion of low-dose prostacyclin (epoprostenol) was used in some patients to reduce transcapillary leakage and improve microcirculation in the penumbra zone (0.5 ng/kg per minute) [26]. Blood glucose levels (3–8 mmol/l) were maintained with short acting insulin. Muscle relaxants or prophylactic antiepileptic drugs were not used. A single dose of mannitol was used only if an emergency situation occurred. Hyperthermia (>38°C) was treated by paracetamol and surface cooling. Glucocorticoid (30 mg/kg metylprednisolone) was given as a single dose if hyperthermia was persistent. Enteral nutrition was started as soon as tolerated.
Statistics
Results are reported as mean ±standard deviation, percentage or median (range). The Mann-Whitney U test, a non-parametric statistic, was used to compare groups. A p level less than 0.05 was considered statistically significant.
Results
The survival rate was 93% and median GOS 5 (1–5; Fig. 2). Favorable outcome (GOS 4 and 5) was achieved in 80%. All of the deaths occurred at the ICU and within 96 h of ICP monitoring time. Two children died due to refractory intracranial hypertension and one of asystoli. The 38 survivors had a median GCS of 7 (4–8) and the three nonsurvivors 4 (3–4; p=0.005). The ISS of survivors was 25 (16–41) and that of nonsurvivors 40 (25–75; p=0.056). The five excluded children had a median GOS of 3 (1–4), which included two deaths.
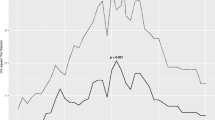
Median ICP monitoring time in all included children was 10 days (3–19). Mean ICP was 15±11 mmHg, CPP 63±11 mmHg, MAP 77±7 mmHg, and PaCO2 4.5±0.4 kPa. In the 38 survivors mean ICP was 13±4 mmHg, CPP 64±8 mmHg, MAP 78±7 mmHg, and PaCO2 4.6±0.3 kPa. In the three nonsurvivors mean ICP was 43±26 mmHg, CPP 39±15 mmHg, MAP 75±8 mmHg, and PaCO2 3.8±0.4 kPa. There were statistical significant differences between the two groups in mean ICP (day 1, p=0.009; day 2, p=0.004; day 3, p=0.037) and in mean CPP (day 2, p=0.008; day 3, p=0.04). There was no statistical difference in mean MAP between days 1 to 3 or mean CPP on day 1. Mean MAP was 66±4 mmHg in those 0–2 years old, 74±7 mmHg in those 3–5 years old, 78±5 mmHg in those 6–8 years old, 80±3 mmHg in those 9–11 years old, and 83±2 mmHg in those 12–14 years old. Mean values of maximum ICP and minimum CPP in all patients per day are shown in Fig. 3. Due to technical problems diastolic arterial pressure recordings were missing 24 h for one child.
Neurosurgery was performed in 46% of the children. Evacuation of hematomas in 34% and decompressive craniectomy in 22% (Table 1). During controlled ventilation 100% of the children received midazolam and fentanyl as continuous infusions. In 83% clonidine was administered for 7.6±4.4 days and in 76% metoprolol for 6.7±4.2 days. Thiopenthone was used 6.8±3.7 days in 88%. Vasopressors (dopamine or dopexamine) were used for 5.7±3.5 days in 34%. Vasopressor and metoprolol/clonidine infusions overlapped each other in 20%. DHE was infused in 24% and low-dose prostacyclin in 32%. Short-acting insulin was required by 27%. Glucocorticoid was given to 10%, mannitol to 34%, and diuretics to 80%. Total fluid balance during the first 10 days was +2 ml/kg per patient in survivors and +53 ml/kg per patient in nonsurvivors.
The proportion of pathological observations was 16% with intracranial hypertension, 3.9% cerebral hypoperfusion pressure, 0.4% hypoxia, 20% hyperthermia, 10% pathological blood glucose levels, 7% pathological serum sodium level, and 9% hypoalbuminemia [27] (Table 2). Figure 4 illustrates the success rate in fulfilling the treatment criteria.
Discussion
For more than 10 years the Lund concept has combined neurosurgical treatment with intensive care medicine for ICP control by a clearly defined therapy. The results of this study show that the goals of physiological and biochemical parameters were achieved, which verify treatment in accordance with our protocol. Comparison between the Lund concept and the recently published pediatric guidelines for severe TBI reveals both similarities and important differences [28]. A cornerstone of the Lund concept is aggressive maintenance of normovolemia. Optimal fluid management is probably extremely important for ensuring adequate cerebral perfusion, satisfactory cerebral oxygenation, and sufficient colloid osmotic pressure [29]. It is noteworthy that there are no comments regarding either fluid therapy or fluid balance in the pediatric guidelines (except for resuscitation) [28, 30].
The Lund concept is a treatment for vasogenic edema. In the most injured areas of the brain the blood-brain barrier is disrupted, and autoregulation can be impaired. In these damaged regions an increase in capillary hydrostatic pressure in combination with low colloid osmotic pressure causes fluid filtration. On the other hand, decreased capillary hydrostatic pressure in combination with a normal colloid osmotic pressure causes fluid absorption [9, 10, 31]. The preset goal of achieving normal serum albumin values, as a marker for normal colloid osmotic pressure, was achieved in 91% of the patients in this series.
The Lund concept includes reduction in systemic arterial pressure to decrease capillary hydrostatic pressure [11]. It has been well documented that hypotensive episodes can be deleterious in severe TBI [32, 33, 34]. Although hypotensive agents are used in the Lund concept, episodes of hypotension (defined as SAP below 70 mmHg+2× age) were detected in only 0.5% of observations. The aggressive maintenance of normovolemia is an important factor in preventing hypotensive episodes. Mean MAP as a marker of normotension in different age groups in this study was well within standard ranges and those proposed by Jones et al. [23] and Steven et al. [25].
The Lund concept accepts a CPP down to 40 mmHg in children [13]. This is in accordance with pediatric guidelines [28]. In this study CPP was kept above 40 mmHg in 96% of observations. No study has yet demonstrated that active maintenance of CPP above any threshold is related to improved outcome in pediatric severe TBI. To our knowledge, this is the first study with a CPP level in a treatment protocol in accordance with pediatric guidelines [28]. The low CPP range in our ICP-targeted therapy is controversial since the predominant strategy during the past 10 years has been a CPP-targeted approach [33]. The optimal CPP is probably related to the systemic arterial pressure. As Jones et al. [23] have pointed out, it is important to define age-related CPP limits. With improved monitoring perhaps CPP levels also can be adjusted to the degree of impaired autoregulation.
ICP monitoring is mandatory in the Lund concept. As for CPP, it is important to define age-related ICP levels. The threshold for intracranial hypertension in the Lund concept is 20 mmHg, which is in agreement with pediatric guidelines [28]. The threshold for intracranial hypertension in childhood should probably be revised downwards depending on age [23]. All of the children in this study had severe TBI; still, 84% of ICP recordings were below 20 mmHg (Fig. 2).
There is no recommendation concerning sedation and analgesia in the pediatric guidelines for severe TBI [28, 30]. Reduction in stress response and cerebral energy metabolism are important strategies in the Lund concept [9]. The awakening test is considered stressful and is not used. Pain and stress increase the cerebral metabolic demand and can increase cerebral blood flow, cerebral blood volume, and thereby ICP. The importance of stress reduction is probably underestimated and needs further investigation.
Although the children were severely traumatized, indicated by the median ISS of 25, the favorable outcome by GOS was 80%. GOS is the most widely accepted outcome scale for severe TBI and was therefore used in this study, although it was not designed for children. Various modifications of GOS have been developed over the past 10 years to satisfy a number of detailed aspects for outcome scoring of children [35]. Outcome evaluation in children is complicated by cognitive and behavioral changes in normal development, which must also be considered.
The wide range in the the time at which GOS was assessed (2–26 months) is a consequence of retrieving the source for adequate scoring in a retrospective material, approx. 12 months postinjury. Data from randomized, controlled studies on severe TBI and outcome in pediatric populations are sparse. Only few comparable studies have been published during the past decade. Simma et al. [36] used a standardized protocol for 32 children with severe TBI and had a 94% survival rate with an early 72 h (postinjury) follow-up. Studies with different treatment strategies and more long-term follow-up have reported mortality rates of 22–24% [4, 8, 23, 37].
Large prospective randomized clinical trails are essential to compare the efficacy of different strategies [32, 37, 38, 39, 40]. These are not easy to perform in children with severe TBI since the number of children treated at each center is low. In multicenter studies there can be problems comparing treatment regimes because of heterogeneous populations and different hospital standards [41]. Therefore we may have to depend on small randomized or nonrandomized studies. These studies must then be evaluated in accordance with the newly published pediatric guidelines.
In conclusion, the Lund concept is an ICP-targeted therapy combining neurosurgery with all aspects of intensive care. It is unlikely that one single therapy will be able to improve outcome after severe TBI. Different approaches must be integrated into a total concept to be successful. Pediatric patients with severe TBI treated according to the Lund concept in this study had a survival rate of 93% and favorable outcome in 80%. This study also confirms that the preset goals of the treatment protocol were achieved.
References
Mazzola CA, Adelson PD (2002) Critical care management of head trauma in children. Crit Care Med 30:S393–S401
Thakker JC, Splaingard M, Zhu J, Babel K, Bresnahan J, Havens PL (1997) Survival and functional outcome of children requiring endotracheal intubation during therapy for severe traumatic brain injury. Crit Care Med 25:1396–1401
Hackbarth RM, Rzeszutko KM, Sturm G, Donders J, Kuldanek AS, Sanfilippo DJ (2002) Survival and functional outcome in paediatric traumatic brain injury: a retrospective review and analysis of predictive factors. Crit Care Med 30:1630–1635
Taylor A, Butt W, Rosenfeld J, Shann F, Ditchfield M, Lewis E, Klug G, Wallace D, Henning R, Tibballs J (2001) A randomised trial of very early decompressive craniectomy in children with traumatic brain injury and sustained intracranial hypertension. Childs Nerv Syst 17:154–162
Khanna S, Davis D, Peterson B, Fisher B, Tung H, O’Quigley J, Deutsch R (2000) Use of hypertonic saline in the treatment of severe refractory posttraumatic intracranial hypertension in paediatric traumatic brain injury. Crit Care Med 28:1144–1151
Biswas A, Bruce DA, Sklar FH, Bokovoy JL, Sommerauer JF (2002) Treatment of acute traumatic brain injury in children with moderate hypothermia improves intracranial hypertension. Crit Care Med 30:2742–2751
Cassidy LD, Potoka DA, Adelson PD, Ford HR (2003) Development of a novel method to predict disability after head trauma in children. J Pediatr Surg 38:482–485
Downard C, Hulka F, Mullins RJ, Piatt J, Chesnut R, Quint P, Mann NC (2000) Relationship of cerebral perfusion pressure and survival in paediatric brain-injured patients. J Trauma 49:654–659
Grände PO, Asgeirsson B, Nordström CH (2002) Volume-targeted therapy of increased intracranial pressure: the Lund concept unifies surgical and non-surgical treatments. Acta Anaesthesiol Scand 46:929–941
Asgeirsson B, Grände PO, Nordström CH (1994) Effects of arterial and venous pressure alterations on transcapillary fluid exchange during raised tissue pressure. Intensive Care Med 20:567–572
Asgeirsson B, Grände PO, Nordström CH, Berntman L, Messeter K (1995) Effects of hypotensive treatment with alfa-2-agonist and beta-1 antagonist on cerebral haemodynamics in severely head injured patients. Acta Anaesthesiol Scand 39:347–351
Nilsson F, Messeter K, Grände PO, Rosén I, Ryding E, Nordström CH (1995) Effects of dihydroergotamine on cerebral circulation during experimental intracranial hypertension. Acta Anaesthesiol Scand 39:916–921
Nordström CH, Reinstrup P. Xu W, Gärdenfors A, Ungerstedt U (2003) Assessment of the lower limit for cerebral perfusion pressure in severe head injuries by bedside monitoring on regional energy metabolism. Anesthesiology 98:809–814
Kongstad L, Möller A, Grände PO (1999) Reflection coefficient for albumin and capillary fluid permeability in cat calf muscle after traumatic injury. Acta Physiol Scand 165:369–380
Eker C, Asgeirsson B, Grände PO, Schalén W, Nordström CH (1998) Improved outcome after severe head injury with a new therapy based on principles for brain volume regulation and preserved microcirculation. Crit Care Med 26:1881–1886
Naredi S, Edén E, Zäll S, Stephensen H, Rydenhag B (1998) A standardised neurosurgical/neurointensive therapy directed toward vasogenic oedema after severe traumatic brain injury: clinical results. Intensive Care Med 24:446–451
Naredi S, Olivecrona M, Lindgren C, Östlund AL, Grände PO, Koskinen LOD (2001) An outcome study of severe traumatic brain injury using the “Lund therapy” with low-dose prostacyclin. Acta Anaesthesiol Scand 45:402–406
Reilly PL, Simpson DA, Sprod R, Thomas L (1988) Assessing the conscious level in infants and young children: a paediatric version of the Glasgow Coma Scale. Childs Nerv Syst 4:30–33
Greenspan L, McLellan BA, Greig H (1985) Abbreviated Injury Scale and Injury Severity Score: a scoring chart. J Trauma 25:60–64
Ott R, Krämer R, Martus P, Bussenius-Kammerer M, Carbon R, Rupprecht H (2000) Prognostic value of trauma scores in paediatric patients with multiple injuries. J Trauma 49:729–736
Potoka DA, Schall LC, Ford HR (2001) Improved functional outcome for severely injured children treated at paediatric trauma centres. J Trauma 51:824–834
Starmark JE, Stålhammar D, Holmgren E, Rosander B (1988) A comparison of the Glasgow Coma Scale and the Reaction Level Scale (RLS85). J Neurosurg 69:699–706
Jones PA, Andrews PJD, Easton VJ, Minns RA (2003) Traumatic brain injury in childhood: intensive care time series data and outcome. Br J Neurosurg 17:29–39
Asgeirsson B, Grände PO, Nordström CH (1994) A new therapy of post-trauma brain oedema based on haemodynamic principles for brain volume regulation. Intensive Care Med 20:260–267
Steven JM, Cohen DE, Sclabassi RJ (1996) Anesthesia Equipment and monitoring. In: Motoyama EK, Davis PJ (ed) Smith’s anesthesia for infants and children. Mosby, St. Louis, pp 229–279
Möller AD, Grände PO (1997) Low-dose prostacyclin has potent capillary permeability-reducing effect in cat skeletal muscle in vivo. Am J Physiol 273:H200–H207
Venkatesh B, Garrett P, Fraenkel DJ, Purdie D (2004) Indices to quantify changes in intracranial and cerebral perfusion pressure by assessing agreement recordings. Intensive Care Med 30:510–513
Carney NA, Chesnut R, Kochanek PM (2003) Guidelines for the acute medical management of severe traumatic brain injury in infants, children and adolescents. Crit Care Med 31:417–S491
Clifton GL, Miller ER, Choi SC, Levin HS (2002) Fluid thresholds and outcome from severe brain injury. Crit Care Med 30:739–745
Bullock R, Chestnut R, Clifton GL (2000) Guidelines for the management of severe head injury. Brain Trauma Foundation, American Association of Neurological Surgeons, Joint Section on Neurotrauma and Critical Care. J Neurotrauma 17:449–627
Todd NV, Graham DI (1990) Blood-brain barrier damage in traumatic brain contusions. Acta Neurochir (Wien) 51:S296–S299
Pigula FA, Wald SL, Shackford SR, Vane DW (1993) The effect of hypotension and hypoxia on children with severe head injuries. J Pediatr Surg 28:310–316
Rosner MJ, Rosner SD, Johnson AH (1995) Cerebral perfusion pressure: management protocol and clinical results. J Neurosurg 83:949–962
Marmarou A, Anderson RL, Ward JD, Choi SC, Young HF (1991) Impact of ICP instability and hypotension on outcome in patients with severe head trauma. J Neurosurg 75:S59–S65
Crouchman M, Rossiter L, Colaco T, Forsyth R (2001) A practical outcome scale for paediatric head injury. Arch Dis Child 84:120–124
Simma B, Burger R, Falk M, Sacher P, Fanconi S (1998) A prospective, randomised, and controlled study of fluid management in children with severe head injury: lactated Ringer’s solution versus hypertonic saline. Crit Care Med 26:1265–1270
White JRM, Farukhi Z, Bull C, Christensen J, Gordon T, Paidas C, Nichols DG (2001) Predictors of outcome in severely head-injured children. Crit Care Med 29:534–540 s
Tilford JM, Simpson PM, Yeh TS, Lensing S, Aitken ME, Green JW, Harr J, Fiser DH (2001) Variation in therapy and outcome for paediatric head trauma patients. Crit Care Med 29:1056–1061
Cochran A, Scaife ER, Hansen KW, Downey EC (2003) Hyperglycemia and outcomes from paediatric traumatic brain injury. J Trauma 55:1035–1038
Vavilala MS, Bowen A, Lam AM, Uffman JC, Powell J, Winn HR, Rivara FP (2003) Blood pressure and outcome after severe paediatric traumatic brain injury. J Trauma 55:1039–1044
Maas AIR, Steyerberg EW, Murray GD, Bullock R, Baethmann A, Marshall LF, Teasdale GM (1999) Why have recent trials of neuroprotective agents in head injury failed to show convincing efficacy? A pragmatic analysis and theoretical considerations. Neurosurgery 44:1286–1297
Acknowledgements
We express our gratitude to G. Barrows, M. Palmén, C. Ritzén, A.-L. Östlund, M. Bohlin, M. Åström, and Dr. C. Cressy, MD. This study was supported by grants from the Faculty of Medicine, Umeå University, Sweden, and the Regional Health Care authority of Western Sweden.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wahlström, M.R., Olivecrona, M., Koskinen, LO.D. et al. Severe traumatic brain injury in pediatric patients: treatment and outcome using an intracranial pressure targeted therapy—the Lund concept. Intensive Care Med 31, 832–839 (2005). https://doi.org/10.1007/s00134-005-2632-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-005-2632-2