Abstract
Objective
Few comparative data exist on the responses of the subcutaneous and splanchnic circulations to evolving endotoxic shock. We therefore compared continuous subcutaneous pO2 (pO2sc) and pCO2 (pCO2sc) with simultaneous continuous gut luminal pCO2 (pCO2gi) in an animal model of endotoxaemia and examined whether changes in gas tensions track tissue energy charge (EC).
Design
Prospective observational study.
Subjects
Fourteen anaesthetized rats, 7 controls and 7 experimental.
Interventions
Controls were injected with saline, the experimental group with 20 mg/kg Klebsiella endotoxin. pCO2sc, pO2sc, and pCO2gi were measured continuously. Plasma lactate concentrations were measured at defined periods during the study. After 2 h ileal segments were snap frozen and assayed for tissue EC.
Measurements and results
Endotoxaemia resulted in a significant decrease in mean arterial blood pressure (132±9 to 71±20 mmHg) and pO2sc (71±23 to 33±22 torr) and a significant increase in pCO2gi (58±10 to 90±20 torr) and pCO2sc (56±6 to 81±25 torr). During endotoxaemia pCO2gi was directly correlated with pCO2sc (R 2=0.5) and inversely correlated with pO2sc (R 2=0.63). Plasma lactate concentrations were significantly elevated from baseline in the endotoxin limb. The mean EC was not significantly different in the two groups.
Conclusions
Both subcutaneous tissue gas tensions and intestinal luminal carbon dioxide tensions are rapidly responsive during evolving hypodynamic endotoxic shock. Alterations in tissue gas tensions were not associated with dysoxia.
Similar content being viewed by others
Introduction
The compensatory neurohumoral mechanisms triggered during the evolution of shock cause redistribution of blood flow away from the splanchnic and cutaneous circulations [1, 2]. This forms the basis of gastric tonometry as an early indicator of covert shock [3]. Data derived from gastric tonometry have been shown to prognosticate outcome in critically ill patients [4, 5, 6, 7]; however, errors in gastric luminal pCO2 measurement and the bicarbonate assumption may lead to errors in the estimation of intramucosal acidosis [8, 9]. In addition, the presence of luminal blood and enteral feeds may delay and blunt the tissue pCO2 response to mucosal ischaemia [10]. Our group has examined the other known “early responder” site to shock namely the subcutaneous tissue. In an animal model of haemorrhage we have demonstrated a close concordance between the subcutaneous tissue and ileal luminal gas tensions during shock and resuscitation [11]. We have subsequently confirmed both the feasibility of measuring subcutaneous pO2 and its good correlation with changes in mucosal CO2 tensions in patients during burns shock and resuscitation [12]. This in addition to other published data constitutes a large body of evidence supporting the usefulness of subcutaneous monitoring in hypovolaemic shock [13, 14].
In endotoxic shock, however, a number of factors limit the usefulness of published data on tissue oxygenation. Tissue oxygen tensions measured during sepsis do not change in any consistent direction from baseline [15, 16, 17, 18, 19]. Although published data on tissue oxygenation during endotoxaemia provide information on ileal, urinary and skeletal muscle pO2, these measurement techniques are unlikely to reach clinical application owing to technological and logistical problems. Also, information on concomitant changes in tissue pCO2 during endotoxaemia is sparse [20]. There is a paucity of data on subcutaneous gas tensions during endotoxaemia and their concordance with ileal mucosal gas tensions. Finally, the true relationship between tissue oxygen tensions and dysoxia must be clarified before tissue pO2 can reliably be used as a marker of cellular dysoxia.
We designed an experimental model of sepsis to examine the following questions: (a) How do subcutaneous gas tensions change in response to an endotoxic insult? (b) Do changes in subcutaneous gas tensions reflect mucosal hypercapnia during endotoxaemia? (c) What is the relationship between gut luminal and subcutaneous gas tensions, on the one hand, and gut energy stores, on the other, during endotoxaemia?
Material and methods
The study was approved by the University of Queensland Animal Ethics Experimentation Committee. The principles of laboratory animal care met the standards of the National Institutes of Health as well as those of the National Health and Medical Research Council of Australia. The study was a prospective randomized interventional study with controls. The animals were randomized by a sealed envelope technique into one of two groups: controls and endotoxaemic group
Surgical preparation
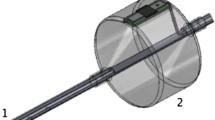
After a water-only overnight fast 14 male Sprague-Dawley rats (310–470 g) were anaesthetized with sodium pentobarbitone (60 mg/kg intraperitoneally) and ventilated via a tracheostomy with oxygen and isoflurane using a Harvard Rodent Ventilator. Isoflurane was chosen as the maintenance anaesthetic agent for its favourable cardiovascular profile in maintaining perfusion to the splanchnic and the cutaneous circulations [21]. Cannulae (22 gauge) were placed in the common carotid artery and the jugular vein for mean arterial blood pressure (MAP) monitoring and intravenous access, respectively. A 10-cm-long silastic tube was inserted into the subcutaneous tissue of the skin on the ventrolateral aspect between the groin and the axilla. At laparotomy a silastic tube of the same length was placed in the proximal ileum. A multiparameter tissue gas sensor (Paratrend 7, Diametrics Medical, Bucks, UK) was inserted into the subcutaneous and ileal silastic tubing. pCO2 measurements from ileal lumen (pCO2gi) and pO2 and pCO2 measurements from the subcutaneous tissue (pO2sc, pCO2sc) were recorded continuously. Minute ventilation was adjusted until the arterial pCO2 was in the range 30–50 mmHg. Normal saline was infused into the carotid artery at 3 ml/h. Normal saline was chosen as the administered crystalloid to replicate clinical resuscitated sepsis as closely as possible, a situation in which normal saline is commonly infused. The inspired isoflurane concentration was adjusted to maintain a MAP of approx. 100 mmHg. The ileal temperature was kept within the range 35–38° C.
Experimental design
Following surgical preparation, vascular cannulation and placement of sensors the animals were observed for 30 min to achieve steady state conditions. When stability was achieved, the following protocols were followed: in the control group (n =7) an intravenous bolus of 1 ml normal saline was administered; in the endotoxaemic group [19] (n =7) an intravenous bolus of endotoxin (Klebsiella serotype 0127:B8, Sigma Pharmaceuticals) at a dose of 20 mg/kg in 1 ml saline was administered. The mean weights of the rats in the two groups were comparable (415±19 in controls vs. 438±25 g in the endotoxin limb). The total maintenance fluid input was adjusted to be 3 ml/100 g per hour throughout the experiment. All animals were monitored for 120 min after the injection. At the end of the 120-min period a small segment of ileum was snap-frozen using clamps pre-cooled in liquid nitrogen, and stored at −70°C for later assay of ATP, ADP and AMP content and energy charge (EC). At the end of the experiment all animals were killed under anaesthesia by bilateral thoracotomy.
Physiological measurements
Tissue gas tensions was measured by the Paratrend 7, comprised of optodes for the measurement of pH, pCO2 and pO2 and a thermocouple for the measurement of temperature [22]. The mean 90% in vitro response times of the pH, pCO2 and pO2 sensors are 70, 143 and 76 s respectively. Subcutaneous and ileal luminal gas tensions and temperature were measured continuously using this device. At the beginning and end of each experiment the sensor was calibrated with calibration gases at 37°C. Arterial blood pressure was measured continuously using a pressure transducer with output displayed on a portable monitor (Model 1275A, Hewlett-Packard, Waltham, Mass., USA). Arterial blood specimens were analysed for blood gases and lactate concentrations (ABL 620, Radiometer Copenhagen, Denmark).
We chose a sample size of seven in each limb. As one of the important aims of our study was to examine differences in gut EC, a sample size of seven would have allowed us to detect a difference in EC of 0.2 with a power of 0.9.
Time points of data collection
Arterial blood gases and plasma lactate concentrations were measured pre-endotoxin injection and at 60-min intervals subsequently. Gas tensions in the subcutaneous tissue and in the ileum were collected at 1-min intervals. Samples of ileum for nucleotide assay were collected at 120 min following injection of saline or endotoxin.
Biochemical analysis of nucleotides
The biochemical assay of nucleotides was based on the method described by Cross et al. [23]. Values for total adenine nucleotides (TAN; i.e. ATP +ADP+AMP) and EC [i.e. ATP+(0.5*ADP/TAN)] were calculated from the measured levels of tissue nucleotides [24] and expressed per gram of protein. The nucleotide assays were performed by an investigator who was blinded to both the experimental group and to the corresponding tissue gas tension data.
Data analysis
A professional biostatistician analysed the data. Generalized linear models were fitted to the time series. All models accounted for the fact that data were obtained as repeated measurements per subject over time. The models (a) considered whether there were linear trends with time (steady increase or decrease as the most clinically relevant trend of interest) and (b) assessed whether the observed relationship was influenced by limb (interaction effect). Model error structures were specified to account for the repeated measures nature of the collected data.
The baseline gas tension in each vascular bed was defined as the mean value recorded for the 5 min prior to endotoxin injection. The peak pCO2 and the nadir pO2 values during the shock phase were defined as the value with the greatest deviation from baseline. The magnitude of change in tissue gas tensions during endotoxaemia was calculated as the difference between the baseline and nadir values. Within animal gas tension differences were determined by paired t test. Analysis of variance for repeated measures was used to determine the time point at which gas tensions changed significantly from baseline during endotoxaemia. Pearson’s correlation coefficient was used to examine the relationship between subcutaneous and ileal luminal gas tensions. Regression analysis was used to examine the relationship between tissue gas tensions and nucleotide assays and EC. Unless otherwise specified, results are presented as mean ±SD. Statistical significance was defined to be at the conventional 95% level (two-tailed).
Results
Haemodynamic data
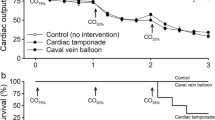
The mean baseline MAP in the control group was 117±14 mmHg, reaching a nadir value of 108±13 mmHg during the 2-h period (p =0.13). In the endotoxin limb there was a significant drop in MAP from 132±9 mmHg at baseline to a nadir value of 71±20 mmHg (p <0.001). At the end of the 2 h significant differences persisted in MAP between controls (132±16 mmHg) and the endotoxin limb (99±34 mmHg, p =0.04). MAP changes in both limbs are illustrated in Fig. 1.
Blood gas data
There were no significant differences in arterial gas tensions or pH between the two limbs at any stage during the study (Table 1).
Tissue gas tensions
Tissue pO2
Endotoxaemia resulted in a statistically significant decrease in pO2sc (p <0.05; Table 2). Although there was a downward drift of the pO2sc in controls, these did not reach statistical significance.
Tissue CO2
Baseline tissue CO2 tensions in the two study groups were comparable in both the subcutaneous tissue and in the ileal lumen (Table 2). Endotoxaemia resulted in a statistically significant increase in pCO2gi ( p <0.05) and pCO2sc (p <0.05). No significant changes in tissue pCO2 were observed in controls.
Time course of changes
Following endotoxin injection, both pCO2gi and pO2sc responded rapidly. The times to significant change from baseline were 21 min (p =0.01) and 25 min (p =0.04) for pCO2gi and pO2sc, respectively. The time to significant change for pCO2sc from baseline was 29 min (p =0.03). The changes in pO2sc and pCO2gi during the experiment are illustrated in Fig. 2.
Mean tissue gas tensions following saline or endotoxin injection. White open triangles pCO2gi in control limb; white filled triangles pCO2gi in endotoxin limb; black open squares pO2sc in control limb; black filled squares pO2sc in endotoxin limb; black open diamonds pCO2sc in control limb; black filled diamonds pCO2sc in endotoxin limb; arrow A time of injection of saline or endotoxin. To avoid crowding of data and to preserve clarity, only representative error bars are shown
Changes in mucosal and subcutaneous CO2 gap (tissue pCO2−arterial pCO2)
The mucosal CO2 gap was similar at baseline in endotoxin and control groups (22±11 mmHg vs. 19±11.5 mmHg, respectively. Following endotoxin administration there was a statistically nonsignificant trend towards an increase in the mucosal CO2 gap at both 60 min (32±18 mmHg, p =0.18) and 120 min (p =0.24). No such trends were noted in controls. The subcutaneous CO2 gap was also similar at baseline in endotoxin and control groups (21±8 mmHg vs. 17±9 mmHg, respectively, p =0.41). Following endotoxin administration there was a significant increase in the CO2 gap at 60 min (32±11 mmHg, p =0.05) and a non-significant rise at 120 min (38±33 mmHg, p =0.24).
Relationship between the subcutaneous and ileal luminal gas tensions
During endotoxaemia pCO2gi was directly correlated with pCO2sc (R 2=0.5; p <0.001) and inversely correlated with pO2sc (R 2=0.63; p <0.001; Fig. S1 in Electronic Supplementary Material). Analysis of the relationship in individual animals also revealed a strong correlation (Table S1 in Electronic Supplementary Material) between pO2sc and pCO2gi in five of the seven animals. There was a variable degree of correlation between the subcutaneous and the mucosal CO2 gaps at baseline (R 2=0.45, p =0.09), at 60 min (R 2=0.83, p <0.01) and at 120 min (R 2=0.42, p =0.1).
Plasma lactate concentrations
Plasma lactate concentrations were comparable at baseline in the two groups, but in the endotoxin limb there were increases both at 60 min (p <0.05) and at 120 min (p =0.06; Fig. 3).
Nucleotides and energy charge
Mean gut mucosal ATP concentrations in the control and the experimental limbs were 0.46±0.12 and 0.36±0.07 µ mol/g, respectively. Mean ECs in control limb and endotoxin limbs were 0.81±0.02 and 0.78±0.03, respectively (p =0.07).
Relationship between mucosal CO2 gap and indices of dysoxia (mucosal EC vs. lactate)
EC was assessed once (at 120 min). There was a poor correlation between the final CO2 gap and EC (R 2=0.08, p =0.58) in the endotoxin limb. There was a correlation between the final CO2 gap and plasma lactate concentration at 120 min (R 2=0.4).
Discussion
In this study the primary finding was that both subcutaneous pO2 and ileal luminal CO2 are rapidly responsive to endotoxaemia. The magnitude of change in pCO2sc was less than that of pCO2gi. However, there was a strong correlation between tissue gas tensions in both circulatory beds. These observations are very similar to our findings in haemorrhagic shock [11]. The fall in tissue pO2 with endotoxaemia is due to a reduction in tissue perfusion and thus a reduction in tissue oxygen delivery. Tissue pCO2 may increase as a result of flow stagnation or anaerobic metabolism or a combination of both. The rises in CO2 gap is more in keeping with flow stagnation. This is consistent with the data of Vallet et al. [25] who have demonstrated that preservation of perfusion to the tissues during dysoxia would not be accompanied by changes in CO2 gap. The inert metabolic nature of the skin compared to the gut mucosa [26, 27] may explain the differences in CO2 responses between the two tissues. The marginally elevated baseline tissue CO2 tensions observed in their study mirrored our findings in rodents pre-haemorrhage [11]. Whilst this raises the question of tissue hypoperfusion, the normal baseline tissue oxygen tensions and plasma lactate concentrations coupled with the presence of haemodynamic stability make tissue hypoxia an unlikely contributor to the baseline tissue hypercapnia.
Are tissue gas tensions correlated with indices of dysoxia?
Dysoxia was not demonstrable, as evidenced by unaltered tissue EC in the endotoxaemic limb despite significant alterations in tissue pO2 and pCO2, CO2 gap, and plasma lactate concentrations. This confirms that tissue gas tensions are sensitive to minor perturbations in perfusion but not specific for dysoxia. Dysoxic changes are a feature of severe sustained reductions in perfusion. The increase in CO2 gap is therefore likely to be due to flow stagnation rather than anaerobic metabolism [28].
Why does pO2 not rise with endotoxaemia in this model?
Cytopathic hypoxia, thought to be an important pathophysiological process in sepsis [29], is characterized by an elevated tissue oxygen tension in the presence of deranged cellular energetics. However, our study is one of many to report a decline in tissue pO2 in sepsis [15, 16, 20]. Potential reasons for this include: (a) failure of endotoxin to induce cytopathic hypoxic changes as evidenced in our study by normal EC in both limbs, (b) differences in experimental models (hyperdynamic vs. hypodynamic sepsis), and (c) endotoxin induced microvascular shunting of blood flow away from the vicinity of the probe [30].
Comparison with previously published data
The close correlation between subcutaneous and ileal gas tensions suggests that the former accurately reflects changes in mucosal perfusion. This is consistent with data published by our group in an earlier model of haemorrhage and those of Makisalo et al. [14] also in an animal model of haemorrhage.
Critique of the study
The sensor used for the measurement of tissue gas tensions was originally designed for continuous intra-arterial blood gas and pH measurement [22] and has since been validated and widely used experimentally for the measurement of tissue O2 and CO2 tensions [10, 11, 12]. We used luminal pCO2 as an indicator of mucosal pCO2 because: (a) CO2 is highly diffusible thus allowing rapid equilibration between mucosa and lumen, and (b) published data have shown a close correlation between mesenteric venous and intestinal luminal gas tensions in a porcine model under physiological conditions and during mesenteric ischaemia [31].
As we did not measure blood flow, the hyper/hypodynamic nature of the model created cannot be determined with certainty. To mimic the clinical syndrome of resuscitated sepsis the animals were given sufficient fluid to maintain a MAP above 100 mmHg throughout most of the experiment (Fig. 1). Under these conditions a hyperdynamic state is a frequent finding. However, there is considerable dose response variability within the same species, especially over time, and the dose of endotoxin chosen was slightly higher than hyperdynamic doses used in a previous experiment [19]. It is possible therefore that with this dose we created a hypodynamic model.
We used the EC as an overall marker of dysoxic severity based on data both from ourselves and other investigators [32, 33, 34]. Although EC has been shown to remain stable for 10 h in models of caecal ligation and perforation, its temporal profile of change following endotoxin injection is not known [35]. Whilst one could argue that hyperlactaemia in the presence of a normal EC implies enhanced aerobic glycolysis rather than dysoxia, the absence of serum pyruvate concentrations limits our ability to be definitive about this mechanism.
Although we demonstrated a difference between the groups with respect to subcutaneous CO2 gap, only non-significant trends were observed with respect to the mucosal CO2 gap and plasma lactate concentrations. It is possible that a larger sample size would have resulted in statistical significance.
Could the saline related acidosis be a confounding factor in the interpretation of cardiovascular changes? Severe acidaemia has important cardiovascular effects potentially affecting the signal from tissue sensors. However, saline induced acidosis on its own rarely reduces base excess below −8 mmol/l [36, 37, 38, 39, 40]. This is also true of experimental normovolaemic haemodilution [41]. With appropriate respiratory compensation the pH thus rarely falls much below 7.3, a level unlikely to have major effects on vasomotor tone or cardiac performance [42].
In conclusion, we have demonstrated that continuous subcutaneous tissue gas tensions and intestinal luminal carbon dioxide tensions respond rapidly during evolving endotoxic shock. We have also shown that alterations in tissue gas tensions are not associated with dysoxic changes. Continuous subcutaneous oxygen and carbon dioxide tension measurement has the advantages of being minimally invasive, rapidly responsive and not subject to interference by factors such as luminal contents or duodenal reflux. Whilst the results from this study are encouraging, and the data add to the growing literature on new techniques to monitor tissue oxygenation, this mode of monitoring requires further evaluation in humans to assess its usefulness, safety and its ability to predict outcome in critical illness.
References
Dantzker D (1993) Adequacy of tissue oxygenation. Crit Care Med 21:S40–S43
Neutze JM, Wyler F, Rudolph AM (1968) Changes in distribution of cardiac output after hemorrhage in rabbits. Am J Physiol 215:857–864
Fiddian Green R (1984) A sensitive and a specific diagnostic test for intestinal ischemia using silastic tonometers. Eur Surg J 16[Suppl]:A32
Levy B, Gawalkiewicz P, Vallet B, Briancon S, Nace L, Bollaert PE (2003) Gastric capnometry with air-automated tonometry predicts outcome in critically ill patients. Crit Care Med 31:474–480
Mythen MG, Purdy G, Mackie IJ, McNally T, Webb AR, Machin SJ (1993) Postoperative multiple organ dysfunction syndrome associated with gut mucosal hypoperfusion, increased neutrophil degranulation and C1-esterase inhibitor depletion. Br J Anaesth 71:858–863
Mythen MG, Webb AR (1994) Intra-operative gut mucosal hypoperfusion is associated with increased post-operative complications and cost. Intensive Care Med 20:99–104
Hurtado FJ, Beron M, Olivera W, Garrido R, Silva J, Caragna E, Rivara D (2001) Gastric intramucosal pH and intraluminal PCO2 during weaning from mechanical ventilation. Crit Care Med 29:70–76
Venkatesh B, Morgan J, Jones RD, Clague A (1998) Validation of air as an equilibration medium in gastric tonometry: an in vitro evaluation of two techniques for measuring air PCO2. Anaesth Intensive Care 26:46–50
Morgan TJ, Venkatesh B, Endre ZH (1999) Accuracy of intramucosal pH calculated from arterial bicarbonate and the Henderson-Hasselbalch equation: assessment using simulated ischemia. Crit Care Med 27:2495–2499
Venkatesh B, Morgan TJ (2000) Blood in the gastrointestinal tract delays and blunts the PCO2 response to transient mucosal ischemia Intensive Care Med 26:1108–1115
Venkatesh B, Morgan T, Lipman J (2000) Subcutaneous oxygen tensions provide similar information to ileal luminal CO2 tensions in an animal model of hemorrhagic shock. Intensive Care Med 26:592–600
Venkatesh B, Meacher R, Muller MJ, Morgan TJ, Fraser J (2001) Monitoring tissue oxygenation during resuscitation of major burns. J Trauma 50:485–494
Soini HO, Takala J, Nordin AJ, Makisalo HJ, Hockerstedt KA (1992) Peripheral and liver tissue oxygen tensions in hemorrhagic shock. Crit Care Med 20:1330–1334
Makisalo HJ, Soini HO, Tapani Lalla ML, Hockerstedt KA (1988) Subcutaneous and liver tissue oxygen tension in hemorrhagic shock: an experimental study with whole blood and two colloids. Crit Care Med 16:857–861
Gutierrez G, Lund N, Palizas F (1991) Rabbit skeletal muscle PO2 during hypodynamic sepsis. Chest 99:224–229
Hasibeder W, Germann R, Wolf HJ, Haisjackl M, Hausdorfer H, Riedmann B, Bonatii J, Gruber E, Schwarz B, Waldenberger P, Friesenecker P, Furtner M (1996) Effects of short-term endotoxemia and dopamine on mucosal oxygenation in porcine jejunum. Am J Physiol 270:G667–G675
Hurtado FJ, Gutierrez AM, Silva N, Fernandez E, Khan AE, Gutierrez G (1992) Role of tissue hypoxia as the mechanism of lactic acidosis during E. coli endotoxemia. J Appl Physiol 72:1895–1901
Boekstegers P, Weidenhofer S, Kapsner T, Werdan K (1994) Skeletal muscle partial pressure of oxygen in patients with sepsis. Crit Care Med 22:640–650
Rosser DM, Stidwill RP, Jacobson D, Singer M (1995) Oxygen tension in the bladder epithelium rises in both high and low cardiac output endotoxemic sepsis. J Appl Physiol 79:1878–1882
Vallet B, Lund N, Curtis SE, Kelly D, Cain SM (1994) Gut and muscle tissue PO2 in endotoxemic dogs during shock and resuscitation. J Appl Physiol 76:793–800
Debaene, B, Goldfarb G, Braillon A, Jolis P, Lebrec D (1990) Effects oketamine, halothane, enflurane, and isoflurane on systemic and splanchnic hemodynamics in normovolemic and hypovolemic cirrhotic rats. Anesthesiology 73:118–124
Venkatesh B, Clutton Brock TH, Hendry SP (1994) A multiparameter sensor for continuous intra-arterial blood gas monitoring: a prospective evaluation. Crit Care Med 22:588–594
Cross M, Endre ZH, Stewart-Richardson P, Cowin GJ, Westhuyzen J, Duggleby RG, Fleming SJ (1993) 23Na-NMR detects hypoxic injury in intact kidney: increases in sodium inhibited by DMSO and DMTU. Magn Reson Med 30:465–475
Atkinson DE (1968) The energy charge of the adenylate pool as a regulatory parameter. Interaction with feedback modifiers. Biochemistry 7:4030–4034
Vallet B, Teboul JL, Cain S, Curtis S (2000) Venoarterial CO2 difference during regional ischemic or hypoxic hypoxia. J Appl Physiol 89:1317–1321
Eleftheriadis E, Kotzampassi K, Papanotas K, Heliadis N, Sarris K (1996) Gut ischemia, oxidative stress, and bacterial translocation in elevated abdominal pressure in rats. World J Surg 20:11–16
Ganong W (1997) Circulation through special regions. In: Ganong W (ed) Review of medical physiology. Appleton & Lange, Stamford, pp 567–585
Venkatesh B, Morgan T (2002) Tissue lactate concentrations in critical illness: physiology and monitoring. In: Vincent J-L (ed) Yearbook of intensive care and emergency medicine. Springer, Berlin Heidelberg New York, pp 587–603
Fink M (2002) Bench-to-bedside review: cytopathic hypoxia. Crit Care 6:491–499
Ince C, Sinaasappel M (1999) Microcirculatory oxygenation and shunting in sepsis and shock. Crit Care Med 27:1369–1377
Knichwitz, G, Rotker J, Brussel T, Kuhmann M, Mertes N, Mollhoff T (1996) A new method for continuous intramucosal PCO2 measurement in the gastrointestinal tract. Anesth Analg 83:6–11
Ataullakhanov FI, Vitvitsky VM (2002) What determines the intrcellular ATP concentration. Biosci Rep 22:501–511
Zager RA, Shaw Jurkowitz M, Merola AJ (1985) Responses of the normal rat kidney to sequential ischaemic events. Am J Physiol 249:F148–F159
Morgan TJ, Venkatesh B, Crerar-Gilbert A, Gainer J, Wilgoss D (2003)). Sodium crocetinate does not alter gut hypercapnic responses or renal energy stores during transient sub-diaphragmatic ischaemia. Intensive Care Med 29:652–654
Hampton WA, Townsend MC, Haybron DM, Shirmer WJ, Fry DE (1987) Effective hepatic blood flow and hepatic bioenergy status in murine peritonitis. J Surg Res 42:33–38
McFarlane C, Lee A (1994) A comparison of Plasmalyte 148 and 0.9% saline for intra-operative fluid replacement. Anaesthesia 49:779–781
Scheingraber S, Rehm M, Sehmisch C, Finsterer U (1999) Rapid saline infusion produces hyperchloremic acidosis in patients undergoing gynecologic surgery. Anesthesiology 90:1265–1270
Waters JH, Gottleib A, Schoenwald P, Popovich MJ, Sprung J, Nelson DR (2001) Normal saline versus lactated Ringer’s solution for intraoperative fluid management in patients undergoing abdominal aortic aneurysm repair: an outcome study. Anesth Analg 93:817–822
Wilkes NJ, Woolf R, Mutch M, Mallet SV, Peachey T, Stephen R, Mythen MG (2001) The effects of balanced versus saline-based Hetastarch and crystalloid solutions on acid-base and electrolyte status and gastric mucosal perfusion in elderly surgical patients. Anesth Analg 93:811–816
Forrest DM, Walley KR, Russell JA (1998) Impact of acid-base disorders on individual organ systems In: Ronco C, Bellomo R (eds) Critical Care Nephrology. Kluwer, Dordrecht, pp 313–326
Morgan TJ, Venkatesh B, Hall J (2004) Crystalloid strong ion difference determines metabolic acid-base change during acute normovolemic hemodilution. Intensive Care Med 30:1432–1437
Adrogue HJ, Madias NE (1998) Management of life-threatening acid-base disorders. I. N Engl J Med 338:26–34
Acknowledgements
The authors thank Ms. Diana Battistutta, Biostatistician, Queensland University of Technology for statistical analysis of data.
Author information
Authors and Affiliations
Corresponding author
Additional information
This work was made possible by a generous grant from the Australia and New Zealand Intensive Care Society and from institutional funds from the Royal Brisbane Hospital. The Paratrend 7 sensors used in the study were supplied by Diametrics Medical Inc, UK. The work was performed in the Intensive Care Laboratory, Division of Anesthesiology and Critical Care, University of Queensland.
Electronic Supplementary Material
Rights and permissions
About this article
Cite this article
Venkatesh, B., Morgan, T.J., Hall, J. et al. Subcutaneous gas tensions closely track ileal mucosal gas tensions in a model of endotoxaemia without anaerobism. Intensive Care Med 31, 447–453 (2005). https://doi.org/10.1007/s00134-005-2558-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-005-2558-8