Abstract
Objective
To investigate the dose-related effects of magnesium on pulmonary vascular resistance and associated changes in cardiac output in porcine micro-embolic pulmonary hypertension.
Design
Prospective, interventional animal study.
Setting
University animal laboratory.
Subjects
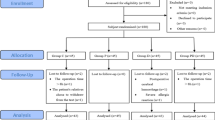
Forty anaesthetised and ventilated piglets.
Interventions
Right heart catheterisation for the measurement of cardiac output, pulmonary artery pressure, central venous pressure and pulmonary capillary wedge pressure; arterial cannulation for measurement of arterial pressures and ionised magnesium levels; calculation of pulmonary and systemic vascular resistance before and after induction of acute pulmonary micro-embolism, and without or with the administration of magnesium (0.5, 1.0, 2.0 mmol/kg bolus and 1 mmol/kg bolus followed by 1 mmol/kg per h continuous infusion).
Measurements and main results
The bolus administration of increasing doses of magnesium (0.5, 1.0, 2.0 mmol/kg) was associated with an increase in ionised serum magnesium levels and a dose-dependent decrease of mean pulmonary arterial pressure, an increase of cardiac output and a decrease of pulmonary vascular resistance. This effect was sustained after bolus administration (1 mmol/kg) followed by a continuous infusion of magnesium (1 mmol/kg per h).
Conclusions
Magnesium has a directly dose-dependent beneficial effect on the circulation in acute embolic pulmonary hypertension and improves cardiocirculatory impairment in massive pulmonary embolism (PE).
Similar content being viewed by others
Introduction
Pulmonary embolism (PE) is a significant cause of morbidity and mortality in modern societies [1, 2] and rates of clinical outcomes, such as death and recurrence, vary widely among studies [3, 4, 5, 6, 7]. Massive PE leads to an acute increase of right ventricular afterload and possible right heart failure with consecutive impairment of the systemic cardiac output [8] and altered gas exchange. These pathophysiological findings explain the high incidence of acute death after fulminant PE [9, 10, 11, 12].
Therapeutic strategies include, after appropriate recognition of the underlying disease (i.e. thrombus, gas, fat or amniotic fluid embolism), the removal or dissolution of the embolic thrombi or interventional and surgical measures [9, 13, 14]. In severe forms, ventilation with high inspiratory oxygen concentration, selective pulmonary vasodilation and support of the cardiac output (CO) is beneficial for outcome [15, 16, 17, 18].
Magnesium plays a significant role in the tone of vascular smooth muscles and its effect can be characterised as calcium-antagonistic. Higher levels of ionised magnesium promote vascular relaxation. In several studies, magnesium sulphate was reported to have beneficial effects on primary pulmonary hypertension and secondary pulmonary hypertension after correction of congenital heart defects [19, 20, 21]. Additionally, its use in hypoxic pulmonary hypertension accentuates the effect of nitric oxide [22].
The objective of the present study was to investigate the dose-dependent effects of increasing doses of magnesium on the cardiovascular system in a porcine model of acute massive PE.
Material and methods
The study was approved by the local ethics committee (Senatsverwaltung fuer Gesundheit und Soziales des Landes Berlin, Ziffer G 0350/95). All investigations were performed at the animal research laboratories of the Humbold University of Berlin, Campus Charité, Rudolf Virchow Klinikum, Wedding, Berlin.
Animal preparation
We used German Landrace piglets with body weights from 12 to 18 kg. All animals were handled according to the guidelines published by the National Institutes of Health and the Council of the American Physiologic Society [23]. Following overnight fasting and premedication with azaperone (Stresnil; Janssen; Neuss, Germany; 4 mg/kg i.m.) and atropine 0.05 mg, the animals were anaesthetised using i.v. administered methohexital (Brevimythal, 1–4 mg/kg per h) and fentanyl (Janssen, 0.05–0.1 mg/kg) and paralysed with pancouronium bromide (Organon Teknika, Eppelheim, Germany; 0.1–0.3 mg/kg). Ringers’ solution was administered during the entire study period at a rate of 3–5 ml/kg per h. After endotracheal intubation, the lungs were mechanically ventilated at a rate of 20 breaths/min (Servo 300 A Ventilator, Siemens Elema, Solna, Sweden). The tidal volume was adjusted to ensure a PaCO2 between 35 and 40 mmHg with a maximal peak inspiratory pressure at 20 cmH2O and a PEEP of 5 cmH2O. The fraction of inspired oxygen (FIO2) was set at 0.5. This ventilatory regimen was maintained throughout the initial study period. The rectal temperatures of all animals were maintained at a constant level of 35–37°C.
Using cutdown procedures, all animals underwent insertion of a right carotid arterial catheter, (Leader Cath 20G; Laboratoires Pharmaceutiques Vygon, Ecouen France), a right internal jugular vein 5.5 Fr thermistor-tipped flow-directed pulmonary artery catheter (93–631–5.5 Fr; Baxter Healthcare, Irvine, California) and a right external jugular central venous line (Arrow, CS-15854-E, 8.5 Fr, 20 cm).
The tip of the pulmonary artery catheter was placed in the pulmonary artery and the correct placement was verified by a recording of the typical pressure trace after the pulmonary artery was entered and measurement of the pulmonary capillary wedge pressure (PCWP). The position of the catheter tip was corrected during the study whenever necessary. Non-heparinised 0.9% normal saline solution (2 ml/h) was used to maintain the patency of all lines. Each catheter line was connected to a pressure transducer that was levelled to mid-heart. The transducer output was displayed and recorded continuously on a multi-channel recorder (Marquette). Measurements included systolic, diastolic and mean arterial pressure (SAP, DAP, MAP), heart rate (HR), central venous pressure (CVP), systolic, diastolic and mean pulmonary artery pressure (SPAP, DPAP, MPAP) and PCWP. All haemodynamic measurements were taken at end-expiration without expiratory hold.
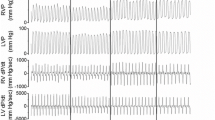
At predetermined time points (T prae, T post, T-0, T-5, T-15, T-30 and T-60 min, see Fig. 1), the haemodynamic measurements were reported and CO was determined by the thermodilution method using a CO computer (Marquette). To achieve CO measurements, 5 ml boluses of ice-cold saline were injected at end-expiration via the injection port of the pulmonary artery catheter. The thermodilution curve was inspected for accurate measurement and the mean value from three consecutive measurements was recorded. The haemodynamic parameters were calculated using standard formulas: pulmonary vascular resistance (PVR)=(MPAP-PCWP) x CO-1x79.9 and systemic vascular resistance (SVR)=(MAP-CVP) x CO-1x79.9.
Experimental protocol
After termination of the preparation period, all animals were allowed to stabilise for 60 min. All variables were then determined under steady-state conditions. Acute massive PE was induced by stepwise injection of 300 μm microspheres (Sephadex G25 superfine; Pharmacia Biotech, Freiburg, Germany) into the superior vena cava over 5 min [18, 22, 24, 25, 26].
Pilot experiments in our institution demonstrated a significant variability of the individual response of the animals to fixed doses of the microspheres injected [27] and the first two animals died due to acute right heart failure. We therefore used an individually titrated injection protocol to achieve an initial MPAP of 50 mmHg within a 5-min period. This was accompanied by an increase in HR and a decrease of the MAP, and can be interpreted as the acute circulatory response to massive PE. Usually a spontaneous decrease of the MPAP was observed after some minutes and a repeat injection was necessary thereafter. These findings are consistent with the findings of other animal models [18]. After induction of the massive PE, the animals were again allowed to stabilise for 60 min. Thereafter, all variables were determined again under the new steady-state conditions for another 60 min (see Table 1). Ventilation was adjusted to a FIO2 of 100% and the respiratory rate was set to achieve a PaCO2 of less than 50 mmHg and a pH of more than 7.3.
Following this period of stabilisation, the animals were randomly assorted to the different groups (A–E) of the study protocol. One group (A) did not receive any magnesium administration. In the subsequent groups B, C, and D magnesium was administered as a bolus of 0.5, 1.0 and 2.0 mmol/kg over 5 min, respectively. The last group (E) received a magnesium bolus of 1 mmol/kg over 5 min followed by a continuous infusion of 1 mmol/kg per h. Serial sets of measurements were taken at 0, and then 5, 15, 30 and 60 min after the start of the magnesium bolus. Serum levels of ionised magnesium were measured at the points T prae, T post, T-0, T-5, T-15, T-30 and T-60 min (see Fig. 1) after magnesium administration using atomic absorption spectroscopy (Perkin Elmer 1100, Ueberlingen, Germany; at 285.5 νm wavelength).
No attempts were made to correct any haemodynamic changes observed during the entire study period with additional fluid administration or inotropic agents. After completion of the protocol, all animals were killed by the injection of a lethal dose of potassium chloride and subsequent post mortem examinations were performed to exclude intracardiac shunts.
Statistical analysis
Statistical analysis was performed using the computer programme SPSS (Version 7.5). The data are presented as means and median values and standard deviation of the mean in each group. All measurements of the treatment groups B, C, D, and E were compared with the results of the control group (A) at the specific time points (T-0, T-5, T-15, T-30 and T-60). The analysis concentrated on the effects of this magnesium therapy on measurements of the variables: magnesium levels, MPAP, MSAP, CO, PVR and SVR. Due to the non-constant variance across the different groups and times involved, the following non-parametric analyses were conducted:
-
1.
‘Friedman’ and ‘Kendall’s W’ tests for multiple related samples, to confirm that control group measurements remained steady over time.
-
2.
At each time of observation (from “steady state” onwards), a Kruskal-Wallis test for comparison of multiple independent samples was conducted to determine whether differences existed between any of the groups at that time, followed by a series of Mann-Whitney U tests to confirm which of the groups differed significantly from the control group at that time.
The results of these tests are shown in the following graphs, one for each of the variables mentioned above. For each variable, the corresponding graph shows the observed mean measurement for each group at each time, together with a 95% confidence interval for the population mean. The annotations * and + on the graphs indicate that a significant result (p<0.05 and p<0.01, respectively) was obtained from the Mann-Whitney comparison test for that combination of group and time.
Results
We administered consecutive doses of the micro-emboli to obtain an increase in pulmonary artery pressure (PAP) of about 50 mmHg. To achieve this, doses of 0.1–1.0 mg of microspheres had to be injected (median 0.35 mg). In the first two animals, acute PE led to an acute right heart failure and death. Subsequent administrations were changed and smaller doses were administered stepwise and no additional acute mortality was observed in the animals investigated.
The acute effects of the pulmonary embolisation are summarised in Table 1. The acute embolisation was followed by an increase in PAP, CVP and HR, and a massive increase (+400%) in PVR, as well as a decrease in MAP and CO. After the stabilisation period of 60 min the baseline measurements were used to compare the effects of the different doses of magnesium administered. The magnesium administration led to a dose-dependent increase of the concentration of ionised serum magnesium (see Fig.2). With bolus administration there was a rapid increase in serum magnesium and a subsequent decline. Bolus administration followed by a continuous infusion was able to stabilise the serum magnesium levels at about 4 mmol/l of ionised magnesium.
The increase of serum magnesium was followed by a dose-dependent decrease of PAP and CVP, and an increase in CO (see Figs. 3 and 4). There was no significant change in HR, but MAP and SVR decreased significantly at higher doses (see Figs. 5 and 6). The direct dose-dependent influence of the concentration of ionised serum magnesium on PVR is shown in Fig. 7. The control did not show significant changes compared to the baseline measurements. No significant changes in oxygenation or CO2 exchange were seen.
The post mortem examination performed in all animals excluded the presence of intracardiac shunts.
Discussion
This investigational study is, to our knowledge, the first to report the beneficial dose-dependent effects of magnesium in severe experimental PE. Magnesium has been described as “nature’s physiological calcium blocker” and is a muscle relaxant and a potent vasodilatory agent [28, 29, 30, 31]. Magnesium inhibits Ca2+-induced muscle contraction by inhibition of the Ca2+ release from the sarcoplasmic reticulum and it competes with calcium at several binding sites on troponin and myosin [32, 33]. Magnesium ions are important for the regulation of Na+ and K+ transport across cell membranes, including cardiac and smooth muscle cells [34]. The effect of magnesium in hypoxic pulmonary vasoconstriction is related to the inhibition of Ca2+-dependent K+ channels [22] and it is essential for cGMP- and cAMP-mediated mechanisms of pulmonary vascular relaxation [30]. The vasodilator effect of magnesium seems to be endothelium-independent but related to the serum concentrations [31]. Additionally, magnesium increases the local production of vasodilatory prostaglandins (i.e. prostacyclin) [35]. In vitro studies have shown that the magnesium ion (Mg2+) modulates smooth muscle contractility and mediator release [33]. This effect is comparable to the inhibition of calcium-dependent muscle contraction of other divalent cations, such as zinc (Zn2+) [36, 37], or specific calcium channel blockers, such as nifedipine, used to treat pulmonary hypertension [38, 39, 40, 41].
Several reports have suggested that magnesium may be a therapeutic agent with which to treat elevated PVR [20, 42]. Persistent pulmonary hypertension of the newborn (PPHN) is potentially fatal and various therapeutic strategies have been used including systemic and inhalant vasodilatory agents, ECMO and, more recently, inhaled nitric oxide [43, 44, 45, 46, 47]. Several clinical trials to treat PPHN with the use of magnesium have been published [19, 21, 48]. These results indicate that magnesium is very useful in improving oxygenation by pulmonary vasodilatation in these patients. The side effects observed were a slight decrease in heart rate [21] and various degrees of systemic hypotension [49, 50].
The normal plasma levels of magnesium range from 0.75 to 1.5 mmol/l and about 60% is ionised (0.4–0.7 mmol/l) [32]. Hypermagnesaemia (2.27±0.25 mmol total serum magnesium) lowered PAP and delayed the fall in SAP and stroke volume in lambs exposed to hypoxia-induced pulmonary hypertension [51]. This effect seems to be correlated to the level of oxygen in the pulmonary artery, and magnesium can prevent and reduce hypoxia-induced pulmonary hypertension [52, 53]. Increasing aliquots of 1 mmol/kg magnesium ions (as MgSO4) resulted in a significant decrease in PVR. In septic lambs, however, a fall in SAP was observed. This effect could be increased by the additional administration of nitric oxide [22, 50].
The serum levels reported for treating pulmonary hypertension ranged between 2.5 mmol/l and 6.6 mmol/l [19, 21, 54]; no significant changes in HR, blood pressure, renal function or serum electrolytes were observed [48, 49, 54]. The magnesium doses administered in experimental and clinical studies to treat pulmonary hypertension varied from bolus administration of 0.5 mmol/kg up to continuous infusions of 4 mmol/kg per h [20, 48]. Significant effects were observed at serum concentrations of 2.5–4.0 mmol/l of total serum magnesium. In our animal model we tested the different doses described and could correlate increasing levels of ionised magnesium to decreasing PVR and increasing CO (see Figs. 4 and 7). Only at levels of ionised magnesium above 4 mmol/l did we find a significant decrease in the mean arterial blood pressure. This effect was not found in studies when smaller amounts of magnesium were administered and lower plasma levels were achieved [48, 49, 54]. Therefore the therapeutic usefulness of magnesium using high doses may be limited by its relative non-selectivity. However, this side effect could be minimised by the administration of catecholamines for the circulatory support of severe PE [8, 55, 56].
The increase in PVR in micro-embolic lung injury occurs at the periphery of the pulmonary arterial tree [27, 57]. It rapidly (after 2 h) induces proinflammatory, mitogenic and vasoconstrictive gene expression (endothelins, arachidonate oxidases, thromboxane, serotonin) that increases with the severity and duration of vascular occlusion [58, 59]. A potential beneficial effect of magnesium on this secondary vasoconstriction has been discussed [22, 31, 35], but has not been proven yet. It is postulated that magnesium may act through an increase of the production of endogenous nitric oxide [60, 61] and this may contribute to its clinical effect.
Afterload reduction in acute cor pulmonale after massive PE is essential to improve the right ventricular dysfunction [8, 11]. This therapeutic principle was proven useful in other causes of right ventricular failure [62]. Selective pulmonary vasodilators, such as inhaled nitric oxide and aerolised prostacyclin, achieved pulmonary vasodilatation in patients with congenital cardiac defects and pulmonary hypertension [63]. In our animal model we could show a dose-dependent decrease in PVR and increase in CO (see Figs. 4 and 7). Right ventricular dysfunction has long been recognised as a marker for poor outcome in patients with PE, especially in those with haemodynamic instability. Cardiac arrest will occur within 1–2 h after the onset of clinical presentation in two thirds of fatal PE cases [10]. A significant reduction of PVR and PAP with an increase in CO within the first hour of treatment of massive PE could separate the survivors from the non-survivors [12].
In conclusion, this laboratory study provides evidence that the administration of magnesium may have therapeutic value as an adjunct to traditional therapy in acute PE or when other treatment strategies, such as NO or prostacyclins, are not available. It is also a simple treatment and of low cost. However, further experimental and clinical studies of magnesium and its potentially beneficial effect on the outcome of fulminant PE are needed.
References
Sakuma M, Konno Y, Shirato K (2002) Increasing mortality from pulmonary embolism in Japan, 1951–2000. Circ J 66:1144–1149
Lilienfeld DE (2000) Decreasing mortality from pulmonary embolism in the United States, 1979–1996. Int J Epidemiol 29: 465–469
Laissue JA, Gebbers JO, Musy JP (1984) Pulmonary embolism: epidemiology and pathology. Schweiz Med Wochenschr 114:1711–1720
Hansson PO, Welin L, Tibblin G, Eriksson H (1997) Deep vein thrombosis and pulmonary embolism in the general population. ‘The study of men born in 1913’. Arch Intern Med 157:1665–1670
Bussani R, Cosatti C (1990) Pulmonary embolism: epidemiologic analysis of 27,410 autopsies during a 10-year period. Medicina 10:40–43
Goldhaber SZ, Visani L, De Rosa M (1999) Acute pulmonary embolism: clinical outcomes in the international cooperative pulmonary embolism registry (ICOPER). Lancet 353:1386–1389
Lignitz E, Lignitz G, Puschel K (1995) Lung embolism as the cause of death in legal medicine. Versicherungsmedizin 47:203–207
Vieillard-Baron A, Jardin F (2003) Why protect the right ventricle in patients with acute respiratory distress syndrome? Curr Opin Crit Care 9:15–21
British Thoracic Society (2003) Guidelines for the management of suspected acute pulmonary embolism. Thorax 58:470–483
Wood KE (2002) Major pulmonary embolism. Chest 121:877–905
Comess KA, DeRook FA, Russell ML, Tognazzi-Evans TA, Beach KW (2000) The incidence of pulmonary embolism in unexplained sudden cardiac arrest with pulseless electrical activity. Am J Med 109:351–356
Krivec B, Voga G, Zuran I, Skale R, Pareznik R, Podbegar M, Noc M (1997) Diagnosis and treatment of shock due to massive pulmonary embolism. Chest 112:1310–1316
Spohr F, Boettiger BW (2003) Thrombolytic therapy during and after cardiopulmonary resuscitation. Efficacy and safety of a new therapeutic approach. Minerva Anestesiol 69:357–364
Gei AF, Vadhera RB, Hankins GD (2003) Embolism during pregnancy: thrombus, air and amniotic fluid. Anesthesiol Clin N Am 21:165–182
Kucher N, Luder CM, Dornhofer T, Windecker S, Meier B, Hess OM (2003) Novel management strategy for patients with suspected pulmonary embolism. Eur Heart J 24:366–376
Hasei M, Inamori N, Hitomi K, Tanigami H, Hirata T, Mori T (2003) Intensive care management of acute pulmonary thromboembolism. Masui 52:14–19
Hsieh YY, Chang CC, Li PC (2000) Successful application of extracorporal membrane oxygenation and intraaortic balloon counterpulsation as a lifesaving therapy for a patient with amniotic fluid embolism. Am J Obstet Gynecol 183:496–497
Boettiger BW, Motsch J, Doersam J, Mieck U, Gries A, Weimann J, Martin E (1996) Inhaled nitric oxide selectively decreases pulmonary artery pressure and pulmonary vascular resistance following acute massive pulmonary microembolism in piglets. Chest 110:1041–1047
Daffa SH, Milaat WA (2002) Role of magnesium sulphate in treatment of severe persistent pulmonary hypertension of the newborn. Saudi Med J 23:1266–1269
Lin SC, Teng RJ, Wang JK (1996) Management of severe pulmonary hypertension in an infant with obstructed total anomalous pulmonary venous return using magnesium sulfate. Int J Cardiol 56:131–135
Tolsa JF, Cotting J, Sekarski N, Payot M, Micheli JL, Calame A (1995) Magnesium sulphate as an alternative and safe treatment for severe persistent pulmonary hypertension of the newborn. Arch Dis Child 72:F184–F187
Haas KM, Suzuki S, Yamaguchi N, Kato I, Ban K, Tanaka T, Fukuda S, Togari H (2002) Nitric oxide further attenuates pulmonary hypertension in magnesium-treated piglets. Pediatr Int 44:670–674
National Institutes of Health (1985) Guide for the care and use of laboratory animals (NIH publication No. 85–23). Washington, DC: NIH
Shelub I, van Grondelle A, McCullough R, Hofmeister S, Reeves JT (1984) A model of embolic chronic pulmonary hypertension in the dog. J Appl Physiol 56:810–815
Weimann J, Zink W, Schnabel PA, Jakob H, Gebhard MM, Martin D, Motsch J (1999). Selective vasodilation by nitric oxide during sustained pulmonary hypertension following recurrent microembolism in pigs. J Crit Care 14:133–140
Jones AE, Watts JA, Debelak JP, Thornton LR, Younger JG, Kline J (2003) Inhibition of prostaglandin synthesis during polystyrene microsphere-induced pulmonary embolism in the rat. Am J Physiol Lung Cell Mol Physiol 284:L1072–1081
Delcroix M, Melot C, Vachiery JL, Lejeune P, Leeman M, Vanderhoeft P, Naeije R (1990) Effects of embolus size on hemodynamics and gas exchange in canine embolic pulmonary hypertension. J Appl Physiol 69:2254–2261
Altura BM, Altura BT (1981) Magnesium ions and contraction of vascular smooth muscles: relationship to some vascular diseases. (FASEB J) Fed Proc 40:2672–2679
Belfort MA, Anthony J, Saade GR, Allen JC (2003) A comparison of magnesium sulfate and nimodipine for the prevention of eclampsia. N Engl J Med 348:304–311
Fullerton DA, Hahn AR, Agrafojo J, Sheridan BC, McIntyre RC (1996) Magnesium is essential in mechanisms of pulmonary vasomotor control. J Surg Res 63:93–97
Villamor E, Perez-Vizcaino F, Ruiz T, Tamargo J, Moro M (1996) In vitro effects of magnesium sulfate in isolated intrapulmonary and mesenteric arteries of piglets. Pediatr Res 39:1107–1112
Connolly E, Worthley LIG (1999) Intravenous magnesium. Crit Care Resuscitation 1:162–172
Yoshimura M, Oshima T, Matsuura H, Ishida T, Kambe M, Kajiyama G (1997) Extracellular Mg2+ inhibits capacitative Ca2+ entry in vascular smooth muscle cells. Circulation 95:2567–2572
Altura BM, Altura BT (1984) Interactions of Mg and K on blood vessels—aspects in view of hypertension. Review of present status and new findings. Magnesium 3:175–194
Watson KV, Moldow CF, Ogburn PL, Jacob HS (1986) Magnesium sulfate: rationale for its use in preeclampsia. Proc Natl Acad Sci USA 83:1075–1078
Hirota K, Sato T, Hashimoto Y, Yoshioka H, Ohtomo N, Ishihara H, Matsuki A (1999) Relaxant effect of magnesium and zinc on histamine-induced bronchoconstriction in dogs. Crit Care Med 27:1159–1163
Cheng XY, Chen KY, Zhang XH, Zhu PH (2002) Effect of zinc ions on caffeine-induced contracture in vascular smooth muscle and skeletal muscle of rat. Cell Physiol Biochem 12:119–126
Sitbon O, Humbert M, Jagot JL, Taravella O, Fartoukh M, Parent F, Herve P, Simonneau G (1998) Inhaled nitric oxide as a screening agent for safely identifying responders to oral calcium-channel blockers in primary pulmonary hypertension. Eur Respir J 12:263–264
Rich S, Kaufmann E, Levy PS (1992) The effect of high doses of calcium-channel blockers on survival in primary pulmonary hypertension. N Engl J Med 327:76–81
Barst RJ, Maislin G, Fishman AP (1999) Vasodilator therapy for primary pulmonary hypertension in Children. Circulation 99:1197–1208
Dickstein PJ, Trinlade O, Goldberg RN, Bancalari E (1984) The effect of calcium antagonists on hypoxic pulmonary hypertension in the piglet. Pediatr Res 18:1262–1265
Patole SK, Finer NN (1995) Experimental and clinical effects of magnesium infusion in the treatment of neonatal pulmonary hypertension. Magnes Res 8:373–388
Roberts JD, Polaner DM, Lang P, Zapol WM (1992) Inhaled nitric oxide in persistent pulmonary hypertension of the newborn. Lancet 340:818–819
Bindl L, Fahnenstrich H, Peukert U (1994) Aerolised prostacyclin for pulmonary hypertension in neonates. Arch Dis Child 71:F214–216
Cornfield DN, Maynard RC, deRegnier RA, Guiang SF, Babato F, Milla CE (1999) Randomised controlled trial of low-dose inhaled nitric oxide for the treatment of term and near term infants with respiratory failure and pulmonary hypertension. Pediatrics 104:1089–1094
Sadiq HF, Mantych G, Benawra RS, Devaskar UP, Hocker JR (2003) Inhaled nitric oxide in the treatment of moderate pulmonary hypertension of the newborn: a randomised controlled multicenter trial. J Perinatol 23:98–103
Davidson D, Barefield ES, Kattwinkel J, Dudell G, Damask M, Strauer R, Rhines J, Chang CT (1998) Inhaled nitric oxide for the early treatment of persistent pulmonary hypertension of the newborn: a randomised double-masked, placebo-controlled, dose-response, multicenter study. The I-NO/PPHN study group. Pediatrics 101:325–334
Abu-Osba YK, Galal O, Manasra K, Rejjal A (1992) Treatment of severe persistent pulmonary hypertension of the newborn with magnesium sulphate. Arch Dis Child 67:31–35
Wu TJ, Teng RJ, Yau KIT (1995) Persistent pulmonary hypertension of the newborn treated with magnesium sulfate in premature neonates. Pediatrics 96:472–474
Ryan CA, Finer NN, Barrington KJ (1994) Effects of magnesium sulfate and nitric oxide in pulmonary hypertension induced by hypoxia in newborn piglets. Arch Dis Child Fetal Neonat Ed 71:F151–F155
Anderson ME, Burnette TM, Geiser DR, Janjindamai W (1994) Magnesium attenuates pulmonary hypertension due to hypoxia and group B streptococci. J Appl Physiol 77:751–756
Abu-Osba YK, Rhydderch D, Dalasundaram S, Galal O, Rejjal A, Al Halees Z, Duran C (1990) Reduction of hypoxia induced pulmonary hypertension by MgSO4 in sheep. Pediatr Res 27:351A
Cropp GJA (1968) Reduction of hypoxic pulmonary vasoconstriction by magnesium chloride. J Appl Physiol 24:755–760
Al-Halees Z, Afrane B, El-Barbary M (1997) Magnesium sulfate to facilitate weaning of nitric oxide in pulmonary hypertension. Ann Thorac Surg 63:298–299
Pagnamenta A, Fesler P, Vandinivit A, Brimioulle S, Naeije R (2003) Pulmonary vascular effects of dobutamine in experimental pulmonary hypertension. Crit Care Med 31:1140–1146
Bradford KK, Deb B, Pearl RG (2000) Combination therapy with inhaled nitric oxide and intravenous dobutamine during pulmonary hypertension in the rabbit. J Cardiovasc Pharmacol 36:146–151
Melot C, Vermeulen F, Maggiorini M, Gilbert E, Naeije R (1997) Site of pulmonary vasodilation by inhaled nitric oxide in microembolic lung injury. Am J Respir Crit Care Med 156:75–85
Grattan RM, Zagosrki J, Watts JA, Kline JA (2003) Pulmonary gene expression after experimental pulmonary embolism. Acad Emerg Med 10:576
Smulders YM (2001) Contribution of pulmonary vasoconstriction to haemodynamic instability after acute pulmonary embolism. Implications for treatment? Neth J Med 58:241–247
Izzo AA, Gagniella TS, Mascolo N, Capasso F (1994) Nitric oxide as a mediator of the laxative action of magnesium sulfate. Br J Pharmacol 113:228–232
Gold ME, Buga GM, Wood KS (1990) Antagonistic modulatory role of magnesium and calcium on release of endothelium-derived relaxing factor and smooth muscle tone. Circ Res 66:355–356
Schulze-Neick I, Bueltmann M, Werner H, Gamillscheg A, Vogel M, Berger F, Roissant R, Hetzer R, Lange PE (1997) Right ventricular function in patients treated with inhaled nitric oxide after cardiac surgery for congenital heart disease in newborns and children. Am J Cardiol 80:360–363
Schulze-Neick I, Uhlemann F, Nürnberg JH, Bültmann M, Haas NA, Dähnert I, Alexi-Meshkisvilli V, Opitz C, Pappert D, Rossaint R, Kleber FX, Hetzer R, Lange PE (1997) Aerolosiertes Prostazyklin zur präoperativen Evaluation und postkardiochirurgischen Behandlung von Patienten mit pulmonaler Hypertension. Z Kardiol 86:71–80
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Haas, N.A., Kemke, J., Schulze-Neick, I. et al. Effect of increasing doses of magnesium in experimental pulmonary hypertension after acute pulmonary embolism. Intensive Care Med 30, 2102–2109 (2004). https://doi.org/10.1007/s00134-004-2424-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-004-2424-0