Abstract
Objective
In mechanically ventilated patients inspiratory increase in pleural pressure during lung inflation may produce complete or partial collapse of the superior vena cava. Occurrence of this collapse suggests that at this time external pressure exerted by the thoracic cavity on the superior vena cava is greater than the venous pressure required to maintain the vessel fully open. We tested the hypothesis that measurement of superior vena caval collapsibility would reveal the need for volume expansion in a given septic patient.
Design and setting
Prospective data collection for 66 successive patients in septic shock admitted in a medical intensive care unit and mechanically ventilated for an associated acute lung injury.
Measurements and results
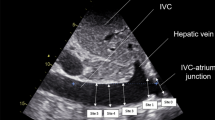
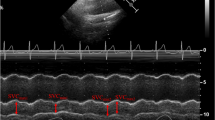
We simultaneously measured superior vena caval collapsibility by echocardiography and cardiac index by the Doppler technique at baseline and after a 10 ml/kg volume expansion by 6% hydroxyethyl starch in 30 min. The threshold superior vena caval collapsibility of 36%, calculated as (maximum diameter on expiration−minimum diameter on inspiration)/maximum diameter on expiration, allowed discrimination between responders (defined by an increase in cardiac index of at least 11% induced by volume expansion) and nonresponders, with a sensitivity of 90% and a specificity of 100%.
Conclusions
Superior vena cava measurement should be systematically performed during routine echocardiography in septic shock as it gives an accurate index of fluid responsiveness.




Similar content being viewed by others
References
Jardin F, Fourme T, Page B, Loubières Y, Vieillard-Baron A, Beauchet A, Bourdarias JP (1999) Persistent preload defect in severe sepsis despite fluid loading: A longitudinal echocardiographic study in patients with septic shock. Chest 116:1354–1359
Parker M Shelhamer J, Bacharach S, Gren M, Natanson C, Frederick T, Damske B, Parrillo J (1984) Profound but reversible myocardial depression in patients with septic shock. Ann Intern Med 100:483–490
Jardin F, Brun-Ney D, Auvert B, Beauchet A, Bourdarias JP (1990) Sepsis-related cardiogenic shock. Crit Care Med 18:1055–1060
Parrillo J (1993) Pathogenic mechanism of septic shock. N Engl J Med 328:1471–1477
Task Force of the American College of Critical Care Medicine, Society of Critical Care Medicine (1999) Practice parameters for hemodynamic support of sepsis in adult patients in sepsis. Crit Care Med 27:639–660
Schneider A, Teule G, Groeneveld A, Nauta J, Heidendal G, Thijs L (1988) Biventricular performance during volume loading in patients with early septic shock, with emphasis on the right ventricle: a combined hemodynamic and radionuclide study. Am Heart J 116:103–112
Krausz M, Perel A, Eimerl D, Cotev S (1977) Cardiopulmonary effects of volume loading in patients in septic shock. Ann Surg 185:429–434
Bendjelid K, Romand J (2003) Fluid responsiveness in mechanically ventilated patients: a review of indices used in intensive care. Intensive Care Med 29:352–360
Michard F, Boussat S, Chemla D Anguel N, Mercat A, Lecarpentier Y, Richard C, Pinsky M, Teboul JL (2000) Relation between respiratory changes in arterial pulse pressure and fluid responsiveness in septic patients with acute circulatory failure. Am J Respir Crit Care Med 162:134–138
Vieillard-Baron A, Augarde R, Prin S, Page B, Beauchet A, Jardin F (2001) Influence of superior vena caval zone conditions on cyclic changes in right ventricular outflow during respiratory support. Anesthesiology 95:1083–1088
Vieillard-Baron A, Prin S, Chergui K, Dubourg O, Jardin F (2003) Hemodynamic instability in sepsis: bedside assessment by Doppler echocardiography. Am J Respir Crit Care Med 168:1270–1276
American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference (1992) Definition for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Crit Care Med 20:864–874
American-European Consensus Conference on ARDS (1994) Definition, mechanisms, relevant outcomes, and clinical trial coordination. Am J Respir Crit Care Med 149:818–824
Darmon PL, Hillel Z, Mogtader A, Mindich B, Thys D (1994) Cardiac output by transesophageal echocardiography using continuous-wave Doppler across the aortic valve. Anesthesiology 80:796–805
Vieillard-Baron A, Schmitt JM, Beauchet A, Augarde R, Prin S, Page B, Jardin F (2001) Early preload adaptation in septic shock? A transesophageal echocardiographic study. Anesthesiology 94:400–406
Vieillard-Baron A, Prin S, Chergui K, Dubourg O, Jardin F (2002) Echo-Doppler demonstration of acute cor pulmonale at the bedside in the medical intensive care unit. Am J Respir Crit Care Med 166:1310–1319
Fellahi JL, Jardin F (1999) Doppler echocardiography in intensive care. In: Webb A, Shapiro M, Singer M, Suter P (eds) Oxford textbook of critical care. Oxford University Press, Oxford, pp 1145–1153
Kimchi A, Ellrodt G, Berman D, Riedinger M, Swan H, Murata G (1984) Right ventricular performance in septic shock: a combined radionuclide and hemodynamic study. J Am Coll Cardiol 5:945–951
Vincent JL, Reuse N, Frank N, Contempré B, Kahn R (1989) Right ventricular dysfunction in septic shock: assessment by measurements of right ventricular ejection fraction using thermodilution technique. Acta Anaesthesiol Scand 33:34–38
Parker M, McCarthy K, Ognibene F, Parrillo J (1990) Right ventricular dysfunction and dilatation, similar to left ventricular changes, characterize the cardiac depression of septic shock in humans. Chest 97:126–131
Morgan B, Martin W, Hornbein T, Crawford E, Guntheroth W (1966) Hemodynamic effect of intermittent positive pressure respiration. Anesthesiology 27:584–590
Jardin F, Farcot JC, Gueret P, Prost JF, Ozier Y, Bourdarias JP (1983) Cyclic changes in arterial pulse during respiratory support. Circulation 68:266–274
Vieillard-Baron A, Chergui K, Augarde R, Prin S, Page B, Beauchet A, Jardin F (2003) Cyclic changes in arterial pulse during respiratory support revisited by Doppler Echocardiography. Am J Respir Crit Care Med 168:671–676
Versprille A (1990) The pulmonary circulation during mechanical ventilation. Acta Anaesthesiol Scand 34 [Suppl 94]:51–62
Vieillard-Baron A, Loubières Y, Schmitt JM, Page B, Dubourg O, Jardin F (1999) Cyclic changes in right ventricular output impedance during mechanical ventilation. J Appl Physiol 87:1644–1650
Author information
Authors and Affiliations
Corresponding author
Additional information
An editorial regarding this article can be found at http://dx.doi.org/10.1007/s00134-004.2362-x
Electronic Supplementary Material
Rights and permissions
About this article
Cite this article
Vieillard-Baron, A., Chergui, K., Rabiller, A. et al. Superior vena caval collapsibility as a gauge of volume status in ventilated septic patients. Intensive Care Med 30, 1734–1739 (2004). https://doi.org/10.1007/s00134-004-2361-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-004-2361-y