Abstract
Objective
To compare N-terminal pro-brain natriuretic peptide (NT-pro-BNP), procalcitonin (PCT), and troponin I (Tn I) concentrations during and after coronary artery surgery in patients with or without cardiovascular complications.
Design and setting
Prospective, comparative study of 12 months in the cardiovascular intensive care unit in a university hospital
Patients
60 adult patients undergoing coronary artery bypass grafting with the off-pump technique.
Measurements and results
Plasma NT-pro-BNP, PCT, and Tn I levels were measured before and immediately after the end of operation and on PODs 1, and 2 and 3. We defined complicated postoperative course as myocardial infarction, cardiogenic shock, arrhythmias, congestive heart failure, and death occurring after the fourth postoperative hour. Receiver operating characteristic (ROC) curve cutoff values were used to assess the ability of the three markers to predict future cardiac events. The area under ROC curve (AUC) using NT-pro-BNP to detect a cardiovascular complicated course was 0.780 at the preoperative time and 0.850 at the end of surgery. A preoperative NT-pro-BNP value of 397 pg/ml had a sensitivity of 76%, specificity of 67%, and accuracy of 74% for predicting a subsequent cardiovascular complication. An immediate postoperative NT-pro-BNP value of 430 pg/ml had a sensitivity of 80%, specificity of 77%, and accuracy of 76%. Patients with preoperative NT-pro-BNP levels less than 275 pg/ml had an excellent postoperative prognosis. Other two markers were less appropriate.
Conclusions
NT-pro-BNP levels measured before and immediately after off-pump coronary artery bypass seem to be predictive of postoperative cardiac events.
Similar content being viewed by others

Introduction
Off-pump coronary artery bypass (OPCAB) is now performed safely without cardiopulmonary bypass even in high-risk patients [1, 2]. However, occlusion of native coronary arteries and displacement of the beating heart may lead to ischemia and hemodynamic instability during the procedure, leading thus to potential postoperative cardiovascular complications. Brain natriuretic peptide (BNP) and its precursor (N-terminal pro-BNP NT-pro-BNP) are newly cardiac hormones secreted by the ventricle which have recently been considered as effective markers of severity and prognosis of acute coronary syndromes [3, 4] and heart failure [5, 6]. Procalcitonin (PCT) is known to early increase after cardiovascular surgery in patients with postoperative complications such as cardiovascular dysfunction [7, 8] or myocardial infarction [9]. Troponin I (Tn I) is also known to have a prognostic significance in unstable angina [10], in myocardial necrosis [9] and is known to be an independent predictor of in-hospital death after adult cardiac surgery [11]. Perioperative myocardial necrosis, congestive heart failure, and ventricular arrhythmias are major cardiovascular complications after heart surgery and can therefore increase the length of stay in the intensive care unit. However, further data on BNP, PCT, and Tn I induction after surgery, especially on cardiovascular complications, are not yet compiled.
The aim of our study was to investigate the relationships between NT-pro-BNP, PCT, and Tn I plasma concentrations in patients with uncomplicated and complicated postoperative cardiovascular courses occurring after OPCAB.
Methods
Patients
After obtaining approval from the university ethics committee and written informed consent, 65 consecutive eligible patients undergoing elective OPCAB were prospectively enrolled. Sixty of them were free of active preoperative infection and inflammation to avoid any increase in PCT. Five patients were withdrawn from the study because of the presence of a preoperative infection such as urinary infection or acute bronchitis.
Preoperative left ventricular ejection fraction (LVEF) was measured by cardiac catheterization and echocardiography (Teicholz method). Recent myocardial infarction was defined as acute coronary syndrome with or without ST modification and with Tn I level modifications occurring within 6 weeks of the operation. Unstable angina was associated with acute coronary syndrome without modification in Tn I [12]. Peripheral arteriosclerosis disease included patients with a history of claudication and/or peripheral vascular surgery. Preoperative renal function was assessed by baseline serum creatinine level and creatinine clearance, calculated by the Cockroft-Gault formula. Preexistent renal impairment was defined as a baseline creatinine clearance less than 60 ml/min [13].
Anesthesia and surgical technique
Patients were premedicated with oral oxazepam 0.05 mg/kg on the night and 1 h before surgery. After preoxygenation intravenous anesthesia was induced with 0.05 mg/kg midazolam, 0.3 mg/kg etomidate, and 0.5 µg/kg sufentanil. Tracheal intubation was performed after neuromuscular blocking with 0.5 mg/kg atracurium. Anesthesia was maintained with sufentanil (0.5 µg/kg per hour), atracurium (0.5 mg/kg per hour), and sevoflurane (0.5–1.5% end-tidal concentrations). Lungs were ventilated via an endotracheal tube with a ventilator initially set to deliver a FIO2 of 0.5, a tidal volume of approx. 7–10 ml/kg, and a respiratory rate adjusted to maintain an arterial PaCO2 between 30 and 40 mmHg. All patients were monitored by electrocardiography, pulse oximetry, end-tidal carbon dioxide capnography, systemic arterial line, and right heart catheterization (Swan-Ganz catheter). Cardiac output was measured by flow-directed thermodilution pulmonary artery catheter (Opti Q, 8F, 110 cm, Abbott laboratories, North Chicago, Ill., USA). Radial artery catheterization was performed for pressure monitoring and blood sampling. Blood gas analyses were performed using a blood gas analyzer (ABL-505; Radiometer, Copenhagen, Denmark). Urinary bladder temperature was used to assess core temperature. Antibiotic prophylaxis was 1.5 g cefamandole intravenously after induction and 750 mg every 2 h throughout surgery. No antibiotic therapy was systematically administered postoperatively in the absence of any bacteriological positive sample. Hypothermia was prevented throughout surgery due to the systematic use of warming blanket. A cell saver was systematically added to minimize homologous blood transfusion.
The heparin dose was 150 IU/kg to reach an activated clotting time of more than 300 s. Surgical technique was standardized, and all procedures were performed by the same surgeon. The left internal mammary artery was attached to the left anterior descending artery, and vein grafts to other coronary arteries as appropriate in all patients. The top end anastomoses were constructed with the help of a side-biting clamp. Coronary artery immobilization was achieved with a mechanical stabilizer (Octopus 3, Medtronic, Minneapolis, Minn., USA). At the end of surgery protamine sulfate was administered intravenous to reach an activated clotting time of less than 160 s.
Postoperative management
Tracheal extubation was performed when patients met the full following criteria described in a previous study [7]. From postoperative day (POD) 1 patients received 250 mg aspirin intravenously per day during mechanical ventilation and 160 mg orally per day after extubation was performed. Usually the patients were discharged from the ICU on POD 2. Criteria of an abnormal postoperative course were recorded until POD 7. Euroscore [14] and Parsonnet index [15] were monitored on POD 1 and based on preoperative criteria.
Abnormal cardiovascular postoperative course was defined by at least one of the eight events occurring 4 h after admission in ICU: (a) systolic arterial pressure lower than 90 mmHg with low cardiac output (cardiac index <2 l min−1 m−2) and signs of hypoperfusion such as oliguria; (b) need for catecholamines for cardiovascular support (dobutamine >5 µg kg−1 min−1 or any amount of epinephrine or norepinephrine longer than 6 h); (c) postoperative myocardial infarction defined as a maximal creatine kinase MB fraction level higher than 100 IU l−1 associated electrocardiographic modifications and segmental hypokinesia at the echocardiography; (d) congestive heart failure defined by fluid retention and persistent chest infiltration; (e) atrial fibrillation longer than 15 min with hemodynamic instability requiring electrical or pharmacological cardioversion; (f) ventricular fibrillation or tachycardia requiring electrical cardioversion; (f) operative mortality occurring within 30 days of the operation.
Blood samples
Blood samples were collected 30 min after induction of intravenous anesthesia before surgery (t 0), 10 min (t 1) and 4 h after the end of the surgery (t 2), and on the first (t 3), second (t 4), and third (t 5) days postoperatively at 5 a.m. Blood samples were collected from the cannulated radial artery and immediately centrifuged for 20 min. Plasma samples frozen at –80°C were then stable for assays for longer than 20 days after sampling, and all samples were measured within 2 weeks after sampling. To avoid any influence on medical decision regarding treatment or extubation the surgeon and anesthesists were blinded to NT-pro-BNP, PCT, and Tn I dose results. Biologists were blinded to postoperative course of patients included during their intensive care unit stay.
NT-pro-BNP, PCT, and cardiac Tn I determinations
BNP or its precursor NT-pro-BNP are cardiac hormones recently considered as the most effective markers of severity and prognosis of acute coronary syndromes [3, 4] and congestive heart failure [5, 6]. NT-pro-BNP was chosen here because of its greatest stability in blood at ambient temperature and because of its longest plasmatic half life (120 vs. 20 min for BNP). PCT is known to early increase after cardiovascular surgery in patients with postoperative complications such as cardiovascular dysfunction [7, 8] or myocardial infarction [9]. Tn I is also known to have a prognostic significance in acute coronary syndromes with or without ST elevation [9, 10] and is an independent predictor of in-hospital death after adult cardiac surgery [11]. Cardiac Tn I and PCT levels are routinely determined at the perioperative time in our center.
NT-pro-BNP concentrations were measured with a sandwich immunoassay using polyclonal antibodies that recognize epitopes located in the N-terminal part (1–76) of pro-BNP (1–108). An electrochemiluminescence immunoassay was performed using an Elecsys analyzer (Roche Diagnostics, Mannheim, Germany). The intra-assay coefficient of variation was 2.7% at 175 pg/ml and 1.9% at 1068 pg/ml and the interassay coefficient of variation 3.0% at 175 pg/ml and 2.6% at 1068 pg/ml. PCT concentrations in serum were measured by immunoluminometric assay with the commercially available LUMI test PCT (B.R.A.H.M.S Diagnostica, Berlin, Germany). The interassay precision of the kit was 6–10%; the lower limit detection was 0.1 ng/ml. Cardiac Tn I was measured with an immunoassay by using the Stratus II autoanalyzer (Dade Behring, Paris France; lowest detection limit at 0.04 µg/ml with an imprecision of 10% coefficient of variation at 0.2 µg/ml as determined in our laboratory. The 99th percentile of a reference population is 0.07 µg/ml. The receiver operating characteristic (ROC) curve medical decision cutoff value for myocardial infarction was 0.6 µg/ml with a total imprecision of 8%.
Statistical analysis
The association between postoperative cardiovascular complications and predictive or prognostic factors were analyzed using the χ2 test or Fisher’s exact test when appropriate for discrete variables or using the Mann-Whitney U test for continuous variables. For continuous variables correlations were assessed using Spearman’s nonparametric coefficient. Information coming from NT-pro-BNP, PCT, and Tn I to estimate complication risk was assessed by ROC curves. Cutoff values, defined as the threshold values maximizing the sum of sensitivity and specificity, were determined for each score with ROC curves. The areas under the curve were calculated and compared by the Hanley-McNeil nonparametric method [16]. We analyzed the variation over time in NT-pro-BNP, PCT, and Tn I according to the complication status of individual patients using analysis of variance for repeated measures with complication as explicative factor. For all tests p values less than 0.05 were considered as statistically significant. Statistical analysis was performed using SPSS software, version 11.1 for Windows.
Results
Clinical and demographic features are given in Table 1. There was no significant difference between preoperative patients characteristics, except a greater number of diabetic patients (p=0.043) and a trend towards a lower LVEF (p=0.09) in the group with complications. As expected, the 21 patients with complications had more frequent cardiovascular complications, induced prolonged duration of mechanical ventilation, and stay in ICU (Table 2). Postoperative inotropic support was significantly higher in patients with complications (Table 2).
Kinetics of NT-pro-BNP, PCT, and Tn I after uncomplicated OPCAB
Figures 1, 2, and 3 show time course of NT-pro-BNP, PCT, and Tn I after uncomplicated coronary artery bypass grafting in 39 consecutive patients. Plasma NT-pro-BNP levels were normal before surgery (275±170 pg/ml), increased progressively 4 h after surgery (307±270 pg/ml), peaked at 48 h postoperatively (T4; 945±351 pg/ml) and began to decrease at 72 h (T5). PCT peaked at 48 h (T4) from 0.10±0.09 ng/ml preoperatively to 0.23±0.22 ng/ml on POD 2 and returned to baseline on POD 3 (T5). Cardiac Tn I peaked at T2 (0.45±0.60 µg/l) and returned to baseline values at 72 h.
Time course of plasma concentration of NT-pro-brain natriuretic peptide (NT-pro-BNP). Uncomplicated Patients with normal postoperative course after OPCAB; complicated patients with abnormal postoperative course after OPCAB. T0 Level 30 min after induction of intravenous anesthesia before surgery; T1 10 min after the end of surgery; T2 4 h after the end of the surgery; T3 POD 1; T4 POD 2; T5 POD 3. Given are median, quartile (box), and 10/90 percentiles (whiskers)
Time course of plasma concentration of procalcitonin (PCT). Uncomplicated Patients with normal postoperative course after OPCAB; complicated patients with abnormal postoperative course after OPCAB. T0 Level 30 min after induction of intravenous anesthesia before surgery; T1 10 min after the end of surgery; T2 4 h after the end of the surgery; T3 POD 1; T4 POD 2; T5 POD 3. Given are median, quartile (box), and 10/90 percentiles (whiskers)
Time course of plasma concentration of troponin I). Uncomplicated Patients with normal postoperative course after OPCAB; complicated patients with abnormal postoperative course after OPCAB. T0 Level 30 min after induction of intravenous anesthesia before surgery; T1 10 min after the end of surgery; T2 4 h after the end of the surgery; T3 POD 1; T4 POD 2; T5 POD 3. Given are median, quartile (box), and 10/90 percentiles (whiskers)
NT-pro-BNP, PCT and Tn I concentrations after complicated surgery
Figures 1, 2, and 3 represent plasma NT-pro-BNP, PCT and Tn I concentrations measured in complicated patients. Plasmatic NT-pro-BNP concentrations in the patients with complications were significantly higher than in those without complications (p=0.005) for each time of the study. Plasma concentrations of PCT and Tn I also did not differ between the patients with and those without complications (respectively p=0.158 and p=0.07). Finally, two patients in with complications died during hospitalization, and NT-pro-BNP was significantly and rapidly higher in these patients (>7000 pg/ml at 48 h). The first death occurred on POD 4 and was directly related to a cardiovascular complication (cardiogenic shock following myocardial infarction). The second patient died from infectious acute respiratory distress syndrome on POD 12; however, his immediate postoperative course was characterized by hemodynamic instability and pulmonary edema associated with left ventricular diastolic dysfunction.
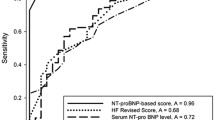
Sensitivity and specificity for the various cardiovascular complications were combined at different concentrations of NT-pro-BNP by ROC analysis (Figs. 4 and 5). The AUC for cardiovascular complications was 0.780 at T0 (p<0.001; CI 95% 0.660–0.889), 0.850 at T1 (p<0.001; CI 95% 0.710–0.950), and 0.893 at T2 (p<0.0001; CI 95% 0.734–0.971; Table 3). The AUC for PCT was 0.506 at T0 (p=0.864; CI 95% 0.337–0.694), 0.654 at T1 (p=0.026; CI 95% 0.541–0.860), and 0.710 (p=0.04; CI 95% 0.561–0.874) at T2 for PCT. The value for Tn 1 was 0.585 at T0 (p=0.253; CI 95% 0.432–0.778), 0.720 at T1 (p=0.007; CI 95% 0.590–0.892), and 0.722 at T2 (p=0.009; CI 95% 0.591–0.901; Table 3, Figs. 4, 5, 6).
Correlations between NT-pro-BNP and preoperative physical findings and diagnostic tests
Preoperative values of NT-pro-BNP (T0) were significantly correlated with echographic left ventricular end-diastolic diameter (r=0.61, p<0.001, n=60) and New York Heart Association (NYHA) score (p=0.023) and were inversely correlated with preoperative LVEF (r=−0.64, p<0.001). The correlation between preoperative NT-pro-BNP values and LVEF was significant both in patients without postoperative complications (r=−0.66, p=0.003) and in those with cardiovascular complications (r=−0.62, p=0.002). There was no significant correlation between preoperative NT-pro-BNP values and preoperative renal function (serum creatinine, r=−0.004, p=0.491; creatinine clearance, r=−0.094, p=0.28, n=60). No correlation was found between NT-pro-BNP at t 0 and preoperative scoring systems.
Discussion
This study was designed to examine the plasma levels of NT-pro-BNP, Tn I, PCT in patients with and in those without cardiovascular events complicating the postoperative course after OPCAB. We found that high preoperative NT-pro-BNP values predict postoperative cardiovascular complications and may therefore provide an indication of which patients are at risk for these types of complications.
Correlation between NT-pro-BNP and preoperative left ventricular ejection fraction
Our data confirm that plasma NT-pro-BNP concentrations are raised in cardiac disease in proportion to the severity of left ventricular dysfunction [17, 18], and that the preoperative plasma levels of NT-pro-BNP are valuable predictors of the postoperative course. In a previous study we demonstrated that patients with lowest preoperative LVEF developed a highest incidence of postoperative severe systemic inflammatory response syndrome associated with cardiovascular dysfunction [7]. This information complements the powerful body of published evidence linking NT-pro-BNP concentrations to hemodynamic and echographic state in heart diseases [5, 6, 19, 20, 21]. Plasma NT-pro-BNP concentrations are also seen as indicators of recovery of the left ventricular function after coronary surgery [22].
Correlation between preoperative NT-pro-BNP and NYHA status
In this study preoperative plasma NT-pro-BNP concentrations were significantly correlated with disease severity and with NYHA classification. Although the NYHA classification is correlated with clinical symptoms, the fact that a subjective classification is still the major means to stage congestive heart failure remains a concern. Because NT-pro-BNP concentrations have been shown to be closely correlated to end-diastolic pressure [20, 21], which in turn are closely correlated to the dyspnea, a chief symptom of congestive heart failure, it is not surprising that NT-pro-BNP concentrations increase as well as NYHA status.
Plasma NT-pro-BNP concentrations and renal function
No previous study has evaluated NT-pro-BNP levels in patients with coronary artery disease and without dialysis-dependent chronic renal failure. In this study no significant correlation was found between preoperative plasma NT-pro-BNP concentrations and creatinine clearance. This marker could also be helpful for management of cardiovascular complications in patients without dialysis-dependent chronic renal failure. In patients requiring renal dialysis one recent study found that plasma NT-pro-BNP levels in patients with coronary artery disease are significantly higher than those without any coronary artery disease and are significantly correlated with LVEF, end-diastolic volume index, and end-systolic volume index determined by left ventriculography [23]. One other study demonstrated that NT-pro-BNP is not a useful reference for management of cardiovascular complications in patients with dialysis-dependent chronic renal failure [24]. In our study none of the 60 patients had dialysis-dependent chronic renal failure.
Comparison between NT-pro-BNP, PCT, and cardiac Tn I
PCT and Tn I are routinely determined in our center. However, these two markers were also less discriminant than NT-pro-BNP in this current study. Therefore the data suggest that a preoperative NT-pro-BNP cutoff of 400 pg/ml provides a good prediction of postoperative cardiovascular complications. The identification of clinical cardiovascular complications by the diagnostic threshold was especially beneficial because the sensitivity was 76% for patients with postoperative complicated course. The AUC in the ROC analysis for cardiovascular complications was 0.780, significantly different from that for PCT and Tn I. The mechanism of production of BNP is also unclear. Perhaps subacute preoperative myocardial ischemia increases regional ventricular wall stretch owing to local depression of myocardial contraction. Mechanical stretch could therefore stimulate BNP secretion [25]. The second possible mechanism is a preoperative left ventricular diastolic dysfunction due to systemic hypertension or diabetes mellitus. One clinical study comparing Doppler velocity recordings and BNP levels has suggested that BNP predicts diastolic abnormalities in patients with normal systolic function [21]. In our study, however, patients with restrictionlike filling patterns on echocardiography were not significantly more numerous among those with complications.
Study limitations
The aim of this study was to determine whether NT-pro-BNP, Tn I, and PCT concentrations can serve as predictors of cardiovascular complications following OPCAB. Because our study covered a short period, we did not evaluate the role of these hormones in predicting long-term prognosis and in particular the overall impact of the procedure on long-term mortality, for which longitudinal studies are advisable in a larger group of patients. The population studied was homogeneous, but the limited number of patients associated with the heterogeneous postoperative cardiovascular complications did not allow us to determine the accuracy of plasmatic NT-pro-BNP levels to be predictive for each type of cardiovascular complication. The first NT-pro-BNP dose was administered 30 min after the induction of anesthesia. Therefore mechanical ventilation could have altered the results of this first sample. To our knowledge, however, no study has previously demonstrated this association.
In summary, delineating the postoperative course after coronary artery bypass grafting can be difficult.
The current findings confirm that NT-pro-BNP levels are predictive for complicated cardiovascular course. Thus NT-pro-BNP levels, more than PCT or Tn I values, are valuable in risk stratification following OPCAB.
References
Mehta Y, Juneja R (2002) Off-pump coronary artery bypass grafting: new developments but a better outcome? Curr Opin Anaesthesiol 15:9–18
Demaria RG, Carrier M, Fortier S, Martineau R, Fortier A, Cartier R, Pellerin M, Hébert Y, Bouchard D, Pagé P, Perrault LP (2002) Reduced mortality and strokes with off-pump coronary artery bypass grafting surgery in octogenarians. Circulation 106:5–10
Lemos JA de, Morrow DA (2002) Brain natriuretic peptide in acute coronary syndromes. Ready for clinical application? Circulation 106:2868–2870
Lemos JA de, Morrow DA, Bentley JH, Omland T, Sabatine MS, McCabe C, Hall C, Cannon CP, Braunwald E (2001) The prognostic value of B-type natriuretic peptide in patients with acute coronary syndromes. N Engl J Med 345:1014–1021
Selvais PL, Donckier JE, Robert A, Laloux O, Linden F van, Ahn S, Ketelslegers JM, Rousseau MF (1998) Cardiac natriuretic peptides for diagnosis and risk stratification in heart failure: influence of left ventricular dysfunction and coronary artery diseases on cardiac hormonal activation. Eur J Clin Invest 28:636–642
Wieczorek SJ, Wu AH, Christenson R, Krishnaswamy P, Gottlieb S, Rosano T, Hager D, Gardetto N, Chiu A, Bailly KR, Maisel A (2002) A rapid B-type natriuretic peptide assay accurately diagnoses left ventricular dysfunction and heart failure: a multicenter evaluation. Am Heart J 144:834–839
Kerbaul F, Guidon C, Lejeune PJ, Mollo M, Mesana T, Gouin F (2002) Hyperprocalcitonemia is related to postoperative severe SIRS associated with cardiovascular dysfunction after coronary artery bypass graft surgery. J Cardiothorac Vasc Anesth 16:47–53
Meisner M, Rauschmayer C, Schmidt J, Feyrer R, Cesnjevar R, Bredle D, Tschaikowsky K (2002) Early increase of procalcitonin after cardiovascular surgery in patients with postoperative complications. Intensive Care Med 28:1094–1102
Lecharny JB, Khater D, Bronchard R, Philip I, Durand G, Desmonts JM, Dehoux M (2001) Hyperprocalcitonemia in patients with perioperative myocardial infarction after cardiac surgery. Crit Care Med 29:323–325
Bertinchant JP, Laperche T, Polge A, Raczka F, Beyne P, Ledermann B, Himbert D, Pernel I, Nigond J, Cohen-Solal A (1997) Prognostic significance of early raised cardiac troponin I in unstable angina. Contribution to the identification of a high-risk sub-group. Arch Mal Coeur Vaiss 90:1615–1622
Lasocki S, Provenchère S, Benessiano J, Vicaut E, Lecharny JB, Desmonts JM, Dehoux M, Philip I (2002) Cardiac troponin I is an independent predictor of in-hospital death after adult cardiac surgery. Anesthesiology 97:405–411
Joint European Society of Cardiology/American College of Cardiology Committee for the Redefinition of Myocardial Infarction (2000) Myocardial infarction redefined—a consensus document. Eur Heart J 21:1502–1513
Provenchère S, Plantefève G, Hufnagel G, Vicaut E, Vaumas C de, Lecharny JB, Depoix JP, Vrtovsnik F, Desmonts JM, Philip I (2003) Renal dysfunction after cardiac surgery with normothermic cardiopulmonary bypass: incidence, risk factors, and effect on clinical outcome. Anesth Analg 96:1258–1264
Nashef SAM, Roques F, Michel P, Gauducheau E, Lemeshow S, Salamon R, the EuroSCORE study group (1999) European system for cardiac operative risk evaluation (EuroSCORE). Eur J Cardiothorac Surg 16:9–13
Parsonnet V, Dean D, Bernstein AD (1989) A method of uniform stratification of risk for evaluating the results of surgery in acquired adult heart disease. Circulation 79 (Suppl I):I3–I12
Hanley JA, McNeil BJ (1983) A method of comparing the areas under receiving operating curves derived from the same cases. Radiology 148:839–843
Yoshimura M, Yasue H, Okumura K, Ogawa H, Jougasaki M, Mukoyama M, Nakao K, Imura H (1993) Different secretion patterns of atrial natriuretic peptide and brain natriuretic peptide in patients with congestive heart failure. Circulation 87:464–469
Clerico A, Lervasi G, Del Chicca MG, Emdin M, Maffei S, Nannipieri M, Sabatino L, Forini F, Manfredi C, Donato L (1998) Circulating levels of cardiac natriuretic peptides (ANP and BNP) measured by highly sensitive and specific immunoradiometric assays in normal subjects and in patients with different degrees of heart failure. J Endocrinol Invest 21:170–179
Yamamoto K, Burnett JC, Jougasaki M, Nishimura MA, Bailey KR, Saito Y, Nakao K, Redfield MM (1996) The relative value of natriuretic peptides as markers for detecting abnormal ventricular structure and function. J Am Coll Cardiol 69A:721–723
Choy AM, Darbar D, Lang CC, Pringle TH, McNeill GP, Kennedy NS, Struthers AD (1994) Detection of left ventricular dysfunction after acute myocardial infarction: comparison of clinical, echocardiographic, and neurohormonal methods. Br Heart J 72:16–22
Lubien E, DeMaria A, Krishnaswamy P, Clopton P, Koon J, Kazanegra R, Gardetto N, Wanner E, Maisel AS (2002) Utility of B-natriuretic peptide in detecting diastolic dysfunction: comparison with Doppler velocity recordings. Circulation 5:595–601
Chello M, Mastroroberto P, Perticone F, Cirillo F, Bevacqua E, Olivito S, Covino E (2001) Plasma levels of atrial and brain natriuretic peptides as indicators of recovery of left ventricular systolic function after coronary artery bypass. Eur J Cardiothorac Surg 20:140–146
Nishikimi T, Futoo Y, Tamano K, Takahashi M, Suzuki T, Minami J, Honda T, Uetake S, Asakawa H, Kobayashi N, Horinaka S, Ishimitsu T, Matsuoka H (2001) Plasma brain natriuretic peptide levels in chronic hemodialysis patients: influence of coronary artery disease. Am J Kidney Dis 37:1201–1208
Haug G, Metzele A, Steffgen J, Kochs M, Hombach V, Grunert A (1994) Increased brain natriuretic peptide and atrial natriuretic peptide plasma concentration in dialysis-dependent chronic renal failure and in patients with elevated left ventricular filling pressure. Clin Investig 72:430–434
Nakao K, Mukoyama M, Hosoda K, Suga S, Ogawa Y, Saito Y, Shirakami G, Arai H, Jougasaki M, Imura H (1991) Biosynthesis, secretion, and receptor selectivity of human brain natriuretic peptide. Can J Physiol Pharmacol 69:1500–1506
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kerbaul, F., Collart, F., Giorgi, R. et al. Increased plasma levels of pro-brain natriuretic peptide in patients with cardiovascular complications following off-pump coronary artery surgery. Intensive Care Med 30, 1799–1806 (2004). https://doi.org/10.1007/s00134-004-2299-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-004-2299-0