Abstract
Objective
Pseudomonas aeruginosa-induced lung injury is characterized not only by the alteration in lung fluid movement but also by apoptosis of lung epithelial and endothelial cells. We studied whether inhibition of apoptosis using a broad spectrum caspase inhibitor, benzyloxycarbonyl-Val-Ala-Asp fluoromethylketone (Z-VAD.fmk), would affect lung fluid balance in rat P. aeruginosa pneumonia.
Methods
Z-VAD.fmk (3 mg/kg) was administered intravenously simultaneously with P. aeruginosa intratracheal instillation (0.5 ml/kg, 2×109 CFU/ml). Apoptosis was evaluated with the TUNEL technique, cytoplasmic oligonucleosome assay, and caspase 3 activation. To evaluate lung permeability, extravascular plasma equivalent (EPE) and lung wet to dry weight ratio (W/D) were measured 4 h after intratracheal instillation of P. aeruginosa.
Results
We found an increase of lung apoptosis 4 h after P. aeruginosa instillation: cytoplasmic oligonucleosome assay increased from 3.17±0.78 to 26.82±4.67 OD×1000/mg of proteins/ml, Z-VAD.fmk administration decreased this parameter to 10.3±2.98 OD×1000/mg of proteins/ml. Caspase 3 levels followed the same pattern. Apoptosis involved both epithelial cells and endothelial cells. Endothelial permeability was increased after Pseudomonas instillation: W/D increased from 3.75±0.28 in the Co group to 4.42±0.23 in the Pn group; EPE was also higher in the Pn group compared with the Co group (0.125±0.04 and 0.002±0.01 ml, respectively). Both of these parameters were improved after Z-VAD.fmk administration; W/D decreased to 3.36±0.25 and EPE to 0.02±0.02 ml.
Conclusion
Apoptosis occurs in the early phase of P. aeruginosa pneumonia. Administration of Z-VAD.fmk significantly decreases DNA fragmentation and caspase 3 levels. This is associated with an improvement of endothelial permeability and lung fluid balance.
Similar content being viewed by others
Introduction
Bacterial pneumonia is a leading cause of morbidity and mortality among critically ill patients [1]. P. aeruginosa is the most frequent Gram-negative organism associated with nosocomial pneumonia in hospitalized patients [2, 3]. In a recent investigation, patients with ventilator-associated pneumonia (VAP) infected with P. aeruginosa had the highest rate of acute lung injury (ALI) [4], suggesting that P. aeruginosa was associated with an increased morbidity and mortality compared with other pathogens.
In its early stage, ALI is characterized by the association of edema, exudation, and hyaline membrane in the alveolar space due to a major increase in the permeability of the alveoli–capillary membrane. Lung fluid balance is regulated by alveolar and lung liquid clearance: alveolar clearance depends on the active sodium transport from the alveoli to the interstitium. This transport relies on sodium channels and the Na, K-ATPase [5, 6, 7, 8]. Bacteria-induced acute lung injury is characterized by an alteration in lung fluid balance leading to an increase in extravascular lung water [9, 10]. We have previously shown that P. aeruginosa instillation could decrease lung liquid clearance both at the early phase and after 24 h in a rat model of pneumonia [10]. There is actually a solid line of evidence that the capacity of maintaining alveolar active fluid transport is highly correlated with a favorable outcome in patients with acute lung injury [11, 12].
A characteristic feature of ALI is a widespread destruction of the alveolar epithelium, with morphological and physiological evidence of severe epithelial injury in distal airways and alveoli, although the exact mechanism of cell death is uncertain [12]. There is a growing body of experimental and clinical evidence that apoptosis of lung cells may play an important role in the mechanisms of injury to these cells. Mantell et al. showed in three distinct models of ALI (hyperoxia, oleic acid and bacterial pneumonia) that apoptosis was clearly a feature of ALI [13]. Moreover, P. aeruginosa instilled into the airspaces has been shown to induce apoptosis of lung epithelial cells [14, 15, 16]. The mechanisms by which bacteria induce apoptosis in lung epithelial cells are complex. Recent data suggest that P. aeruginosa may activate the Fas/FasL pathway in epithelial cells [16]. If there is a good amount of literature on bacteria-induced epithelial cell apoptosis, only a few data can be recovered on endothelial cells. Endothelial cell apoptosis has been studied in LPS or TNF-treated mice in vivo; LPS induced a disseminated form of endothelial apoptosis which was mediated sequentially by TNF and ceramide generation [17].
Most of the biochemical features of apoptosis are caused by a group of cysteine proteases called caspases (cysteine aspartate enzyme) that selectively cleave substrates at the level of an aspartate residue. The end point of the process is a progressive fragmentation of DNA by endonucleases responsible for the generation fragments of 180–200 base pairs that may be detected as a ladder on gel electrophoresis. Caspases are thought to be central executioners of the apoptotic process. In most experimental models, elimination of caspase activity will slow down or prevent apoptosis: the inhibition of caspases by benzyloxycarbonyl-Val-Ala-Asp fluoromethylketone (Z-VAD.fmk) has been shown to prevent LPS-induced apoptosis in mice [18, 19].
Our first objective was to investigate, in a rat model, whether administration of a well-known broad-spectrum caspase inhibitor Z-VAD.fmk could prevent P. aeruginosa-induced apoptosis in the lung. Apoptosis was evaluated by assessing in situ transferase-mediated dUTP nick end labeling (TUNEL) analysis, cytoplasmic oligonucleosome assay, and enzymatic activity of caspase 3. The second aim of our study was to evaluate a potential link between lung fluid balance and apoptosis inhibition in this model. Two major parameters of lung injury were considered, alveoli–capillary permeability and lung edema. We concluded that administration of Z-VAD.fmk decreased apoptosis in the lung and could, at least partially, modulate fluid transport even if apoptosis is not the only mechanism involved in P. aeruginosa-induced lung injury.
Materials and methods
Animals
Specific pathogen-free Sprague-Dawley rats (n=101; 280–300 g, Centre d’élevage Dépré, St. Doulchard, France) were housed in the Lille University Animal Care Facility and allowed food and water ad lib. All experiments were performed with approval of the Lille Institutional Animal Care and Use Committee.
Intratracheal instillation of P. aeruginosa
P. aeruginosa (PaO1 strain) was incubated in 125 ml of tryptic soy broth at 37°C in a rotating shaking water bath for 8 h. The resulting bacterial suspension was at 2×109 CFU/ml. Pneumonia was produced according to the method described by Pennington and Ehrie [20]. Under short ether anesthesia, a small midline incision was made on the neck ventral. Using a 28-G needle, 0.5 ml/kg of bacterial suspension was instilled in the trachea followed by injection of 0.5 ml of air. Once awake, the rats were returned to their cages, allowed to recover and access food and water. Control animals received an equal volume of saline using the same procedure.
Z-VAD.fmk intravenous administration
Animals were anesthetized with ether (Mallinkrodt, Paris, France). Z-VAD.fmk (Z-val-Ala-DL-Asp-fluoromethylketone, Bachem, Voisin le Bretonneux, France) prepared in 1% dimethyl sulfoxide (DMSO) was injected with a 28-G needle in the dorsal penile vein for a dose of 3 mg/kg. An equal volume of saline (0.5 ml) was intravenously administered for controls.
Histology
After a vascular washout with isotonic saline, lungs from each experimental group were fixed 24 h in a 4% paraformaldehyde buffered solution (pH=7.4) and embedded in paraffin. Serial lung sections (4 µm thick) were stained with hematoxylin–eosin–safran to allow analysis of inflammatory cells and parenchymal lesions.
Diffuse alveolar damage was evaluated using a blind histological scoring technique by two blinded pathologists.
Immunohistochemistry
The terminal deoxynucleotidyl (TUNEL)method was performed on unstained paraffin sections. The “in situ cell death detection kit” (Roche, Mannheim, Germany) was used according to manufacturer’s instructions with minor modifications. For alveolar apoptosis detection, the slides were incubated with biotine avidine inhibitor followed by a nick end labeled with biotinylated-dUTP catalyzed by TdT (1.8 µl of 17 UI/µl). For endothelial apoptosis detection, the slides were incubated with the TUNEL reaction mixture (TdT in the label solution 1:80 final concentration; Roche, Mannheim, Germany) for 1 h at 37°C. At the end of the TUNEL reaction, samples were also labeled with a peroxydase conjugated anti-FITC antibody (Converter-POD, 1:2 in distilled water; Roche, Mannheim, Germany), revealed by DAB substrat (Pierce, Perbio Science, Ilinois). Counterstaining of nuclei was performed with methyl green.
Cytoplasmic oligonucleosome assay
The cell death detection ELISA plus kit (Roche, Mannheim, Germany) was used according to the manufacturer’s instructions. Briefly, small pieces (40–50 mg) of lung were homogenized in the provided lysis buffer 45 min at room temperature, followed by centrifugation 10 min at 2000 rpm. Protein level was determined on the supernatants. Twenty microliters of the supernatant was subjected immediately to the ELISA test. Results are expressed as OD×1000/concentration of proteins (mg of proteins/ml).
Measurement of caspase 3 activity
Dissected lungs were washed in ice-cold Krebs-Henseleit (KH) buffer solution and immediately frozen in liquid nitrogen. Frozen tissue was subsequently ground into a powder using a mortar and pestle and resuspended with ice-cold lysis buffer containing 1 mM PMSF, 10 µg/ml aprotinin, and leupeptin. Homogenates were centrifuged and the supernatants were used. An amount of 100 µg of proteins were diluted with assay buffer and incubated at 25°C with the colorimetric substrates Ac-DEVD-pNA (Biomol, Plymouth, PA), 200 µM final concentration, in 96-well microtiter plates. Cleavage of the p-nitroaniline (p-NA) dye from the peptide substrate was determined by the measure of absorbance of p-NA at 405 nm in a microplate reader Digiscan (Asys Hitech, Cincinnati, Ohio).
Measurement of lung fluid movement and permeability
Surgical preparation and ventilation
Sprague-Dawley male rats were anesthetized with pentobarbital (Sanofi, Libourne, France). An endotracheal tube (PE-220) was inserted through a tracheostomy. The rats were ventilated with a constant volume pump (Harvard Apparatus, South Natick, Mass.) with an inspired O2 fraction of 1.0, a peak airway pressure of 8–12 cm H2O, and a positive end-expiratory pressure of 2 cm H2O. A catheter (PE-50) was inserted into the left carotid artery to monitor systemic arterial pressure and obtain blood samples. Arterial blood gases were measured at a 1-h interval. The arterial PO2 was used to quantify the oxygenation deficit [21, 22, 23]. Samples from instilled protein solution, from final distal airspace fluid, and from initial and final blood were collected to measure total protein concentration with an automated analyzer (Hitachi 917, Tokyo, Japan).
Preparation of instilled solution
The test solution, used for alveolar instillation, was prepared as follows: a 5% bovine albumin solution was prepared using Ringer lactate and was adjusted with NaCl to be isoosmolar with the rat circulating plasma [21, 22, 23]. 1µCi of 125I-labeled human serum albumin (125I-HSA; CIS biointernational, Gif sur Yvette, France) was added to the 5% albumin solution.
General protocol
After the surgical preparation, hemodynamic parameters were allowed to stabilize for 1 h. The rat was then placed in left decubitus position. A vascular tracer, 1µCi of 131I-labeled human albumin, was injected into the bloodstream to calculate the flux of plasma protein into the lung interstitium [22, 23]. This tracer 131I-HSA was prepared in our institution according to a standardized technique [24]. To calculate the flux of protein from the airspaces into the circulating plasma, the instilled solution described above was instilled 30 min later into the left lung over a 2-min period, using a 1-ml syringe and a polypropylene tube (0.5 mm ID) introduced into the endotracheal tube [21]. One hour after the instillation, the abdomen was opened and the rat was exsanguinated. Urine was sampled for radioactivity counts. The lungs were removed through a sternotomy, and fluid from the distal airspaces was obtained by passing a propylene tube (0.5 mm ID) into a wedged position in the left lower lobe. The total protein concentration and the radioactivity of the liquid sampled were measured. Right and left lungs were homogenized separately for water-to-dry-weight ratio measurements and radioactivity counts.
Albumin flux across alveoli–capillary barrier
We estimated the quantity of plasma that entered the instilled lungs by measuring the transfer of the vascular protein tracer, 131I-albumin, into the extravascular spaces of the instilled lung using the equation of plasma equivalents. The clearance of plasma into the extravascular spaces of the lung was estimated as previously described [9].
Extravascular lung water
Extravascular lung water was determined as it has been described previously by calculating the water-to-dry-weight ratio [9, 10].
Experimental protocol
For all experiments, parameters were measured 4 h after the instillation of P. aeruginosa into the lungs. Four groups were studied: (a) Control (Co), i.e., intratracheal and intravenous injection of isotonic saline 0.5 and 1 ml/kg, respectively; (b) Z-VAD.fmk (ZVAD), i.e., intratracheal injection of isotonic saline 0.5 ml/kg and intravenous injection of Z-VAD.fmk 3 mg/kg; (c) Pneumonia (Pn), i.e., intratracheal injection of PaO1 0.5 ml/kg of 2×109 CFU and intravenous injection of isotonic saline 1 ml/kg; and (d) Pneumonia with Z-VAD.fmk (ZPn), i.e., intratracheal injection of PaO1 0.5 ml/kg of 2×109 CFU and intravenous injection of Z-VAD.fmk 3 mg/kg.
Statistical analysis
Results are presented as mean±SD. Data were analyzed using Kruskal-Wallis test and the Mann-Whitney test when appropriate. The p values less than 0.05 were considered as statistically significant.
Detailed methodology
The detailed methods are available in the online supplement.
Results
P. aeruginosa induces apoptosis, Z-VAD.fmk decreases both alveolar and endothelial cells induced apoptosis.
Histological sections showed a major destruction of the alveoli architecture 4 h after P. aeruginosa administration, the injury was mainly perihilar which is consistent with the administration mode (intra-tracheally). The histological injury score calculated increased from 0.2±0.1 in the Co group to 8.5±2.4 in the Pn group (p<0.05). In injured zones, alveoli were filled with fluid and inflammatory cells: PMN and macrophages (Fig. 1). The percentage of TUNEL-positive cells in the Pn group was increased compared with the Co group (Fig. 2). The oligonucleosome assay showed an increased oligonucleosomal fragmentation in the Pn group compared with the Co group (Table 1). Consistent with these data, caspase 3 activity in pneumonic lungs was significantly increased compared with controls (Table 1).
Morphologic assessment of P. aeruginosa -induced lung injury (×40). A Hematoxylin–eosin stained control lungs (Co). B Hematoxylin–eosin stained lungs 4 h after P. aeruginosa infection (Pn). C Hematoxylin–eosin stained lungs 4 h after P. aeruginosa infection and Z-VAD.fmk injection (ZPn). D Hematoxylin–eosin stained lungs 4 h after Z-VAD.fmk injection
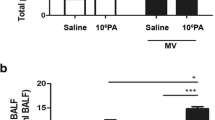
Effect of Z-VAD-fmk on apoptosis of A epithelial and B endothelial cells 4 h after Pseudomonas aeruginosa induced lung injury: control group (Co); intratracheal Pseudomonas aeruginosa and intravenous PBS co administration (Pn); intratracheal PBS and intravenous Z-VAD.fmk co administration (Z-VAD); and intratracheal Pseudomonas aeruginosa and intravenous Z-VAD.fmk co administration (ZPn). *p<0.05 vs the Co group
In Z-VAD.fmk-treated pneumonic animals, lung injury was observed, although it was less extensive compared with the Pn group. Inflammatory cells were still present, but edema was limited to the interstitium, the injury score was significantly lower than the Pn group (3.2±0.9 vs 8.5±2.4; p<0.05). After Z-VAD administration alone, the score remained comparable to that of the Co group (0.4±0.2 vs 0.2±0.1; p=NS). The percentage of TUNEL-positive cells was significantly decreased compared with the Pn group (Fig. 2). These results were confirmed by the oligonucleosome assay, which showed a decrease of oligonucleosomal fragmentation (Table1). Measurement of caspase 3 activity was also significantly decreased (Table 1).
Endothelial apoptosis was evaluated with TUNEL peroxidase staining, the number of apoptotic endothelial cells increased from 11±11% in the Co group to 37±9% in the Pn group. A statistically significant decrease was obtained after Z-VAD.fmk administration reducing the number of apoptotic endothelial cells to 11±6% (Fig. 1).
Administration of Z-VAD.fmk decreases extravascular lung water and improves endothelial permeability in P. aeruginosa-induced lung injury.
Lung wet-to-dry-weight ratio (W/D) was significantly increased in the Pn group compared with both, Co and ZPn groups (Table 2). The measurement of the endothelial effect of Z-VAD.fmk showed a decrease of extravascular plasma equivalents in the ZPn group compared with the Pn group (Table 2).
Discussion
Pseudomonas aeruginosa (Pa) has been shown to induce ALI characterized by host inflammation response and diffuse lung edema, leading to a high mortality and morbidity rate in patients with nosocomial bacterial pneumonia [1, 3]. Recent studies indicated that several pathogens, including some bacteria, were able to trigger apoptosis of mammalian host cells [13, 15, 25, 26, 27]. We demonstrated, in vivo, a significant increase in apoptosis activity in the lung during the early phase of P. aeruginosa pneumonia, involving both alveolar epithelial cells (AEC) and endothelial cells. The percentage of apoptotic cells was decreased and extravascular lung water content was reduced after the administration of Z-VAD.fmk, a caspase inhibitor. These results indicate an interesting role for apoptosis modulation during P. aeruginosa-induced lung injury.
Many studies have shown the occurrence of apoptosis in septic shock and acute lung injury in patients as well as experimental models [28, 29, 30, 31]. After intravenous LPS administration, Kawasaki et al. found apoptosis in lung tissues involving alveolar epithelial as well as endothelial cells [19]. In Streptococcus sanguis lung infection, TUNEL-positive cells were observed in the airway epithelium [13]. Other studies involving group A Streptococcus and Staphylococcus aureus showed a pathogen-induced apoptosis of epithelial cells [25, 26]. In our study, we show apoptosis of both alveolar and endothelial cells; the number of TUNEL-positive cells was significantly increased 4 h after P. aeruginosa intratracheal instillation compared with the control group. The identification of epithelial and endothelial cells by histopathological evaluation using hematoxylin–eosin sections is very difficult without an associated electron microscopy ultrastructure analysis. Even if our evaluation was performed with two blinded pathologists, these results on epithelial and endothelial cells apoptosis should be analyzed very carefully. The analysis of apoptosis must not rely on a single parameter; we therefore used other elements and, consistent with these results, both caspase 3 activity and oligonucleosome assay showed an increased apoptosis after P. aeruginosa instillation.
It was recently shown that P. aeruginosa infection induced apoptosis of lung epithelial cells by activation of the endogenous CD95/CD95 ligand system. Indeed, deficiency of this system prevented apoptosis of lung epithelial cells in vitro as well as in vivo [16]. Using a different P. aeruginosa strain, Hauser and Engel showed that P. aeruginosa-induced apoptosis of macrophages and epithelial cells was related to P. aeruginosa type-III secretion system [14]. In contrast, another study found that the airway epithelium was highly resistant to apoptosis after PaO1 exposition [15]. These discrepancies between this last result and our study may be related to the inoculum size which was significantly lower (1.106 CFU/ml) and to the experimental model: the study was not performed in vivo but with epithelial cells culture.
From these data and our results we conclude that P. aeruginosa induces alveolar epithelial and endothelial cells apoptosis in vivo; therefore, in the second part of our work, we studied whether inhibition of apoptosis could be associated with an improvement of lung fluid balance in P. aeruginosa pneumonia. We co-treated the animals with the tripeptide benzyloxycarbonil-Val-Ala-Asp fluoromethylketone (Z-VAD.fmk), a broad-spectrum caspase inhibitor, which has been shown to inhibit the intracellular activation of caspases in vitro and in vivo [32]. There is actually a solid line of evidence that the capacity of maintaining alveolar active fluid transport is highly correlated with a favorable outcome in patients with acute lung injury [12, 33]. It was therefore interesting to evaluate potential functional consequences related to apoptosis inhibition.
In our study, we observed after Pseudomonas instillation an increase of the extravascular lung water associated with an increase in extravascular plasma equivalent. The coadministration of Z-VAD.fmk decreased the number of apoptotic cells (Fig. 2), lung wet-to-dry-weight ratio as well as extravascular plasma equivalent (Table 2). These data show in P. aeruginosa pneumonia a major role of endothelial apoptosis. It has also been demonstrated that P. aeruginosa could induce endothelial cell apoptosis [15], which is consistent with our TUNEL analysis of endothelial cells. The effect we describe on lung water may therefore be related to an anti-apoptotic action of Z-VAD.fmk on endothelial cells. We only used one compound to inhibit apoptosis, but Z-VAD.fmk-related apoptosis inhibition is largely documented in the literature [32] and this molecule has previously been used in lung models to inhibit apoptosis [19] as well as in other models [18]; however, one author reported that this molecule could also induce cathepsin inhibition [34]. Oberholzer et al. also showed that inhibition of caspase activity by Z-VAD.fmk significantly reduced lipolysaccharide or Staphylococcus aureus induced release of interleukin 1 beta [35]. This effect was regulated through the IL-1-converting-enzyme/caspase-1. We observed a decrease of apoptosis after Z-VAD.fmk administration. This effect could be related either to a direct inhibition of apoptosis by Z-VAD.fmk or an indirect decrease through the inflammatory cascade modulation.
If apoptosis inhibition is an attractive hypothesis for clinical trials in infectious diseases, we must underline several limitations of our study. In fact, we use a high inoculum, a non-uniform instillation (mainly peri-hilar), and short end points (4 h), all of which can make a difference in a clinical setting. Nevertheless, the effect of Z-VAD.fmk is interesting and gives several research pathways to improve pneumonia management.
Conclusion
In conclusion, apoptosis occurs in the early phase of P. aeruginosa pneumonia. Z-VAD.fmk co administration with the pathogen can significantly, in vivo, decrease this apoptotic process mainly through an endothelial protective mechanism. Apoptosis is an important feature in P. aeruginosa pneumonia, and further evaluation of blocking factor, such as Z-VAD.fmk, could be an interesting challenge in therapeutic research.
References
Rello J, Ollendorf DA, Oster G, Vera-Llonch M, Bellm L, Redman R, Kollef MH (2002) Epidemiology and outcomes of ventilator-associated pneumonia in a large US database. Chest 122:2115–2121
Chastre J, Fagon JY (2002) Ventilator-associated pneumonia. Am J Respir Crit Care Med 165:867–903
Fagon JY, Chastre J, Domart Y, Trouillet JL, Gibert C (1996) Mortality due to ventilated-associated pneumonia or colonization with Pseudomonas or Acinetobacter species: assessment by quantitative culture of samples obtained by a protected specimen brush. Clin Infect Dis 23:538–542
Akca O, Koltka K, Uzel S, Cakar N, Pembeci K, Sayan MA, Tutuncu AS, Karakas SE, Calangu S, Ozkan T, Esen F, Telci L, Sessler DI, Akpir K (2000) Risk factors for early-onset, ventilator-associated pneumonia in critical care patients: selected multiresistant versus nonresistant bacteria. Anesthesiology 93:638–645
Goodman B, Kim K, Crandall E (1987) Evidence for active sodium transport across alveolar epithelium of isolated rat lung. J Appl Physiol 62:2460–2466
Goodman B, Fleischer R, Crandall E (1983) Evidence for active Na+ transport by cultured monolayers of pulmonary alveolar epithelial cells. Am J Physiol 245:C78–C83
Sakuma T, Folkesson HG, Suzuki S, Okaniwa G, Fujimura S, Matthay MA (1997) Beta-adrenergic agonist stimulated alveolar fluid clearance in ex vivo human and rat lungs. Am J Respir Crit Care Med 155:506–512
Sakuma T, Okaniwa G, Nakada T, Nishimura T, Fujimura S, Matthay MA (1994) Alveolar fluid clearance in the resected human lung. Am J Respir Crit Care Med 150:305–310
Rezaiguia S, Garat C, Delclaux C, Fleury J, Legrand P, Matthay MA, Jayr C (1997) Acute bacterial pneumonia in rats increases alveolar epithelial fluid clearance by a tumor necrosis factor-alpha-dependent mechanism. J Clin Invest 99:325–335
Viget N, Guery B, Ader F, Nevière R, Alfandari S, Creusy C, Roussel-Delvallez M, Foucher C, Mason CM, Beaucaire G, Pittet JF (2000) Keratinocyte growth factor protects against Pseudomonas aeruginosa-induced lung injury. Am J Physiol Lung Cell Mol Physiol 279:L1199–L1209
Ware LB, Matthay MA (2001) Alveolar fluid clearance is impaired in the majority of patients with acute lung injury and the acute respiratory distress syndrome. Am J Respir Crit Care Med 163:1376–1383
Matthay MA, Wiener-Kronish JP (1990) Intact epithelial barrier function is critical for the resolution of alveolar edema in humans. Am Rev Respir Dis 142:1250–1257
Mantell L, Kazzaz J, Xu J, Palaia T, Piedboeuf B, Hall S, Rhodes G, Niu G, Fein A, Horowitz S (1997) Unscheduled apoptosis during acute inflamatory lung injury. Cell Death Differentiation 4:600–607
Hauser AR, Engel JN (1999) Pseudomonas aeruginosa induces type-III-secretion-mediated apoptosis of macrophages and epithelial cells. Infect Immun 67:5530–5537
Rajan S, Cacalano G, Bryan R, Ratner AJ, Sontich CU, van Heerckeren A, Davis P, Prince A (2000) Pseudomonas aeruginosa induction of apoptosis in respiratory epithelial cells: analysis of the effects of cystic fibrosis transmembrane conductance regulator dysfunction and bacterial virulence factors. Am J Respir Cell Mol Biol 23:304–312
Grassme H, Kirschnek S, Riethmueller J, Riehle A, Kurthy G von, Lang F, Weller M, Gulbins E (2000) CD95/CD95 ligand interactions on epithelial cells in host defense to Pseudomonas aeruginosa. Science 290:527–530
Haimovitz-Friedman A, Cordon-Cardo C, Bayoumy S, Garzotto M, McLoughlin M, Gallily R, Edwards CK III, Schuchman EH, Fuks Z, Kolesnick R (1997) Lipopolysaccharide induces disseminated endothelial apoptosis requiring ceramide generation. J Exp Med 186:1831–1841
Neviere R, Fauvel H, Chopin C, Formstecher P, Marchetti P (2001) Caspase inhibition prevents cardiac dysfunction and heart apoptosis in a rat model of sepsis. Am J Respir Crit Care Med 163:218–225
Kawasaki M, Kuwano K, Hagimoto N, Matsubara H, Kunitake R, Tanaka T, Maeyama T, Hara N (2000) Protection from lethal apoptosis in lipopolysaccharide-induced acute lung injury in mice by a caspase inhibitor. Am J Pathol 157:597–603
Pennington JE, Ehrie MG (1978) Pathogenesis of Pseudomonas aeruginosa pneumonia during immunosuppression. J Infect Dis 137:764–774
McElroy MC, Wiener-Kronish JP, Miyazaki H, Sawa T, Modelska K, Dobbs LG, Pittet JF (1997) Nitric oxide attenuates lung endothelial injury caused by sublethal hyperoxia in rats. Am J Physiol 272:L631–L638
Modelska K, Matthay MA, McElroy MC, Pittet JF (1997) Upregulation of alveolar liquid clearance after fluid resuscitation for hemorrhagic shock in rats. Am J Physiol 273:L305–L314
Pittet,J, Hashimoto,S, Pian,M, McElroy,M.C, Nitenberg,G, and Wiener-Kronish,J.P. (1996): Exotoxin A stimulates fluid reabsorption from distal airspaces of lung in anesthetized rats. Am J Physiol, 270:L232-L241
Hunter WM, Greenwood FC (1962) Preparation of iodine-131 labeled human hormone of high specific activity. Nature 194:495–496
Kahl BC, Goulian M, van Wamel W, Herrmann M, Simon SM, Kaplan G, Peters G, Cheung AL (2000) Staphylococcus aureus RN6390 replicates and induces apoptosis in a pulmonary epithelial cell line. Infect Immunol 68:5385–5392
Tsai PJ, Lin YS, Kuo CF, Lei HY, Wu JJ (1999) Group A Streptococcus induces apoptosis in human epithelial cells. Infect Immunol 67:4334–4339
Menzies BE, Kourteva I (1998) Internalization of Staphylococcus aureus by endothelial cells induces apoptosis. Infect Immunol 66:5994–5998
Hotchkiss RS, Swanson PE, Freeman BD, Tinsley KW, Cobb JP, Matuschak GM, Buchman TG, Karl IE (1999) Apoptotic cell death in patients with sepsis, shock, and multiple organ dysfunction. Crit Care Med 27:1230–1251
Hashimoto S, Kobayashi A, Kooguchi K, Kitamura Y, Onodera H, Nakajima H (2000) Upregulation of two death pathways of perforin/granzyme and FasL/Fas in septic acute respiratory distress syndrome. Am J Respir Crit Care Med 161:237–243
Lin E, Katz JA, Calvano SE, Coyle SM, Randhawa S, Shahin I, Kumar A, Lowry SF (1998) The influence of human endotoxemia on CD95-induced apoptosis. Arch Surg 133:1322–1327
Haendeler J, Messmer UK, Brune B, Neugebauer E, Dimmeler S (1996) Endotoxic shock leads to apoptosis in vivo and reduces Bcl-2. Shock 6:405–409
van Noorden CJ (2001) The history of Z-VAD-FMK, a tool for understanding the significance of caspase inhibition. Acta Histochem 103:241–251
Verghese GM, Ware LB, Matthay BA, Matthay MA (1999) Alveolar epithelial fluid transport and the resolution of clinically severe hydrostatic pulmonary edema. J Appl Physiol 87:1301–1312
Schotte P, Declercq W, Van Huffel S, Vandenabeele P, Beyaert R (1999) Non-specific effects of methyl ketone peptide inhibitors of caspases. FEBS Lett 442:117–121
Oberholzer A, Harter L, Feilner A, Steckholzer U, Trentz O, Ertel W (2000) Differential effect of caspase inhibition on proinflammatory cytokine release in septic patients. Shock 14:253–257
Acknowledgements
The authors thank M. Matthay and R. Nevière for all the help and support they provided in the elaboration of this work. M. Roussel-Delvallez and J.M. Marissael were very helpful for the bacterial preparation. We are also very grateful to X. Marchandise, M. Tassin, P. Briche, N. Zenani, and P. Fialdes for their daily encouragements. C. Chopin and the EA 2689 team allowed managing and improving our studies. Most of this work was performed with the very helpful support of C. Vouillot, D. Vallée, and J.P. Dheson of the SmithKline-Beecham Institute. This work as supported by grants EA 2689, CHRU de Lille, SmithKline-Beecham Institute, and NIH 614 62 188
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Berre, R.L., Faure, K., Fauvel, H. et al. Apoptosis inhibition in P. aeruginosa-induced lung injury influences lung fluid balance. Intensive Care Med 30, 1204–1211 (2004). https://doi.org/10.1007/s00134-004-2165-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-004-2165-0