Abstract
Objective
More than one-half the deaths of patients admitted to intensive care units (ICUs) occur after a decision to forgo life-sustaining therapy (DFLST). Although DFLSTs typically occur in patients with severe comorbidities and intractable acute medical disorders, other factors may influence the likelihood of DFLSTs. The objectives of this study were to describe the factors and mortality associated with DFLSTs and to evaluate the potential independent impact of DFLSTs on hospital mortality.
Design and setting
Prospective multicenter 2-year study in six ICUs in France.
Patients
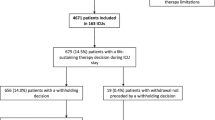
The 1,698 patients admitted to the participating ICUs during the study period, including 295 (17.4%) with DFLSTs.
Measurements and results
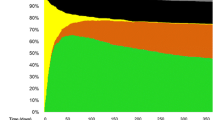
The impact of DFLSTs on hospital mortality was evaluated using a model that incorporates changes in daily logistic organ dysfunction scores during the first ICU week. Univariate predictors of death included demographic factors (age, gender), comorbidities, reasons for ICU admission, severity scores at ICU admission, and DFLSTs. In a stepwise Cox model five variables independently predicted mortality: good chronic health status (hazard ratio, 0.479), SAPS II score higher than 39 (2.05), chronic liver disease (1.463), daily logistic organ dysfunction score (1.357 per point), and DFLSTs (1.887).
Conclusions
DFLSTs remain independently associated with death after adjusting on comorbidities and severity at ICU admission and within the first ICU week. This highlights the need for further clarifying the many determinants of DFLSTs and for routinely collecting DFLSTs in studies with survival as the outcome variable of interest.
Similar content being viewed by others
References
Ferrand E, Robert R, Ingrand P, Lemaire F (2001) Withholding and withdrawal of life support in intensive-care units in France: a prospective survey. French LATAREA Group. Lancet 357:9–14
Asch DA, DeKay ML (1997) Euthanasia among US critical care nurses. Practices, attitudes, and social and professional correlates. Med Care 35:890–900
Pochard F, Azoulay E, Chevret S, Vinsonneau C, Grassin M, Lemaire F, Herve C, Schlemmer B, Zittoun R, Dhainaut JF (2001) French intensivists do not apply American recommendations regarding decisions to forgo life-sustaining therapy. Crit Care Med 29:1887–1892
Prendergast TJ, Claessens MT, Luce JM (1998) A national survey of end-of-life care for critically ill patients. Am J Respir Crit Care Med 158:1163–1167
Prendergast TJ, Luce JM (1997) Increasing incidence of withholding and withdrawal of life support from the critically ill. Am J Respir Crit Care Med 155:15–20
McLean RF, Tarshis J, Mazer CD Szalai JP (2000) Death in two Canadian intensive care units: institutional difference and changes over time. Crit Care Med 28:100–103
Jayes RL, Zimmerman JE, Wagner DP, Draper EA, Knaus WA (1993) Do-not-resuscitate orders in intensive care units. Current practices and recent changes. JAMA 270:2213–2217
American Thoracic Society Board of Directors (1991) Withholding and withdrawing life-sustaining therapy. Am Rev Respir Dis 144:726–731
Truog RD, Cist AF, Brackett SE, Burns JP, Curley MA, Danis M, DeVita MA, Rosenbaum SH, Rothenberg DM, Sprung CL, Webb SA, Wlody GS, Hurford WE (2001) Recommendations for end-of-life care in the intensive care unit: the Ethics Committee of the Society of Critical Care Medicine. Crit Care Med 29:2332–2348
Sulmasy DP (1999) Do patients die because they have DNR orders, or do they have DNR orders because they are going to die? Med Care 37:719–721
Cook DJ, Guyatt GH, Jaeschke R, Reeve J, Spanier A, King D, Molloy DW, Willan A, Streiner DL (1995) Determinants in Canadian health care workers of the decision to withdraw life support from the critically ill. Canadian Critical Care Trials Group. JAMA 273:703–708
Cook DJ (1997) Health professional decision-making in the ICU: a review of the evidence. New Horiz 5:15–519
Caralis PV, Hammond JS (1992) Attitudes of medical students, housestaff, and faculty physicians toward euthanasia and termination of life-sustaining treatment. Crit Care Med 20:683–690
Fried TR, Bradley EH, Towle VR, Allore H (2002) Understanding the treatment preferences of seriously ill patients. N Engl J Med 346:1061–1066
Wenger NS, Pearson ML, Desmond KA, Brook RH, Kahn KL (1995) Outcomes of patients with do-not-resuscitate orders. Toward an understanding of what do-not-resuscitate orders mean and how they affect patients. Arch Intern Med 155:2063–2068
Rivera S, Kim D, Garone S, Morgenstern L, Mohsenifar Z (2001) Motivating factors in futile clinical interventions. Chest 119:1944–1947
Asai A, Fukuhara S, Lo B (1995) Attitudes of Japanese and Japanese-American physicians towards life-sustaining treatment. Lancet 346:356–359
Kollef MH (1996) Private attending physician status and the withdrawal of life-sustaining interventions in a medical intensive care unit population. Crit Care Med 24:968–975
Kelly WF, Eliasson AH, Stocker DJ, Hnatiuk OW (2002) Do specialists differ on do-not-resuscitate decisions? Chest 121:957–963
Mebane EW, Oman RF, Kroonen LT, Goldstein MK (1999) The influence of physician race, age, and gender on physician attitudes toward advance care directives and preferences for end-of-life decision-making. J Am Geriatr Soc 47:579–591
Shepardson LB, Gordon HS, Ibrahim SA, Harper DL, Rosenthal GE (1999) Racial variation in the use of do-not-resuscitate orders. J Gen Intern Med 14:15–20
Le Gall JR, Klar J, Lemeshow S, Saulnier F, Alberti C, Artigas A, Teres D (1996) The Logistic Organ Dysfunction system. A new way to assess organ dysfunction in the intensive care unit. ICU Scoring Group. JAMA 276:802–810
Le Gall JR, Lemeshow S, Saulnier F (1993) A new Simplified Acute Physiology Score (SAPS II) based on a European/North American multicenter study. JAMA 270:2957–2963
Knaus WA, Draper EA, Wagner DP, Zimmerman JE (1985) APACHE II: a severity of disease classification system. Crit Care Med 13:818–829
Timsit JF, Fosse JP, Troche G, De Lassence A, Alberti C, Garrouste-Orgeas M, Azoulay E, Chevret S, Moine P, Cohen Y (2001) Accuracy of a composite score using daily SAPS II and LOD scores for predicting hospital mortality in ICU patients hospitalized for more than 72\h. Intensive Care Med 27:1012–1021
Prendergast TJ (2000) Withholding or withdrawal of life-sustaining therapy. Hosp Pract (Off Ed) 35:91–2:95–100:102
Keenan SP, Busche KD, Chen LM, Esmail R, Inman KJ, Sibbald WJ (1998) Withdrawal and withholding of life support in the intensive care unit: a comparison of teaching and community hospitals. The Southwestern Ontario Critical Care Research Network. Crit Care Med 26:245–251
Hall RI, Rocker GM (2000) End-of-life care in the ICU: treatments provided when life support was or was not withdrawn. Chest 118:1424–1430
Wenger NS, Pearson ML, Desmond KA, Harrison ER, Rubenstein LV, Rogers WH, Kahn KL (1995) Epidemiology of do-not-resuscitate orders. Disparity by age, diagnosis, gender, race, and functional impairment. Arch Intern Med 155:2056–2062
Shepardson LB, Youngner SJ, Speroff T, Rosenthal GE (1999) Increased risk of death in patients with do-not-resuscitate orders. Med Care 37:727–737
Markgraf R, Deutschinoff G, Pientka L, Scholten T, Lorenz C (2001) Performance of the score systems Acute Physiology and Chronic Health Evaluation II and III at an interdisciplinary intensive care unit, after customization. Crit Care 5:31–36
Pettila V, Pettila M, Sarna S, Voutilainen P, Takkunen O (2002) Comparison of multiple organ dysfunction scores in the prediction of hospital mortality in the critically ill. Crit Care Med 30:1705–1711
Ferreira FL, Bota DP, Bross A, Melot C, Vincent JL (2001) Serial evaluation of the SOFA score to predict outcome in critically ill patients. JAMA 286:1754–1758
Atkinson S, Bihari D, Smithies M, Daly K, Mason R, McColl I (1994) Identification of futility in intensive care. Lancet 344:1203–1206
Second European Consensus Conference in Intensive Care Medicine (1994) Predicting outcome in ICU patients. Intensive Care Med 20:390–397
Cook DJ, Giacomini M, Johnson N, Willms D (1999) Life support in the intensive care unit: a qualitative investigation of technological purposes. Canadian Critical Care Trials Group. Can Med Assoc J 161:1109–1113
Stevens L, Cook D, Guyatt G, Griffith L, Walter S, McMullin J (2002) Education, ethics, and end-of-life decisions in the intensive care unit. Crit Care Med 30:290–296
Astrow AB, Puchalski CM, Sulmasy DP (2001) Religion, spirituality, and health care: social, ethical, and practical considerations. Am J Med 110:283–287
Lo B, Ruston D, Kates LW, Arnold RM, Cohen CB, Faber-Langendoen K, Pantilat SZ, Puchalski CM, Quill TR, Rabow MW, Schreiber S, Sulmasy DP, Tulsky JA (2002) Discussing religious and spiritual issues at the end of life: a practical guide for physicians. JAMA 287:749–754
Keenan SP, Mawdsley C, Plotkin D, Webster GK, Priestap F (2000) Withdrawal of life support: how the family feels, and why. J Palliat Care 16:S40–S44
Pochard F, Azoulay E, Grassin M (2001) Assessing requests for euthanasia from terminally ill patients. JAMA 285:734–735
Wachter RM, Luce JM, Hearst N, Lo B (1989) Decisions about resuscitation: inequities among patients with different diseases but similar prognoses. Ann Intern Med 111:525–532
Hakim RB, Teno JM, Harrell, FE Jr, Knaus WA, Wenger N, Phillips RS, Layde P, Califf R, Connors AF Jr, Lynn J (1996) Factors associated with do-not-resuscitate orders: patients’ preferences, prognoses, and physicians’ judgments. SUPPORT Investigators. Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatment. Ann Intern Med 125:284–293
Acknowledgements
The authors are indebted to A. Wolfe, MD, for her help in preparing this manuscript and to S. Chevret, MD, PhD, for her critical reading of the manuscript and help in selecting the statistical models. The Outcomerea Study Group includes: Saint-Louis Teaching Hospital (Medical ICU Department and Biostatistics department), Cochin Teaching Hospital (Psychiatry Department), Saint-Joseph Teaching Hospital (Medical-Surgical ICU), Bichat Teaching Hospital (Medical-Surgical ICU), Saint-Denis Teaching Hospital (Medical-Surgical ICU), Louis Mourier Teaching Hospital (Medical ICU), and Avicenne Teaching Hospital (Medical-Surgical ICU).
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
Outcomerea receives an unrestricted grant from the Centre National pour la Recherche Scientifique.
Rights and permissions
About this article
Cite this article
Azoulay, É., Pochard, F., Garrouste-Orgeas, M. et al. Decisions to forgo life-sustaining therapy in ICU patients independently predict hospital death. Intensive Care Med 29, 1895–1901 (2003). https://doi.org/10.1007/s00134-003-1989-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-003-1989-3