Abstract
Objective
To evaluate the incidence and the circumstances of a moderate increase in serum creatinine early after elective abdominal aortic surgery.
Design
Prospective clinical observational study.
Setting
Surgical intensive care unit in a university hospital.
Patients
Two hundred and fifteen consecutive adult patients operated on for infra-renal abdominal aortic surgery during 1 year.
Interventions
A moderate increase in plasma creatinine of 20% from preoperative value (renal dysfunction, RD) was systematically recorded during the first 3 days following surgery. Organ dysfunctions (cardiac, pulmonary, haematological, and neurological) were assessed.
Measurements and results
Forty-three patients (20%) experienced a postoperative RD; six of these required dialysis. RD was associated with other organ dysfunctions in 60.5% patients. Mortality rate was significantly higher for patients who had a RD, than patients without RD (9.3% vs 1.2%, P<0.02). Mean ICU stay of patients with RD was significantly longer (7.9±5.6 days vs 5.0±1.8 days, P<0.01). However, patients with RD but without other organ dysfunctions had a mortality rate of 0% and did not have a significantly longer stay in ICU than patients without any organ dysfunctions (5.2±2.1 days vs 4.6±1.2 days, P=0.09).
Conclusion
Our results suggest that a postoperative 20%-increase in plasma creatinine after abdominal aortic surgery is not rare and occurs frequently with other organ dysfunction.
Similar content being viewed by others
Introduction
Depending on the definition used for renal dysfunction, from 2.5% to 45% of patients may develop a renal failure following abdominal aortic (AA) surgery [1, 2, 3]. Acute renal failure requiring dialysis is considered as a severe postoperative complication with a high mortality rate (30–75%) [1, 2, 3, 4, 5, 6] and is mainly related to progressive multiple organ dysfunction [7, 8]. On the other hand, little is known about the incidence and the prognosis of a moderate renal dysfunction after surgery. The present study was undertaken to evaluate the incidence and the circumstances of occurrence of a moderate increase in plasma creatinine early after AA surgery.
Methods
Patient selection and management
Two hundred and fifteen consecutive adult patients (24–89 years old, 198 males) operated on for elective abdominal aortic surgery, i.e., abdominal aortic aneurysm (AAA), or aorto-iliac occlusive disease (AOD), have been prospectively included in a data base during 1 year.
Perioperative management was standardized for all patients including general anaesthesia (benzodiazepine, fentanyl, and isoflurane) and controlled ventilation. The usual cardiac treatment was maintained until the day of surgery, except diuretics, angiotensin-converting enzyme (ACE) inhibitor, and anti-arrhythmic drugs that were stopped the day before surgery. Patients did not receive contrast media within the 2 weeks preceding surgery. In all patients mean arterial pressure (MAP) was continuously monitored through a radial artery catheter. A crystalloid solution (sodium chloride, Ringer's) adjusted for blood pressure maintenance was infused at a rate of 15–20 ml kg h before aortic clamping, reduced to 10 ml kg h during aortic clamping. Normothermia was ensured with fluid rewarming and a warming blanket. A cell-saver was used during the time of surgery. Hypertension and hypotension as defined as an increase or a decrease in MAP of 20% or more from pre-induction MAP were treated either with increasing anaesthesia (fentanyl or isoflurane), or rapid intravenous administration of solution (lactated Ringer's or colloid) or a vasopressor (MAP ≤60 mmHg), respectively. In the intensive care unit (ICU), repeated boluses of morphine were used to keep the patient pain-free. Weaning from the ventilator was started during emergence of anaesthesia and when stable haemodynamics and normothermia had been maintained for at least 1 h.
Each patient was carefully and thoroughly examined each day so that comorbid events were assessed during the first 3 days after surgery as organ dysfunction: renal dysfunction (RD) was defined as an increase in plasma creatinine of more than 20% from preoperative value and renal failure by the need for dialysis in case of oligo-anuria, hyperkalaemia, or metabolic acidosis; cardiac dysfunction was defined as the need for inotropic support (dobutamine, adrenaline); pulmonary dysfunction was defined as PaO2/FiO2 <200 mmHg; haematological dysfunction was defined as a thrombocyte count <80,000/ml; and neurologic dysfunction was defined as presence of stroke, confusion or agitation.
Mortality was defined as the incidence of death during the stay in the postoperative ICU. Morbidity was assessed with the length of stay in the postoperative ICU.
Data analysis
Data were expressed as mean±SD. Patients with RD were compared with other patients using a Student's t-test. A Fisher exact test was used to compare percentages between patients with or without RD. To determine the relative importance of the postoperative comorbid events on the mortality rate, multivariate analysis using logistic regression was performed. A stepwise selection of the variables was used. Two models were used: without interaction between postoperative comorbid events and with interaction between postoperative comorbid events using a backward elimination procedure. The categories with the less favorable outcome were taken as reference level, all the other categories were included in the model. Odds-ratio (OR) and their confidence intervals (CI 95%) were calculated. To assess the predictive ability of the model, concordance rate between predicted and observed responses was calculated. The goodness-of-fit of the logistic regression model was assessed using the likelihood ratio test and Hosmer and Lemeshow test. The statistical software SAS version 6.11/UNIX was used for statistical analysis. A P value of <0.05 was considered significant.
Results
Patient characteristics and surgery
Patients were 24–89 years old, and most of them were male (92.1%). One hundred and seventy-one cases were scheduled for AAA, and AOD surgery involved 44 patients (Table 1). The surgery was performed with a mean aortic cross clamping time of 67.9±28.8 min. Vasopressor support, inotropic support, and homologous blood transfusion were administered in 6.0%, 1.4%, and 15.3% of patients, respectively.
Incidence of renal dysfunction and comorbid events
RD occurred in 43 patients (20%); six of these (13.9%) or 2.8% of all study patients required dialysis. Pulmonary, hematological, neurological, or cardiac dysfunction occurred in 38 patients (17.7%), 31 patients (14.4%), 31 patients (14.4%, two out of 31 experienced a stroke), and 19 patients (8.8%), respectively. Three or more associated organ dysfunctions (OD) occurred in 19 patients (8.8%). Cardiac dysfunction was significantly related with either pulmonary, neurologic or renal dysfunctions (P<0.05).
RD occurred without any other OD (isolated RD) in 17 patients (39.5% of all RD patients), and one patient (5.9%) of these 17 needed dialysis. RD was associated with other OD as follows: neurological dysfunction in 30.2% patients (one stroke), cardiac dysfunction in 27.9%, pulmonary dysfunction in 20.9%, and hematological dysfunction in 18.6%. Three or more associated OD occurred in 14 patients (32.6%). Preoperative and peroperative characteristics of patients who experienced a RD or not are presented in Table 2.
Mortality and morbidity
Death occurred in six patients (2.8%) and mean stay in postoperative ICU was 5.6±3.2 days (from 2 days to 26 days). Mortality rate increased with the number of OD: mortality rate was 1% for two OD, and 21.1% for more than three OD (P<0.01). Length of stay in ICU increased with the number of OD (from 0 days to 4:4.7±1.2 days to 9.7±5.8 days, P<0.01).
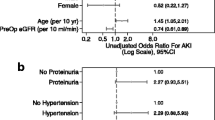
Four patients (9.3%) out of the 43 who developed a RD died; the mortality rate was significantly higher than in patients without RD (1.2%, P<0.02) and increased with the number of combined organ dysfunctions: 0% for RD associated with one other OD, and 28.6% for RD associated with more than two other ODs (P<0.02). Three out of the six patients (50%) who needed dialysis died (P<0.01 versus patients without dialysis). Patients who experienced an isolated RD had a mortality rate of 0%, which was not significantly different from patients without any OD (n=115) (0.8%, P>0.99). The logistic regression without interaction between postoperative comorbid events confirmed that the most important prognostic factor of mortality was cardiac dysfunction (OR=69.6; 95% CI: 7.6 – 637.7). Concordance rate between predicted and observed responses was good (77.8%). Hosmer and Lemeshow Goodness-of-fit test was not significant. The logistic regression with interaction between postoperative comorbid events did not reveal any significant relation between comorbid complications that may have influenced the mortality rate.
When compared to patients without RD the mean ICU stay of patients with RD was significantly longer (7.9±5.6days vs 5.0±1.8 days, P<0.01). Patients with isolated RD did not have a significantly longer stay in ICU than patients without any OD (5.2±2.1 days vs 4.6±1.2 days, P=0.09).
Discussion
The study demonstrates that the incidence of a moderate increase in creatinine (RD) shortly after elective infrarenal abdominal aortic surgery is 20%. In the context of elective surgery, the patients who experienced RD had preoperative altered renal function and prolonged aortic cross clamping time and more transfusion requirement. RD is mostly associated with other organ dysfunctions.
Creatinine is not a real-time descriptor of glomerular filtration rate (GFR). However, it is considered a practical and reasonable approach to use it for defining acute renal failure [9]. The increase in serum creatinine from the preoperative value has been already used to detect postoperative RD [10, 11]. However, the cut-off values of the increase in serum creatinine from baseline were higher, 30–40% [10, 11]. An increase in plasma creatinine of more than 20% from preoperative value has a good specificity (0.99) to detect a decrease in creatinine clearance of at least 20%, but a low sensitivity (0.46) [12]. A low sensitivity means that significant reduction in creatinine clearance may not be detected by a moderate increase in serum creatinine. Nevertheless, using creatinine clearance which is thought to be a reliable marker of GFR, a 20% decrease from baseline gave a 24% incidence of postoperative RD in patients operated on elective abdominal surgery [13]. Therefore, although reducing the threshold of renal impairment detection automatically increases the incidence of RD [14], a 20% increase in postoperative serum creatinine may be appropriate to discriminate patients with or without GFR impairment. The incidence of acute renal failure requiring dialysis (2.8%) and the early postoperative mortality rate (2.8%) are close to the range reported in larger studies (2–5%, and 5–7%) [2, 5].
Patients who suffered from postoperative RD underwent other organ dysfunction in 60.5% cases with multiple organ failure (three or more organ dysfunctions) in almost 33%. MOF has been already described after abdominal aortic surgery and has been mainly observed in patients with preoperative altered renal function who underwent prolonged or emergent surgery, with perioperative episodes of cardiovascular impairment (hypotension and low cardiac output) [8, 15]. In the present study, besides neurological dysfunction which consisted of transient postoperative delirium more than stroke, cardiac dysfunction was the most frequent associated dysfunction with RD. Cardiac dysfunction, which occurred in 27.9% patients with RD, significantly influenced the outcome. A great proportion of patients (83.3%) who required an inotropic support in the postoperative period died. Death incidence following surgical repair of abdominal aortic surgery is closely related to the occurrence of MOF (21.1% patients with more than three OD died) [3, 6, 7, 8, 16]. Nevertheless cardiac dysfunction may have a prominent role in initiating MOF and death; it is the association of OD with cardiac dysfunction that worsens the early postoperative death rate. Conversely, when postoperative RD occurs alone, it is not associated with postoperative death or increased length of stay in postoperative ICU.
References
McCombs PR, Roberts B (1979) Acute renal failure following resection of abdominal aorta. Surg Gynecol Obstet 148:175–178
Diehl JT, Cali RF, Hertzer NR, Beven EG (1983) Complications of abdominal aortic reconstruction. Ann Surg 197:49–56
Olsen PS, Schroeder T, Perko M, Roder OC, Agerskov K, Sorensen S, Lorentzen JE (1990) Renal failure after operation for abdominal aortic aneurysm. Ann Vasc Surg 4:580–583
Novis BK, Roizen MF, Aronson S, Thisted RA (1994) Association of preoperative risk factors with postoperative acute renal failure. Anesth Analg 78:143–149
Ostri P, Mouristen L, Jorgendsen B, Frimodt-Moller C (1986) Renal function following aneurysmectomy of the abdominal aorta. J Cardiovasc Surg 27:714–718
Braams R, Vossen V, Lisman BA, Eikelboom BC (1999) Outcome in patients requiring renal replacement therapy after surgery for ruptured and non-ruptured aneurysm of the abdominal aorta. Eur J Vasc Endovasc Surg 18:323–327
Maziak DE, Lindsay TF, Marshall JC, Walker PM (1998) The impact of multiple organ dysfunction on mortality following ruptured abdominal aneurysm repair. Ann Vasc Surg 12:93–100
Barratt J, Parajasingam R, Sayers RD, Feehally J (2000) Outcome of acute renal failure following repair of ruptured abdominal aortic aneurysm. Eur J Vasc Endovasc Surg 20:163–168
Bellomo R, Kellum J, Ronco C (2001) Acute renal failure: time for consensus. Int Care Med 27:1685–1688
Godet G, Fléron MH, Vicaut E, Zubicki A, Bertrand M, Riou B, Kieffer E, Coriat P (1997) Risk factors for acute postoperative renal failure in thoracic or thoracoabdominal aortic surgery: a prospective study. Anesth Analg 85:1227–1232
Mangano CM, Diamondstone LS, Ramsay JG, Aggarval A, Herskowitz A, Mangano D (1998) Renal dysfunction after myocardial revascularization: risk factors, adverse outcomes, and hospital resource utilization. Ann Intern Med 128:194–203
Zubicki A, Cittanova ML, Zaier K, Montalvan C, Nefaa N, Coriat P (1998) Serum creatinine cannot predict renal impairment in the perioperative period. Br J Anaesth 80[suppl 1]:7
Cittanova ML, Zubicki A, Savu C, Montalvan C, Nefaa N, Zaier K, Riou B, Coriat P (2001) The chronic inhibition of angiotensin-converting enzyme impairs postoperative renal function. Anesth Analg 93:1111–1115
McCullough PA, Wolyn R, Rocher LL, Rocher LL, Levin RN, O'Neill WW (1997) Acute renal failure after coronary intervention: incidence, risk factors, and relationship to mortality. Am J Med 103:368–377
Powell RJ, Roddy SP, Meier GH, Gusberg RJ, Conte MS, Sumpio BE (1997) Effect of renal insufficiency on outcome following infrarenal aortic surgery. Am J Surg 174:126–133
Berisa F, Beaman M, Alu D, McGonigle RJ, Michael J, Downing R, Fielding JW, Dunn J (1990) Prognostic factor in acute renal failure following aortic aneurysm surgery. Q J Med 76:689–698
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ryckwaert, F., Alric, P., Picot, MC. et al. Incidence and circumstances of serum creatinine increase after abdominal aortic surgery. Intensive Care Med 29, 1821–1824 (2003). https://doi.org/10.1007/s00134-003-1958-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-003-1958-x