Abstract
Objective
To report the use of tetracyclines for the treatment of multidrug-resistant Acinetobacter baumannii ventilator-associated pneumonia (VAP).
Design
Observational case series.
Setting
The Presley Regional Trauma Center located within the Regional Medical Center, Memphis, Tennessee, USA.
Patients and participants
Seven critically ill trauma patients with VAP caused by A. baumannii isolates that were resistant to all antibiotics tested except for doxycycline or minocycline.
Interventions
Patients were treated with IV doxycycline or minocycline for an average of 13.5 (range 9–20) days.
Measurements and results
Doxycycline or minocycline was successful in six of seven patients.
Conclusions
Doxycycline or minocycline may be effective for treating multidrug-resistant A. baumannii VAP.
Similar content being viewed by others
Introduction
Critically ill patients who develop ventilator-associated pneumonia (VAP) experience increased morbidity and mortality [1]. In particular, Acinetobacter baumannii is a common cause of late onset VAP in some centers where it is associated with a high mortality rate [1]. Imipenem or meropenem are generally considered the drugs of choice for A. baumannii; however, resistance to these agents is increasing [2]. Recent data suggest that the sulbactam component of ampicillin-sulbactam is clinically effective against some carbapenem-resistant isolates [3]; however, there are few data to guide the selection of agents for treating isolates that are resistant to both carbapenems and sulbactam. For such isolates, tetracyclines may be a viable treatment option based on good in vitro activity in some centers and success in an animal model of A. baumannii pneumonia [2, 4]. Recently, we used minocycline or doxycycline to treat seven patients with VAP caused by A. baumannii isolates that were resistant to all other antibiotics. This is the first report describing the use of tetracyclines for the treatment of multidrug-resistant A. baumannii VAP.
Materials and methods
Patients were identified by a retrospective review of an existing database of late-onset VAP. All patients were cared for in the intensive care unit of the Presley Regional Trauma Center at the Regional Medical Center, Memphis, Tennessee between January and December 1998. The diagnosis of VAP required bacterial growth of >105 colony forming units (CFU)/ml from a diagnostic bronchoalveolar lavage (BAL) in addition to fever, leukocytosis or leukopenia, macroscopically purulent sputum, and new or changing infiltrate on chest radiograph [5]. Organisms were identified by the hospital microbiology laboratory using the Vitek system (bioMerieux, Hazelwood, MO, USA). Antimicrobial susceptibility of A. baumannii isolates was performed by the hospital microbiology laboratory using a disk diffusion method (Becton Dickinson Microbiology Systems, Cockeysville, MD, USA).
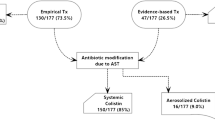
Treatment was considered successful if A. baumannii was absent from a follow-up BAL culture and the patient improved clinically. For patients without a follow-up BAL, treatment was considered successful if the patient improved clinically and survived until discharge from the hospital. Treatment was considered a failure if the patient died from complications of A. baumannii VAP or had persistent A. baumannii VAP on a follow-up BAL without clinical improvement. Based on previous data from our unit, cefepime and vancomycin were administered as empiric therapy to all patients pending the final BAL culture and sensitivity report [5]. A follow-up BAL was performed only when clinically indicated to rule out persistent or new VAP.
Results
Clinical characteristics, microbiological data, and outcomes of seven patients with multidrug-resistant A. baumannii VAP are summarized in Tables 1 and 2. All patients required mechanical ventilation for at least 7 days prior to diagnosis of VAP. All patients were male. One patient (patient 1) with growth of A. baumannii 104–105 CFU/ml from BAL received definitive treatment for VAP because of concomitant A. baumannii bacteremia and the severity of clinical signs and symptoms.
All Acinetobacter isolates were identified as A. baumannii. Five isolates were found to be fully resistant to all agents except minocycline and doxycycline. The two remaining isolates were similar except for intermediate resistance to imipenem in one (patient 1), and intermediate resistance to ampicillin-sulbactam in the other (patient 5). Because of these resistance patterns, all patients were treated definitively with either doxycycline 100 mg IV q12 h (American Pharmaceutical Partners, Los Angeles, CA. USA) or minocycline 100 mg IV q12 h (Minocin, ESI Lederle, Inc., Philadelphia, PA. USA). Duration of therapy was determined by the attending physician based on the patient’s clinical course.
Minocycline or doxycycline therapy was successful in six of seven patients. Eradication of A. baumannii was seen in four of five patients who had a follow-up BAL culture. Two patients (patients 5 and 6) did not have a follow-up BAL performed but improved clinically and were discharged from the hospital. Two of the seven patients died, one of whom was considered a treatment failure (patient 7). This patient had a poor prognosis because of a high initial severity of injury and subsequent septic shock from several sources including VAP and polymicrobial burn wound infections. The other patient who died (patient 4) was considered a microbiologic success because A. baumannii was not found in the follow-up BAL. However, this patient died later in the hospital course from septic shock caused by persistent Pseudomonas aeruginosa VAP. Another patient (patient 3) had a P. aeruginosa VAP superinfection on the follow-up BAL that was successfully treated with cefepime.
Discussion
This is the first report of doxycycline or minocycline therapy for the treatment of multidrug-resistant A. baumannii. These agents were used in this patient group with VAP because the isolates were fully or intermediately resistant to all other drugs, including imipenem-cilastatin and ampicillin-sulbactam. Tetracyclines are not commonly used to treat VAP because they are bacteriostatic agents and lack clinical efficacy data for this indication. Tetracyclines have been reported to have good in vitro activity against A. baumannii [2], although local ICU and interpatient sensitivity patterns will vary. In addition, doxycycline has been shown to be effective, although less so, than imipenem for treating A. baumannii pneumonia in an animal model [4]. Likewise in this small group of patients, minocycline and doxycycline appeared to be effective for A. baumannii VAP.
Strengths of this report include a rigorous definition of VAP that included quantitative cultures from BAL and the use of disk diffusion sensitivity testing. The use of quantitative cultures is important because a purely clinical diagnosis of VAP is poor at differentiating between pneumonia and other clinical states [5]. In addition, five of seven patients had follow-up BALs, the results of which were used in assessing therapy. The use of disk diffusion tests are also important with A. baumannii because automated sensitivity methods may falsely report imipenem resistance.
Three limitations to this report should be noted. First, one patient (patient 4) had polymicrobial VAP with other highly pathogenic organisms (Table 1). Thus, the effect of A. baumannii infection and subsequent minocycline therapy on the clinical course of this patient is unknown. The patient was included in order to complete the reporting of our experience. Microbiologic clearance of A. baumannii from the follow-up BAL in this patient was thought to be noteworthy, even though few data exist on the use of follow-up BALs to monitor VAP therapy.
Second, there is some recent debate regarding the true pathogenicity of A. baumannii. The organism has traditionally been considered to be highly virulent; however, the efficacy of bacteriostatic agents against the organism may be less impressive if A. baumannii is ultimately found to be a relatively weak pathogen. Nonetheless, one patient in this report (patient 7) did die from A. baumannii infections.
Third, the use of combination therapy for A. baumannii in four patients (Tables 1 and 2) is a potentially confounding factor. Two patients received amikacin (patients 3 and 7), one patient received imipenem/cilastatin (patient 2), and one received ampicillin/sulbactam (patient 5). Each isolate was fully or intermediately resistant to these agents. The clinical benefits of combination therapy in these patients are unknown; however, these drug combinations may have resulted in in vivo synergy despite in vitro resistance. Alternatively, there are limited data that show adding amikacin to doxycycline for A. baumannii pneumonia does not improve efficacy compared to doxycycline monotherapy [4]. Indeed, combination therapy has not generally been found to be more effective than monotherapy for gram-negative infections despite widespread recommendations for its use [6, 7, 8, 9].
Current guidelines for the treatment of A. baumannii VAP recommend combination therapy with a beta-lactam plus an aminoglycoside [1]. Specifically, a carbapenem plus amikacin is considered the therapy of choice due to the relatively higher level of resistance to cephalosporins, extended-spectrum penicillins, quinolones, and aminoglycosides [2]. However, imipenem resistance is an emerging problem seen in up to 11% of isolates [2]. Imipenem-resistant organisms are also generally resistant to other drug classes and create a treatment dilemma for which there are few data [10].
Based on three reports, the primary option for treating imipenem-resistant A. baumannii appears to be the sulbactam portion of ampicillin/sulbactam. A recent study suggested that success rates in treating A. baumannii VAP were similar for imipenem-resistant organisms treated with ampicillin-sulbactam compared to imipenem-sensitive organisms treated with imipenem-cilastatin [3]. A similar report concluded that ampicillin-sulbactam was effective in nine of ten patients with lower respiratory tract infections [10]. Likewise, six of eight patients with meningitis were successfully treated with ampicillin/sulbactam plus intrathecal aminoglycosides [11].11 Ampicillin-sulbactam has also been successfully used as an “imipenem-sparing” agent in patients with imipenem-sensitive A. baumannii infections, mostly bacteremias [12, 13, 14]. However, many of these patients were not critically ill.
Intravenous colistin has also been studied for treating imipenem-resistant A. baumannii but with generally poor results. This agent was successful in three case reports; however, it was ineffective and nephrotoxic in a larger report of patients with pneumonia [15, 16, 17, 18]. Another option, aminoglycoside monotherapy, is not generally recommended for treating severe pneumonia because of high failure rates [1]. Aerosolized therapy with aminoglycosides or colistin is likely no more effective than IV therapy of pneumonia based on the few small reports that have been published [19]. Lastly, novel combinations of sulbactam with imipenem or rifampin have been successful in an animal model of resistant A. baumannii, but no clinical data are available [20].
In conclusion, the results of this case series suggest that minocycline or doxycycline may be an effective option for treating imipenem and sulbactam-resistant A. baumannii VAP. Six of seven patients were successfully treated. It is important to study new treatment options for this indication given the high mortality and increasing antibiotic resistance associated with this organism. However, more data are needed to fully determine the role of tetracyclines in treating severe A. baumannii infections.
References
American Thoracic Society (1995) Hospital-acquired pneumonia in adults: diagnosis, assessment of severity, initial antimicrobial therapy, and preventative strategies. A consensus statement. Am J Respir Crit Care Med 153:1711–1725
Gales AC, Jones RN, Forward KR, Linares J, Sader HS, Verhoef J (2001) Emerging importance of multidrug-resistant Acinetobacter species and Stenotrophomonas maltophilia as pathogens in seriously ill patients: Geographic patterns, epidemiological features, and trends in the SENTRY antimicrobial surveillance program (1997–1999). Clin Infect Dis 32(Suppl ii):104–113
Wood GC, Hanes SD, Croce MA, Fabian TC, Boucher BA (2002) Comparison of ampicillin-sulbactam and imipenem-cilastatin for the treatment of Acinetobacter ventilator-associated pneumonia. Clin Infect Dis 34:1425–1430
Rodríguez-Hernández MJ, Pachón J, Pichardo C, Cuberos L, Ibánez-Martínez J, García-Curiel A, Caballero FJ, Moreno I, Jiménez-Mejías ME (2000) Imipenem, doxycycline and amikacin in monotherapy in combination in Acinetobacter baumannii experimental pneumonia. J Antimicrob Chemother 45:493–501
Croce MA, Fabian TC, Waddle-Smith L, Melton SM, Minard G, Kudsk KA, Pritchard FE (1998) Utility of Gram’s stain and efficacy of quantitative cultures for posttraumatic pneumonia: A prospective study. Ann Surg 227:743–755
Leibovici L, Paul M, Poznanski O, Drucker M, Samra Z, Konigsburger H, Pitlik SD (1997) Monotherapy versus lactam-aminoglycoside combination treatment for gram-negative bacteremia: a prospective, observational study. Antimicrob Agents Chemother 41:1127–1133
DuPont H, Carbon C, Carlet J (2000) Monotherapy with a broad-spectrum beta-lactam is as effective as its combination with an aminoglycoside in treatment of severe generalized peritonitis: a multicenter randomized controlled trial. Antimicrob Agents Chemother 44:2028–2033
Cometta A, Baumgartner JD, Lew D, Zimmerli W, Pittet D, Chopart P, Schaad U, Herter C, Eggimann P, Huber O, Ricou B, Suter P, Auckenthaler R, Chiolero R, bille J, Scheidegger C, Frei R, Glauser MP (1994) Prospective randomized comparison of imipenem monotherapy with imipenem plus netilmicin for treatment of severe infections in nonneutropenic patients. Antimicrob Agents Chemother 38:1309–1313
Croce MA, Fabian TC, Stewart RM, Pritchard FE, Minard G, Trenthem L, Kudsk KA (1993) Empiric monotherapy versus combination therapy of nosocomial pneumonia in trauma patients. J Trauma 35:303–311
Urban C, Go E, Mariano N, Berger BJ, Avraham I, Rubin D, Rahal JJ (1993) Effect of sulbactam on infection caused by imipenem-resistant Acinetobacter calcoaceticus biotype anitratus. J Infect Dis 167:448–451
Jiménez-Mejías ME, Pachón J, Becerril B, Palomino-Nicas J, Rodriguez-Cobacho A, Revuelta M (1997) Treatment of multidrug-resistant Acinetobacter baumannii meningitis with ampicillin/sulbactam. Clin Infect Dis 24:932–935
Cisneros JM, Reyes MJ, Pachón J, Becerril B, Caballero FJ, Garcia-Garmendia JL, Ortiz C, Cobacho AR (1996) Bacteremia due to Acinetobacter baumannii: epidemiology, clinical findings, and prognostic features. Clin Infect Dis 22:1026–1032
Jellison TK, McKinnon PS, Rybak MJ (2001) Epidemiology, resistance, and outcomes of Acinetobacter baumannii bactermia treated with imipenem-cilastatin or ampicillin-sulbactam. Pharmacotherapy 21:142–148
Corbella X, Ariza J, Ardanuy C, Vuelta M, Tabau F, Sora M, Pujol M, Gudiol F (1998) Efficacy of sulbactam alone and in combination with ampicillin in nosocomial infections caused by multiresistant Acinetobacter baumannii. J Antimicrob Chemother 42:793–802
Jiménez-Mejías ME, Becerril B, Márquez-Rivas FJ, Pichardo C, Cuberos L, Pachon J (2000) Successful treatment of multidrug-resistant Acinetobacter baumannii meningitis with intravenous colistin sulfomethate sodium. Eur J Clin Microbiol Inf Dis 19:970–971
Wood CA, Reboli AC (1993) Infections caused by imipenem-resistant Acinetobacter calcoaceticus biotype anitratus. J Infect Dis 168:1602–1603
Levin AS, Barone AA, Penço J, Santos MV, Marinho IS, Arruda EA, Manrique EI, Costa SF (1999) Intravenous colistin as therapy for nosocomial infections caused by multidrug-resistant Pseudomonas aeruginosa and Acinetobacter baumannii. Clin Infect Dis 28:1008–1011
Fernandez-Viladrich P, Corbella X, Corral F, Tubau F, Mateu A (1999) Successful treatment of ventriculitis due to carbapenem-resistant Acinetobacter baumannii with intraventricular colistin sulfomethate sodium. Clin Infect Dis 28:916–917
Wood GC, Boucher BA (2000) Aerosolized antimicrobial therapy in acutely ill patients. Pharmacotherapy 20:166–181
Wolff M, Joly-Guillou ML, Farinotti R, Carbon C (1999) In vivo efficacies of combinations of -lactams, -lactamase inhibitors, and rifampin against Acinetobacter baumannii in a mouse pneumonia model. Antimicrob Agents Chemother 43:1406–1411
Author information
Authors and Affiliations
Corresponding author
Additional information
No financial support was used for this report.
Rights and permissions
About this article
Cite this article
Wood, G.C., Hanes, S.D., Boucher, B.A. et al. Tetracyclines for treating multidrug-resistant Acinetobacter baumannii ventilator-associated pneumonia. Intensive Care Med 29, 2072–2076 (2003). https://doi.org/10.1007/s00134-003-1811-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-003-1811-2