Abstract
Objective
Antipyrine metabolism is a "gold standard" measure of mixed cytochrome P450 (CYP) mediated drug metabolism in humans. Cytokines (e.g., interleukin-6) and nitric oxide reduce CYP 450 activity in vitro and in vivo. Because interleukin-6 and nitric oxide production increases in children with sepsis-induced multiple organ failure, we hypothesized impaired CYP 450 mediated drug metabolism in this population.
Methods
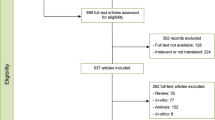
Fifty-one consecutive children with sepsis and six critically ill children without sepsis were enrolled and given 18 mg/kg antipyrine per NG. Plasma antipyrine elimination rate, elimination half-life, and apparent oral clearance were measured and calculated. Plasma interleukin-6 and nitrite plus nitrate levels were measured and organs failing scored on days 1–3 of sepsis.
Results
Children with sepsis had a twofold reduction in antipyrine clearance. Children with persistent failure of three or more organs had a fourfold reduction in antipyrine clearance. Antipyrine clearance was inversely correlated to circulating interleukin-6 and nitrite plus nitrate levels and to number of organ failures.
Conclusions
Interpretation CYP 450 mediated drug metabolism is decreased in children with sepsis, related in part to the degree of inflammation and organ failure. For drugs metabolized by CYP 450 enzymes there is an urgent need to reevaluate the use of standard drug dosage schedules in the sepsis population
Similar content being viewed by others
Introduction
In 1978 Chang et al. [1]. reported a prolonged theophylline elimination rate in patients infected with viral respiratory illness, and in 1982 Kraemer et al. [2] reported 11 cases of theophylline toxicity in children with influenza who had no prior history of difficulty with standard dosing. Injection of experimental animal models with a number of bacterial, viral, and other inflammatory agents has been shown to decrease total cytochrome P450 (CYP) levels and drug metabolizing activity [3, 4]. Inflammation elicits many biological effects by activation of cytokine and nitric oxide production. Abdel-Razzak et al. [5]. reported that interleukin (IL) 1, IL-6, and tumor necrosis factor α are potent depressors of cytochrome P450 mRNA expression and activity in human primary hepatocyte culture. Shedlofsky et al. [6]. reported that adult human volunteers given endotoxin showed a decrease in metabolism of CYP enzyme probe drugs, which included antipyrine (CYP 1A2, 2B6, 2C8, 2C9, 2C18, and 3A4), hexobarbital (CYP 2C19), and theophylline (CYP 1A2, 2E1) [7, 8]. The degree of inhibition of drug metabolism was correlated to the peak circulating plasma level of IL-6 in these endotoxin-treated volunteers. These data showed that in humans the inflammatory response to even a very low dose of lipopolysaccharide significantly decreases hepatic cytochrome P450-mediated drug metabolism. These authors suggested that higher degrees of inflammation could be associated with more profound inhibition of drug metabolism.
Drugs metabolized by the liver are presently being administered to children without regard to levels of inflammation. Although some drugs that are metabolized by the CYP system can be monitored with measurements from the clinical laboratory, technical difficulties dictate that the majority of drugs do not have a definitive monitoring tool. Many drugs can directly cause organ toxicity that can be prevented by careful monitoring and adjustment of dosage intervals and concentrations. It is not known whether failure to adjust drug dosage during states of inflammation results in deleterious effects on organ function from unrecognized toxic levels of medications. The need to address this question is underlined by the observation that a leading cause of mortality in children with inflammation is multiple organ failure (MOF).
We previously reported that children with sepsis-induced inflammation who have circulating plasma levels of IL-6 show more severe and persistent organ failure than children who do not have circulating levels of IL-6 [9]. We also reported that children with higher serum nitrate plus nitrite levels, an indirect measure of nitric oxide production, develop MOF [10]. These observations established a link between the degree of inflammation and the severity of multiple organ dysfunction in children. Since cytokines and NO reduce CYP-mediated metabolism, it is likely that these children with sepsis-induced MOF would show diminished drug metabolizing capacity. We hypothesized that mixed CYP450 mediated drug metabolism, reflected by antipyrine elimination, would be reduced in children with increased inflammation, as measured by increased IL-6 and NO production, and by the development of sepsis-induced MOF.
Methods
This study was approved by the Children's Hospital of Pittsburgh Institutional Review Board. Consecutive children admitted to the intensive care unit with a diagnosis of sepsis were enrolled in the study after written informed consent was obtained. Inclusion criteria were based on those reported by Bone [11]. These criteria include clinical suspicion of sepsis, hyper- or hypothermia (rectal temperature >38.5° or <35°C), tachycardia, and at least one of the following indications of altered organ perfusion and function: altered mental status, hypoxemia, elevated serum lactate level, oliguria, delayed capillary refill (>2 s), and bounding pulses. Patients were excluded if they received any exogenous NO source including inhaled NO, nitroprusside, and/or nitroglycerin during the 3-day study period.
Fifty-one patients were identified and enrolled within 24 h of the diagnosis of sepsis. Their ages ranged from 1 day to 18 years (median 3 years). Culture results were positive for sepsis in 38 children (14 Gram-positive bacteria, 18 Gram-negative bacteria, 9 viral, 3 fungal infections) and negative in 13. In 19 there was no prior medical diagnoses, 6 were newborns, 9 were transplant patients (5 bone marrow transplants, 3 lung transplant, and 1 heart/liver transplant without liver failure), and 17 patients had a variety of medical diagnoses (9 oncology, 3 central nervous system injury, 3 congestive heart failure, 2 bronchopulmonary dysplasia). The overall mortality rate was 14% (7/51).
Each patient was assigned a daily organ failure index (OFI) score for the first 3 days. Patients were assigned 1 point for each organ failure defined as follows:
-
Cardiovascular: mean arterial pressure <5th percentile for age or requirement for vasopressor/inotrope after volume resuscitation
-
Pulmonary: partial pressure arterial oxygen: fraction of inspired oxygen ratio <300 and ventilator requirement
-
Renal: oliguria <1 cc/kg per hour for 8 h if <30 kg or <0.5 cc/kg per hour for 8 h if >30 kg or serum creatinine >1
-
Hematological: prothrombin time, partial thromboplastin time >1.5 times normal and platelet count <100,000
-
Hepatic: alanine aminotransferase, aspartate aminotransferase >100 and total bilirubin >1.0 (bilirubin not scored in neonates)
-
Central nervous system: Glasgow coma scale <12 (in absence of sedation)
Components of the OFI were modified from the multiple organ system failure scoring system for children described by Wilkinson et al. [12] and Proulx et al. [13]. Patients who developed an OFI of 3 or higher that continued to day 3 were considered to have persistent MOF (PMOF). Patients who developed an OFI 3 or higher which resolved to a value lower than 3 by day 3 were considered to have resolved MOF (RMOF). Patients who always had an OFI lower than 3 were considered not to have MOF (NMOF). Concurrent use of CYP450 inhibitors (e.g., ketoconazole, fluconazole, cimetidine, macrolides) and inducers (e.g., rifampin, phenobarbital, carbamazepine, diphenylhydantoin, steroids) was recorded. Six critically ill children without liver disease who were stable after organ transplantation, were the control population.
Patients were given 18 mg/kg antipyrine per NG. Blood samples (1 ml) were obtained at 0, 6, 12, 24, and 48 h. The samples were collected in sodium citrate containing tubes, centrifuged immediately, and the plasma was frozen at −70°C and stored for batch analysis. Antipyrine plasma concentrations were determined using HPLC as previously described [14]. The elimination rate constant (k), elimination half-life (t 1/2=0.693/k), and apparent oral clearance (CL/F=k e×Vd) of antipyrine were calculated using standard methods. Antipyrine volume of distribution was estimated from previous reports and clearance was adjusted to body weight in kilograms [15]. To quantitate the nitrite plus nitrate levels the plasma samples were deproteinized using zinc sulfate at 56° C. The specimens were then either used for direct measurement of plasma nitrite levels or the plasma nitrate was first reduced to nitrite with subsequent nitrite quantitation using the Greiss reaction in a microtiter plate assay as previously described. [16]. IL-6 levels were measured in plasma samples using an enzyme-linked immunosorbent assay kit (R & D Systems, Minneapolis, Minn., USA).
Nonparametric (i.e., ranked) analysis of variance was used to compare differences among groups. Prediction of the development of PMOF or mortality by antipyrine metabolism was determined using a log-linear model followed by either the χ2 Fisher's exact test. Associations between OFI and antipyrine metabolism were examined using ranked regression analysis. Independent associations between cardiovascular, pulmonary, hepatic, renal, hematological, or central nervous system failure and antipyrine metabolism were evaluated using univariate analysis. Significant associations were analyzed controlling for age, hepatic failure, transplant status, and organism using multivariate analyses. Differences were considered significant if the p value was less than 0.05. Statistical analyses were performed using SAS software (SAS Institute, Cary, N.C., USA, 1994).
Results
Antipyrine metabolism was lower in children with sepsis (n=51) than in those without (n=6, p<0.05; Table 1) and was lower in PMOF children (n=17) than in NMOF (n=20, p<0.05) and RMOF children (n=14, p<0.05; Table 2). Nonsurvivors (n=7) had a statistically nonsignificant reduction in antipyrine metabolism; however, this finding needs to be interpreted with caution because the power of the observation was less than 0.80 (Table 3). Univariate analysis revealed an association between reduced antipyrine metabolism and liver, respiratory, and hematological failure (p<0.05). Multivariate logistic regression modeling controlling for age, liver failure, transplantation status, and microbiological cause (fungal, viral, Gram-positive bacteria, and Gram-negative bacteria) showed that reduced antipyrine metabolism continued to predict the development of respiratory and hematological failure (p<0.05). For each 1-h increase in antipyrine half-life there was a 1.04 increase in the odds ratio for development of respiratory and hematological failure. Antipyrine elimination half-life increased with increasing IL-6 levels (day 1 r s=0.38, day 3 r s=0.52), nitrite plus nitrate levels (day 3 r s=0.52), and OFI (day 1 r s=0.31 and day 3 r s=0.46, p<0.05).
Discussion
Cytochrome P450 mediated drug metabolizing enzyme activity was markedly decreased in children with sepsis, particularly in those with MOF. This reduction in activity was related in part to inflammation. Parameters reflecting antipyrine elimination and thus CYP-mediated metabolism were evaluated. There was a twofold decrease in mixed CYP450 metabolizing activity in children with sepsis. There was a fourfold reduction in mixed CYP450 metabolizing activity in children with persistent MOF, and four children had nearly a tenfold reduction in mixed cytochrome P450 drug metabolizing activity. All four of these children had persistent MOF, and three of the four died. These observations are concerning because the children with MOF received multiple cytochrome P450 metabolized medications that were dosed according to a presumed normal CYP activity. These observations suggest the possibility that children with sepsis and organ failure can be subjected to toxic dosing of CYP metabolized medications when standard dose schedules are used.
Antipyrine has been used as a probe of mixed CYP-mediated metabolism in over 67 studies of drug metabolism in children and close to 1,000 studies in humans of all ages. Its advantages as a probe drug to assess CYP activity include complete bioavailability, blood flow independent metabolism, and metabolism by multiple mixed function oxidases including CYP 1A2, 2B6, 2C9, 2C18, and 3A4 [6, 17, 18]. These CYP isozymes are responsible in part for metabolism of as many as 70% of hepatic metabolized drugs.
While antipyrine has been extensively used as a probe of CYP metabolism, there are limitations to its use, including a lack of metabolism by other important CYP enzymes including CYP2D6 and CYP2C19. More importantly, since antipyrine is metabolized by multiple CYP isozymes, clinicians cannot directly extrapolate metabolism of antipyrine to metabolism of a therapeutic agent that is metabolized by specific CYP450 isozymes. For example, one cannot be assured that a twofold reduction in antipyrine metabolism is reflective of a twofold reduction in metabolism of other CYP3A4 substrates (the predominant hepatic isozyme responsible for up to 50% of CYP metabolized drugs). Thus further work using isozyme specific probe drugs is needed in order to determine which CYP isozymes are reduced during inflammation, sepsis, and MOF in children.
While the mechanisms by which inflammation reduces CYP activity are not fully understood, it is clear that cytokines and nitric oxide reduce CYP activity [3, 4, 5]. Muller et al. [19] demonstrated that rats given endotoxin have a reduction in CYP activity, and that pretreatment with l-nitroarginine, an inhibitor of NO synthesis, reduced the production of nitrite plus nitrates and preserved CYP activity. This suggests that NO or its downstream product, the reactive peroxynitrite radical (ONOO), is responsible for reducing CYP activity. Since cytochrome P450 enzymes have a heme moiety, it has been hypothesized that ONOO, produced from the combination of NO and superoxide, could bind to the heme moiety rendering the enzyme inactive. A second ONOO mediated mechanism, protein nitration, has also been reported [20]. These investigators subjected rat microsomes to ONOO and found nitration of a tyrosine residue on CYP2B6. Use of antibody to this residue also reduced metabolism, suggesting that nitration of tyrosine rather than interaction with the heme moiety is the mechanism by which inflammation reduces CYP activity. We found that increased IL-6 and NO production are associated with reduced CYP activity in children with sepsis. This finding supports the cytokine/NO/ONOO mechanistic hypothesis for reduced CYP metabolism during inflammation.
Liver failure results in a reduction in CYP activity because the liver is the predominant source of CYP450 enzyme. Antipyrine metabolism has been successfully used as a measure of liver function and is correlated with clinical scores of liver dysfunction including the Child-Pugh score in adults [21]. We performed our analyses controlling for the presence of liver failure and still found that decreased CYP activity is associated with the development of respiratory and hematological failure. Adults with liver cirrhosis have been reported to have an antipyrine elimination half-life of 37 h [21], well below values observed in some children with MOF without liver failure in our study. Pape et al. [22] were the first to report that reduced CYP metabolism is associated with the development of multiple organ failure in adults without overt liver disease. They showed that reduced metabolism of lidocaine to monoethylglycine-xylidide (CYP3A4 activity) is predictive of trauma-induced MOF. Even though CYP enzymes are predominant in the liver, extrahepatic CYP activity is also abundant in human lung, intestine, kidney, brain, and epithelial tissues. These enzymes are responsible for metabolism of exogenous compounds (xenobiotics) and endogenous compounds including steroids and arachidonic acid. A reduction in extrahepatic CYP enzyme activity could have effects in multiple organs.
CYP activity can be induced or inhibited by environmental, age specific, and genetic factors. Medications can be inhibitors or inducers of CYP isozyme-specific activity. Although we saw no differences in the use of CYP inducers or CYP inhibitors among our patient groups, the number of patients was too small to attain enough power to be certain that these environmental factors played no role in our observations. Age can also affect CYP activity. Children are generally thought to reach full adult CYP activity at 6 months of age. We found that sepsis, inflammation, and organ failure continue to be associated with reduced CYP activity after controlling for age-specific influences. Genetic factors also influence isozyme-specific CYP activity with genetic polymorphisms associated with poor metabolism of CYP2D6, 2C19, and 2C9 substrates. We did not test for these genetic influences.
Another consideration of our study was the use of oral rather than intravenous antipyrine for measurement of antipyrine drug metabolism. Antipyrine is completely (100%) bioavailable in healthy volunteers, but it is still possible that an altered rate of absorption could have affected our results. To control in part for this potential confounding factor we measured antipyrine metabolism over a 48-h period. We observed drug concentration curves consistent with appropriate absorption of the drug and therefore submit that the data accurately reflects CYP-mediated antipyrine metabolism. The administration of the drug per NG also means that small intestine CYP activity may have contributed to our results. CYP3A4 in particular is predominant in the small intestine as well as the liver.
Conclusion
In vitro and in vivo studies have documented that inflammation reduces CYP activity and is associated with the development of organ failure. While present clinical practice adjusts doses of renal eliminated drugs according to creatinine clearance (renal function), CYP metabolized drugs are dosed according to standard schedules without any routine consideration of patient metabolic CYP activity. Our study demonstrates that mixed CYP activity can be reduced two- to tenfold in children with inflammation and organ failure even in the absence of overt liver disease. Therefore there is an urgent need to develop rational drug dosing strategies for critically ill children with reduced drug metabolizing abilities.
References
Chang KC, Bell TD, Lawer BA (1978) Altered theophylline pharmacokinetics during acute respiratory viral illness. Lancet I:1132–1133
Kraemer MJ, Furukawa CT, Kemp JR, Shapiro GG, Pierson WE, Bierman CW (1982) Altered theophylline clearance during an influenza B outbreak. Pediatrics 69:476–480
Morgan ET (1997) Regulation of cytochromes P450 during inflammation and infection. Drug Metab Rev 29:1129–1188
Renton KW (2000) Hepatic drug metabolism and immunostimulation. Toxicology 142:173–178
Abdel Razzak Z, Loyer P, Fautrel A, Gautier JC, Corcos L, Turlin B, Beaune P, Guillozo A (1993) Cytokines down regulate expression of major cytochrome P450 enzymes in adult human hepatocytes in primary culture. Mol Pharmacol 44:707–715
Engel G, Hofmann U, Heidemann H, Cosme J, Eichelbaum M (1996) Antipyrine as a probe for human oxidative drug metabolism: identification of the cytochrome P450 enzymes catalyzing 4-hydroxyantipyrine, 3-hydroxymethylantipyrine, and norantipyrine. Clin Pharmacol Ther 59:613–623
Shedlofsky SI, Israel BC, McClain CJ, Hill DB, Blouin RA (1994) Endotoxin administration to humans inhibits hepatic cytochrome P450 mediated drug metabolism. J Clin Invest 94:2209–2214
Shedlofsky SI, Israel BC, Toleva R, Blouin RA Endotoxin (1997) depresses hepatic CYP 450 mediated drug metabolism in women. Br J Clin Pharmacol 43:627–632
Doughty LA, Kaplan SS, Carcillo JA (1996) Inflammatory cytokine and nitric oxide response in pediatric sepsis and organ failure. Crit Care Med 24:1137–1143
Doughty LA, Carcillo JA, Kaplan SS, Janosky J (1998) Plasma nitrite and nitrate concentration and MOF in pediatric sepsis. Crit Care Med 26:157–162
Bone RC (1990) The sepsis syndrome, definition and general approach to management. Clin Chest Med 17:175–181
Wilkinson JD, Pollack MM, Glass NL, Kanter RR, Katz RW, Steinhart CM (1987) Mortality associated with multiple organ system failure and sepsis in the pediatric intensive care unit. J Pediatr 111:324–328
Proulx F, Fayon M, Farrell CA, LaCroix J, Gauthier M (1996) Epidemiology of sepsis and MODS in children. Chest 109:1033–1037
Matzke GR, Frye RF, Early JJ, Straka RJ, Carson SW (2000) Evaluation of the influence of diabetes mellitus on antipyrine metabolism and CYP1A2 and CYP2D6 activity. Pharmacotherapy 20:182–190
Homeida M, Roberts CJC, Halliwell, Read AE, Branch RA (1979) Antipyrine clearance per unit volume of liver: an assessment of liver function in chronic liver disease Gut 20:596–601
Wong HR, Carcillo JA, Burckart G, Kaplan SS (1996) Nitric oxide production in critically ill patients. Arch Dis Child 74:482–489
Eichelbaum M, Ochs HR, Robertz GM, Somogyi A (1982) Pharmacokinetics and metabolism of antipyrine (phenazone) after intravenous and oral administration. Arzneimittelforschung 32:575–578
Danhof M, Breimer PP (1979) Studies on the different metabolic pathways of antipyrine in man. Br J Pharmacol 8:529–537
Muller CM, Scierka A, Stiller RL, Kim YM, Cook DR, Lancaster JR Jr, Buffington CW, Watkins WD (1996) Nitric oxide mediates hepatic cytochrome P450 dysfunction induced by endotoxin. Anesthesiology 84:1435–1442
Roberts EJ, Lin HI, Crowley JR, Vuletich JL, Osawe Y, Hollenberg PF (1998) Peroxynitrite mediated nitration of tyrosine and inactivation of cytochrome P450 2B1. Chem Res Toxicol 11:1067–1074
St Peter JV, Awni WM (1991) Quantifying hepatic function in the presence of liver disease with phenazone (antipyrine) and its metabolites. Clin Pharmacokinet 20:50–65
Pape D, Lehmann U, Oellerich M, Regal G (1996) Multiple organ failure after severe trauma predicted by the MEGX liver function test? Langenbecks Arch Chir 113:338–339
Author information
Authors and Affiliations
Corresponding author
Additional information
This study was supported in part by NIHRO1GM41734-04A1 and 3M01RR00056GCRC
Rights and permissions
About this article
Cite this article
Carcillo, J.A., Doughty, L., Kofos, D. et al. Cytochrome P450 mediated-drug metabolism is reduced in children with sepsis-induced multiple organ failure. Intensive Care Med 29, 980–984 (2003). https://doi.org/10.1007/s00134-003-1758-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-003-1758-3