Abstract
Objective
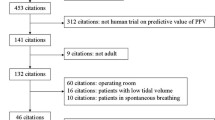
In mechanically ventilated patients the indices which assess preload are used with increasing frequency to predict the hemodynamic response to volume expansion. We discuss the clinical utility and accuracy of some indices which were tested as bedside indicators of preload reserve and fluid responsiveness in hypotensive patients under positive pressure ventilation.
Results and conclusions
Although preload assessment can be obtained with fair accuracy, the clinical utility of volume responsiveness-guided fluid therapy still needs to be demonstrated. Indeed, it is still not clear whether any form of monitoring-guided fluid therapy improves survival.
Similar content being viewed by others
Prediction is very difficult, especially about the future.
Niels Bohr
Introduction
Hypotension is one of the most frequent clinical signs observed in critically ill patients. To restore normal blood pressure, the cardiovascular filling (preload-defined as end-diastolic volume of both ventricular chambers), cardiac function (inotropism), and vascular resistance (afterload) must be assessed. Hemodynamic instability secondary to effective or relative intravascular volume depletion are very common, and intravascular fluid resuscitation or volume expansion (VE) allows restoration of ventricular filling, cardiac output and ultimately arterial blood pressure [1, 2]. However, in the Frank-Starling curve (stroke volume as a function of preload) the slope presents on its early phase a steep portion which is followed by a plateau (Fig. 1). As a consequence, when the plateau is reached, vigorous fluid resuscitation carries out the risk of generating volume overload and pulmonary edema and/or right-ventricular dysfunction. Thus in hypotensive patients methods able to unmask decreased preload and to predict whether cardiac output will increase or not with VE have been sought after for many years. Presently, as few methods are able to assess ventricular volumes continuously and directly, static pressure measurements and echocardiographically measured ventricular end-diastolic areas are used as tools to monitor cardiovascular filling. Replacing static measurements, dynamic monitoring consisting in assessment of fluid responsiveness using changes in systolic arterial pressure, and pulse pressure induced by positive pressure ventilation have been proposed. The present review analyses the current roles and limitations of the most frequently used methods in clinical practice to predict fluid responsiveness in patients undergoing mechanical ventilation (MV) (Table 1).
Representation of Frank-Starling curve with relationship between ventricular preload and ventricular stroke volume in patient X. After volume expansion the same magnitude of change in preload recruit less stroke volume, because the plateau of the curve is reached which characterize a condition of preload independency
One method routinely used to evaluate intravascular volume in hypotensive patients uses hemodynamic response to a fluid challenge [3]. This method consists in infusing a defined amount of fluid over a brief period of time. The response to the intravascular volume loading can be monitored clinically by heart rate, blood pressure, pulse pressure (systolic minus diastolic blood pressure), and urine output or by invasive monitoring with the measurements of the right atrial pressure (RAP), pulmonary artery occlusion pressure (Ppao), and cardiac output. Such a fluid management protocol assumes that the intravascular volume of the critically ill patients can be defined by the relationship between preload and cardiac output, and that changing preload with volume infusion affects cardiac output. Thus an increase in cardiac output following VE (patient responder) unmasks an hypovolemic state or preload dependency. On the other hand, lack of change or a decrease in cardiac output following VE (nonresponding patient) is attributed to a normovolemic, to an overloaded, or to cardiac failure state. Therefore, as the fluid responsiveness defines the response of cardiac output to volume challenge, indices which can predict the latter are necessary.
Static measurements for preload assessment
Measures of intracardiac pressures
According to the Frank-Starling law, left-ventricular preload is defined as the myocardial fiber length at the end of the diastole. In clinical practice, the left-ventricular end-diastolic volume is used as a surrogate to define left-ventricular preload [4]. However, this volumetric parameter is not easily assessed in critically ill patients. In normal conditions, a fairly good correlation exists between ventricular end-diastolic volumes and mean atrial pressures, and ventricular preloads are approximated by RAP and/or Ppao in patients breathing spontaneously [5, 6]. Critically ill patients often require positive pressure ventilation, which modifies the pressure regimen in the thorax in comparison to spontaneous breathing. Indeed, during MV RAP and Ppao rise secondary to an increase in intrathoracic pressure which rises pericardial pressure. This pressure increase induces a decrease in venous return [7, 8] with first a decrease in right and few heart beats later in left-ventricular end-diastolic volumes, respectively [9, 10]. Under extreme conditions such as acute severe pulmonary emboli and/or marked hyperinflation, RAP may also rise secondary to an increase afterload of the right ventricle. Moreover, under positive pressure ventilation not only ventricular but also thoracopulmonary compliances and abdominal pressure variations are observed over time. Thus a variable relationship between cardiac pressures and cardiac volumes is often observed [11, 12, 13, 14]. It has also been demonstrated that changes in intracardiac pressure (RAP, Ppao) no longer directly reflect changes in intravascular volume [15]. Pinsky et al. [16, 17] have demonstrated that changes in RAP do not follow changes in right-ventricular end-diastolic volume in postoperative cardiac surgery patients under positive pressure ventilation. Reuse et al. [18] observed no correlation between RAP and right-ventricular end-diastolic volume calculated from a thermodilution technique in hypovolemic patients before and after fluid resuscitation. The discordance between RAP and right-ventricular end-diastolic volume measurements may result from a systematic underestimation of the effect of positive-pressure ventilation on the right heart [16, 17]. Nevertheless, the RAP value measured either with a central venous catheter or a pulmonary artery catheter is still used to estimate preload and to guide intravascular volume therapy in patient under positive pressure ventilation [19, 20].
On the left side, the MV-induced intrathoracic pressure changes, compared to spontaneously breathing, only minimally alters the relationship between left atrial pressure and left-ventricular end-diastolic volume measurement in postoperative cardiac surgery patients [21]. However, several other studies show no relationship between Ppao and left-ventricular end-diastolic volume measured by either radionuclide angiography [12, 22], transthoracic echocardiography (TTE) [23], or transesophageal echocardiography (TEE) [24, 25, 26]. The latter findings may be related to the indirect pulmonary artery catheter method for assessing left atrial pressure [27, 28], although several studies have demonstrated that Ppao using PAC is a reliable indirect measurement of left atrial pressure [29, 30] in positive-pressure MV patients.
Right atrial pressure used to predict fluid responsiveness
Wagner et al. [31] reported that RAP was significantly lower before volume challenge in responders than in nonresponders (p=0.04) when patients were under positive pressure ventilation. Jellinek et al. [32] found that a RAP lower than 10 mmHg predicts a decrease in cardiac index higher than 20% when a transient 30 cmH2O increase in intrathoracic pressure is administrated. Presuming that the principle cause of decrease in cardiac output in the latter study was due to a reduction in venous return [9, 33, 34, 35], RAP predicts reverse VE hemodynamic effect. Nevertheless, some clinical investigations studying fluid responsiveness in MV patients have reported that RAP poorly predicts increased cardiac output after volume expansion [18, 36, 37]. Indeed, in these studies RAP did not differentiate patients whose cardiac output did or did not increase after VE (responders and nonresponders, respectively).
Ppao used to predict fluid responsiveness
Some studies have demonstrated that Ppao is a good predictor of fluid responsiveness [13, 31, 38]. Recently Bennett-Guerrero et al. [39] also found that Ppao was a better predictor of response to VE than systolic pressure variation (SPV) and left-ventricular end-diastolic area measured by TEE. However, several other studies noted that Ppao is unable to predict fluid responsiveness and to differentiate between VE-responders and VE-nonresponders [18, 25, 36, 37, 40, 41, 42]. The discrepancy between the results of these studies may partly reflect differences in patients' baseline characteristics (e.g., demographic differences, medical history, chest and lung compliances) at study entry. Furthermore, differences in location of the pulmonary artery catheter extremity relative to the left atrium may be present [43]. Indeed, according to its position, pulmonary artery catheter may display alveolar pressure instead of left atrial pressure (West zone I or II) [44]. The value of Ppao is also influenced by juxtacardiac pressure [45, 46] particularly if positive end-expiratory pressure (PEEP) is used [28]. To overcome the latter difficulty in MV patients when PEEP is used, nadir Ppao (Ppao measured after airway disconnection) may be used [46]. However, as nadir Ppao requires temporary disconnection from the ventilator, it might be deleterious to severely hypoxemic patients. No study has yet evaluated the predictive value of nadir Ppao for estimating fluid responsiveness in MV patients.
In brief, although static intracardiac pressure measurements such as RAP and Ppao have been studied and used for many years for hemodynamic monitoring, their low predictive value in estimating fluid responsiveness in MV patients must be underlined. Thus using only intravascular static pressures to guide fluid therapy can lead to inappropriate therapeutic decisions [47].
Measures of ventricular end-diastolic volumes
Radionuclide angiography [48], cineangiocardiography [49], and thermodilution [50] have been used to estimate ventricular volumes for one-half a century. In intensive care units, various methods have been used to measure ventricular end-diastolic volume at the bedside, such as radionuclide angiography [51, 52], TTE [23, 53, 54], TEE [55], and a modified flow-directed pulmonary artery catheter which allows the measurement of cardiac output and right-ventricular ejection fraction (and the calculation of right-ventricular end-systolic and end-diastolic volume) [31, 41].
Right-ventricular end-diastolic volume measured by pulmonary artery catheter used to predict fluid responsiveness
During MV right-ventricular end-diastolic volume measured with a pulmonary artery catheter is decreased by PEEP [56] but is still well correlated with cardiac index [57, 58] and is a more reliable predictor of fluid responsiveness than Ppao [40, 41]. On the other hand, other studies have found no relationship between change in right-ventricular end-diastolic volume measured by pulmonary artery catheter and change in stroke volume in two series of cardiac surgery patients [16, 18]. Similarly, Wagner et al. [31] found that right-ventricular end-diastolic volume measured by pulmonary artery catheter was not a reliable predictor of fluid responsiveness in patients under MV, and that Ppao and RAP were superior to right-ventricular end-diastolic volume. The discrepancy between the results of these studies may partly reflect the measurement errors of cardiac output due to the cyclic change induced by positive pressure ventilation [59, 60, 61, 62], the inaccuracy of cardiac output measurement obtained by pulmonary artery catheter when the flux is low [63], and the influence of tricuspid regurgitation on the measurement of cardiac output [64]. Moreover, as right-ventricular end-diastolic volume is calculated (stroke volume divided by right ejection fraction), cardiac output becomes a shared variable in the calculation of both stroke volume and right-ventricular end-diastolic volume, and a mathematical coupling may have contributed to the close correlation observed between these two variables. Nevertheless, right-ventricular end-diastolic volume compared to Ppao may be useful in a small group of patients with high intra-abdominal pressure or when clinicians are reluctant to obtain off-PEEP nadir Ppao measurements [65]
Right-ventricular end-diastolic volume measured by echocardiography used to predict fluid responsiveness
TTE has been shown to be a reliable method to assess right-ventricular dimensions in patients ventilated with continuous positive airway pressure or positive-pressure ventilation [66, 67]. Using this approach, right-ventricular end-diastolic area is obtained on the apical four chambers view [68]. When no right-ventricular window is available, TEE is preferred to monitor right-ventricular end-volume in MV patients [53, 55, 69, 70, 71]. The latter method has become more popular in recent years due to technical improvements [72]. Nevertheless, no study has evaluated right-ventricular size measurements by TTE or TEE as a predictor of fluid responsiveness in MV patients.
Left-ventricular end-diastolic volume measured by echocardiography used to predict fluid responsiveness
TTE has been used in the past to measure left-ventricular end-diastolic volume and/or area [23, 67, 73, 74] in MV patients. However, no study has evaluated the left-ventricular end-diastolic volume and/or area measured by TTE as predictors of fluid responsiveness in MV patients. Due to its greater resolving power, TEE easily and accurately assesses left-ventricular end-diastolic volume and/or area in clinical practice [53, 75] except in patients undergoing coronary artery bypass grafting [76]. However, different studies have reported conflicting results about the usefulness of left-ventricular end-diastolic volume and/or area measured by TEE to predict fluid responsiveness in MV patients. Cheung et al. [26] have shown that left-ventricular end-diastolic area measured by TEE is an accurate method to predict the hemodynamic effects of acute blood loss. Other studies have reported either a modest [25, 42, 77] or a poor [78, 79] predictive value of left-ventricular end-diastolic volume and area to predict the cardiac output response to fluid loading. Recent studies have also produced conflicting results. Bennett-Guerrero et al. [39] measuring left-ventricular end-diastolic area with TEE before VE found no significant difference between responders and nonresponders. Paradoxically, Reuter et al. [80] found that left-ventricular end-diastolic area index assessed by TEE before VE predicts fluid responsiveness more accurately than RAP, Ppao, and stroke volume variation (SVV). In the future three-dimensional echocardiography could supplant other methods for measuring left-ventricular end-diastolic volume and their predictive value of fluid responsiveness. In a word, although measurements of ventricular volumes should theoretically reflect preload dependence more accurately than other indices, conflicting results have been reported so far. These negative findings may be related to the method used to estimate end-diastolic ventricular volumes which do not reflect the geometric complexity of the right ventricle and to the influences of the positive intrathoracic pressure on left-ventricular preload, afterload and myocardial contractility [81].
Dynamic measurements for preload assessment
Measure of respiratory changes in systolic pressure, pulse pressure, and stroke volume
Positive pressure breath decreases temporary right-ventricular end-diastolic volume secondary to a reduction in venous return [7, 82]. A decrease in right-ventricular stroke volume ensues which become minimal at end positive pressure breath. This inspiratory reduction in right-ventricular stroke volume induces a decrease in left-ventricular end-diastolic volume after a phase lag of few heart beats (due to the pulmonary vascular transit time [83]), which becomes evident during the expiratory phase. This expiratory reduction in left-ventricular end-diastolic volume induces a decrease in left-ventricular stroke volume, determining the minimal value of systolic blood pressure observed during expiration. Conversely, the inspiratory increase in left-ventricular end-diastolic volume determining the maximal value of systolic blood pressure is observed secondary to the rise in left-ventricular preload reflecting the few heart beats earlier increased in right-ventricular preload during expiration. Furthermore, increasing lung volume during positive pressure ventilation may also contribute to the increased pulmonary venous blood flow (related to the compression of pulmonary blood vessels [84]) and/or to a decrease in left-ventricular afterload [85, 86, 87], which together induce an increase in left-ventricular preload. Finally, a decrease in right-ventricular end-diastolic volume during a positive pressure breath may increase left-ventricular compliance and then left-ventricular preload [88]. Thus due to heart-lung interaction during positive pressure ventilation the left-ventricular stroke volume varies cyclically (maximal during inspiration and minimal during expiration).
These variations have been used clinically to assess preload status and predict fluid responsiveness in deeply sedated patients under positive pressure ventilation. In 1983 Coyle et al. [89] in a preliminary study demonstrated that the SPV following one mechanical breath is increased in hypovolemic sedated patients and decreased after fluid resuscitation. This study defined SPV as the difference between maximal and minimal values of systolic blood pressure during one positive pressure mechanical breath. Using the systolic pressure at end expiration as a reference point or baseline the SPV was further divided into two components: an increase (Δup) and a decrease (Δdown) in systolic pressure vs. baseline (Fig. 2). These authors concluded that in hypovolemic patients Δdown was the main component of SPV. These preliminary conclusions were confirmed in 1987 by Perel et al. [90] who demonstrated that SPV following a positive pressure breath is a sensitive indicator of hypovolemia in ventilated dogs. Thereafter Coriat et al. [91] demonstrated that SPV and Δdown predict the response of cardiac index to VE in a group of sedated MV patients after vascular surgery. Exploring another pathophysiological concept, Jardin et al. [92] found that pulse pressure (PP; defined as the difference between the systolic and the diastolic pressure) is related to left-ventricular stroke volume in MV patients. Using these findings, Michard et al. [35, 36,] have shown that respiratory changes in PP [ΔPP=maximal PP at inspiration (PPmax) minus minimal PP at expiration (PPmin); (Fig. 2) and calculated as: ΔPP (%)=100 (PPmax-PPmin)/(Ppmax+PPmin)/2] predict the effect of VE on cardiac index in patients with acute lung injury [35] or septic shock [36]. The same team proposed another approach to assess SVV in MV patients and to predict cardiac responsiveness to VE [79]. Using Doppler measurement of beat-to-beat aortic blood flow, they found that respiratory change in aortic blood flow maximal velocity predicts fluid responsiveness in septic MV patients. Measuring SVV during positive pressure ventilation by continuous arterial pulse contour analysis, Reuter et al. [80] have recently demonstrated that SVV accurately predicts fluid responsiveness following volume infusion in ventilated patients after cardiac surgery.
Systolic pressure variation used to predict fluid responsiveness
The evaluation of fluid responsiveness by SPV is based on cardiopulmonary interaction during MV [93, 94]. In 1995 Rooke et al. [95] found that SPV is a useful monitor of volume status in healthy MV patients during anesthesia. Coriat et al. [91] confirmed the usefulness of SPV for estimating response to VE in MV patients after vascular surgery. Ornstein et al. [96] have also shown that SPV and Δdown are correlated with decreased cardiac output after controlled hemorrhage in postoperative cardiac surgical patients. Furthermore, Tavernier et al. [42] found Δdown before VE to be an accurate index of the fluid responsiveness in septic patients, and that a Δdown value of 5 mmHg is the cutoff point for distinguishing responders from nonresponders to VE. Finally, in septic patients Michard et al. [36] found that SPV is correlated with volume expansion-induced change in cardiac output. However, Denault et al. [81] have demonstrated that SPV is not correlated with changes in left-ventricular end-diastolic volume measured by TEE in cardiac surgery patients. Indeed, in this study, SPV was observed despite no variation in left-ventricular stroke volume, suggesting that SPV involves processes independent of changes in the left-ventricular preload (airway pressure, pleural pressure, and its resultant afterload) [81].
Pulse pressure variation used to predict fluid responsiveness
Extending the concept elaborated by Jardin et al. [92], Michard et al. [36] found that ΔPP predicted the effect of VE on cardiac output in 40 septic shock hypotensive patients. These authors demonstrated that both ΔPP and SPV, when greater than 15%, are superior to RAP and Ppao, for predicting fluid responsiveness. Moreover, ΔPP was more accurate and with less bias than SPV. These authors proposed ΔPP as a surrogate for stroke volume variation concept [93], which has not been validated yet. In another study these authors [35] included VE in six MV patients with acute lung injury and found that ΔPP is a useful guide to predict fluid responsiveness.
Stroke volume variation to predict fluid responsiveness
Using Doppler TEE, Feissel et al. [79] studied changes in left-ventricular stroke volume induced by the cyclic positive pressure breathing. By measuring the respiratory variation in maximal aortic blood flow velocity these authors predicted fluid responsiveness in septic MV patients. Left-ventricular stroke volume was obtained by multiplying flow velocity time integral over aortic valve by valve opening area during expiration. However, this finding may be biased, as expiratory flow velocity time integral is a shared variable in the calculation of both cardiac output and expiratory maximal aortic blood flow velocity and a mathematical coupling may contribute to the observed correlation between changes in cardiac output and variation in maximal aortic blood flow velocity. Finally, Reuter et al. [80] used continuous arterial pulse contour analysis and found that SVV during positive pressure breath accurately predicts fluid responsiveness following VE in ventilated cardiac surgery patients [80]. Using the receiver operating characteristics curve, these authors demonstrated that the area under the curve is statistically greater for SVV (0.82; confidence interval: 0.64–1) and SPV (0.81; confidence interval: 0.62–1) than for RAP (0.45; confidence interval: 0.17–0.74) (p<0.001) [97]. Concisely, dynamic indices have been explored to evaluate fluid responsiveness in critically ill patients. All of them have been validated in deeply sedated patients under positive-pressure MV. Thus such indices are useless in spontaneously breathing intubated patients, a MV mode often used in ICU. Moreover, regular cardiac rhythm is an obligatory condition to allow their use.
Conclusion
Positive pressure ventilation cyclically increases intrathoracic pressure and lung volume, both of which decrease venous return and alter stroke volume. Thus VE which rapidly restore cardiac output and arterial blood pressure is an often used therapy in hypotensive MV patients and indices which would predict fluid responsiveness are necessary. RAP, Ppao, and right-ventricular end-diastolic volume, which are static measurements, have been studied but produced conflicting data in estimating preload and fluid responsiveness. On the other hand, SPV and ΔPP, which are dynamic measurements, have been shown to identify hypotension related to decrease in preload, to distinguish between responders and nonresponders to fluid challenge (Table 1), and to permit titration of VE in various patient populations.
Although there is substantial literature on indices of hypovolemia, only few studies have evaluated the cardiac output changes induced by VE in MV patients. Moreover, therapeutic recommendations regarding unmasked preload dependency states without hypotension need further studies. Finally, another unanswered question is related to patients outcome: does therapy guided by fluid responsiveness indices improve patients survival?
References
Guyton AC, Richardson TQ, Langston JB (1964) Regulation of cardiac output and venous return. Clin Anesth 3:1–34
Guyton AC (1967) Regulation of cardiac output. N Engl J Med 277:805–812
Horst HM, Obeid FN (1986) Hemodynamic response to fluid challenge: a means of assessing volume status in the critically ill. Henry Ford Hosp Med J 34:90–94
Suga H, Sagawa K (1974) Instantaneous pressure-volume relationships and their ratio in the excised, supported canine left ventricle. Circ Res 35:117–126
Crexells C, Chatterjee K, Forrester JS, Dikshit K, Swan HJ (1973) Optimal level of filling pressure in the left side of the heart in acute myocardial infarction. N Engl J Med 289:1263–1266
Buchbinder N, Ganz W (1976) Hemodynamic monitoring: invasive techniques. Anesthesiology 45:146–155
Cournand A, Motley H, Werko L, Richards D (1948) Physiological studies of the effect of intermittent positive pressure breathing on cardiac output in man. Am J Physiol 152:162–174
Fessler HE, Brower RG, Wise RA, Permutt S (1992) Effects of positive end-expiratory pressure on the canine venous return curve. Am Rev Respir Dis 146:4–10
Potkin RT, Hudson LD, Weaver LJ, Trobaugh G (1987) Effect of positive end-expiratory pressure on right and left ventricular function in patients with the adult respiratory distress syndrome. Am Rev Respir Dis 135:307–311
Fewell JE, Abendschein DR, Carlson CJ, Murray JF, Rapaport E (1980) Continuous positive-pressure ventilation decreases right and left ventricular end-diastolic volumes in the dog. Circ Res 46:125–132
McKenney PA, Apstein CS, Mendes LA, Connelly GP, Aldea GS, Shemin RJ, Davidoff R (1994) Increased left ventricular diastolic chamber stiffness immediately after coronary artery bypass surgery. J Am Coll Cardiol 24:1189–1194
Calvin JE, Driedger AA, Sibbald WJ (1981) Does the pulmonary capillary wedge pressure predict left ventricular preload in critically ill patients? Crit Care Med 9:437–443
Packman MI, Rackow EC (1983) Optimum left heart filling pressure during fluid resuscitation of patients with hypovolemic and septic shock. Crit Care Med 11:165–169
Jardin F, Gueret P, Dubourg O, Farcot JC, Margairaz A, Bourdarias JP (1985) Right ventricular volumes by thermodilution in the adult respiratory distress syndrome. A comparative study using two-dimensional echocardiography as a reference method. Chest 88:34–39
Lichtwarck-Aschoff M, Zeravik J, Pfeiffer UJ (1992) Intrathoracic blood volume accurately reflects circulatory volume status in critically ill patients with mechanical ventilation. Intensive Care Med 18:142–147
Pinsky MR, Desmet JM, Vincent JL (1992) Effect of positive end-expiratory pressure on right ventricular function in humans. Am Rev Respir Dis 146:681–687
Pinsky MR (1994) Cardiovascular effects of ventilatory support and withdrawal. Anesth Analg 79:567–576
Reuse C, Vincent JL, Pinsky MR (1990) Measurements of right ventricular volumes during fluid challenge. Chest 98:1450–1454
Saarela E, Kari A, Nikki P, Rauhala V, Iisalo E, Kaukinen L (1991) Current practice regarding invasive monitoring in intensive care units in Finland. A nationwide study of the uses of arterial, pulmonary artery and central venous catheters and their effect on outcome. The Finnish Intensive Care Study Group. Intensive Care Med 17:264–271
Boldt J, Lenz M, Kumle B, Papsdorf M (1998) Volume replacement strategies on intensive care units: results from a postal survey. Intensive Care Med 24:147–151
Guyton RA, Chiavarelli M, Padgett CA, Cheung EH, Staton GW, Hatcher CR (1987) The influence of positive end-expiratory pressure on intrapericardial pressure and cardiac function after coronary artery bypass surgery. J Cardiothorac Anesth 1:98–107
Lemaire F, Teboul JL, Cinotti L, Giotto G, Abrouk F, Steg G, Macquin-Mavier I, Zapol WM (1988) Acute left ventricular dysfunction during unsuccessful weaning from mechanical ventilation. Anesthesiology 69:171–179
Jardin F, Valtier B, Beauchet A, Dubourg O, Bourdarias JP (1994) Invasive monitoring combined with two-dimensional echocardiographic study in septic shock. Intensive Care Med 20:550–554
Hinder F, Poelaert JI, Schmidt C, Hoeft A, Mollhoff T, Loick HM, Van Aken H (1998) Assessment of cardiovascular volume status by transoesophageal echocardiography and dye dilution during cardiac surgery. Eur J Anaesthesiol 15:633–640
Tousignant CP, Walsh F, Mazer CD (2000) The use of transoesophageal echocardiography for preload assessment in critically ill patients. Anesth Analg 90:351–355
Cheung AT, Savino JS, Weiss SJ, Aukburg SJ, Berlin JA (1994) Echocardiographic and hemodynamic indexes of left ventricular preload in patients with normal and abnormal ventricular function. Anesthesiology 81:376–387
Swan HJ, Ganz W, Forrester J, Marcus H, Diamond G, Chonette D (1970) Catheterization of the heart in man with use of a flow-directed balloon-tipped catheter. N Engl J Med 283:447–451
Berryhill RE, Benumof JL (1979) PEEP-induced discrepancy between pulmonary arterial wedge pressure and left atrial pressure: the effects of controlled vs. spontaneous ventilation and compliant vs. noncompliant lungs in the dog. Anesthesiology 51:303–308
Humphrey CB, Gibbons JA, Folkerth TL, Shapiro AR, Fosburg RG (1976) An analysis of direct and indirect measurements of left atrial filling pressure. J Thorac Cardiovasc Surg 71:643–647
Lozman J, Powers SR Jr, Older T, Dutton RE, Roy RJ, English M, Marco D, Eckert C (1974) Correlation of pulmonary wedge and left atrial pressures. A study in the patient receiving positive end expiratory pressure ventilation. Arch Surg 109:270–277
Wagner JG, Leatherman JW (1998) Right ventricular end-diastolic volume as a predictor of the hemodynamic response to a fluid challenge. Chest 113:1048–1054
Jellinek H, Krafft P, Fitzgerald RD, Schwarz S, Pinsky MR (2000) Right atrial pressure predicts hemodynamic response to apneic positive airway pressure. Crit Care Med 28:672–688
Van Trigt P, Spray TL, Pasque MK, Peyton RB, Pellom GL, Christian CM, Fagraeus L, Wechsler AS (1982) The effect of PEEP on left ventricular diastolic dimensions and systolic performance following myocardial revascularization. Ann Thorac Surg 33:585–5892
Johnston WE, Vinten-Johansen J, Santamore WP, Case LD, Little WC (1989) Mechanism of reduced cardiac output during positive end-expiratory pressure in the dog. Am Rev Respir Dis 140:1257–1264
Michard F, Chemla D, Richard C, Wysocki M, Pinsky MR, Lecarpentier Y, Teboul JL (1999) Clinical use of respiratory changes in arterial pulse pressure to monitor the hemodynamic effects of PEEP. Am J Respir Crit Care Med 159:935–939
Michard F, Boussat S, Chemla D, Anguel N, Mercat A, Lecarpentier Y, Richard C, Pinsky, MR, Teboul JL (2000) Relation between respiratory changes in arterial pulse pressure and fluid responsiveness in septic patients with acute circulatory failure. Am J Respir Crit Care Med 162:134–138
Calvin JE, Driedger AA, Sibbald WJ (1981) The hemodynamic effect of rapid fluid infusion in critically ill patients. Surgery 90:61–76
Krausz MM, Perel A, Eimerl D, Cotev S (1977) Cardiopulmonary effects of volume loading in patients in septic shock. Ann Surg 185:429–434
Bennett-Guerrero E, Kahn RA, Moskowitz DM, Falcucci O, Bodian CA (2002) Comparison of arterial systolic pressure variation with other clinical parameters to predict the response to fluid challenges during cardiac surgery. Mt Sinai J Med 69:96–100
Diebel LN, Wilson RF, Tagett MG, Kline RA (1992) End-diastolic volume. A better indicator of preload in the critically ill. Arch Surg 127:817–821
Diebel L, Wilson RF, Heins J, Larky H, Warsow K, Wilson S (1994) End-diastolic volume versus pulmonary artery wedge pressure in evaluating cardiac preload in trauma patients. J Trauma 37:950–955
Tavernier B, Makhotine O, Lebuffe G, Dupont J, Scherpereel P (1998) Systolic pressure variation as a guide to fluid therapy in patients with sepsis-induced hypotension. Anesthesiology 89:1313–1321
Rajacich N, Burchard KW, Hasan FM, Singh AK (1989) Central venous pressure and pulmonary capillary wedge pressure as estimates of left atrial pressure: effects of positive end-expiratory pressure and catheter tip malposition. Crit Care Med 17:7–11
Shasby DM, Dauber IM, Pfister S (1981) Swan-Ganz catheter location and left atrial pressure determine the accuracy of the wedge pressure when positive end-expiratory pressure is used. Chest 80:666–670
Raper R, Sibbald WJ (1986) Misled by the wedge? The Swan-Ganz catheter and left ventricular preload. Chest 89:427–434
Pinsky M, Vincent JL, De Smet JM (1991) Estimating left ventricular filling pressure during positive end-expiratory pressure in humans. Am Rev Respir Dis 143:25–31
Swenson JD, Bull D, Stringham J (2001) Subjective assessment of left ventricular preload using transesophageal echocardiography: corresponding pulmonary artery occlusion pressures. J Cardiothorac Vasc Anesth 15:580–583
Mullins CB, Mason DT, Ashburn WL, Ross J (1969) Determination of ventricular volume by radioisotope-angiography. Am J Cardiol 24:72–78
Kasser IS, Kennedy JW (1969) Measurement of left ventricular volumes in man by single-plane cineangiocardiography. Invest Radiol 4:83–90
Balcon R, Oram S (1968) Measurement of right ventricular end-systolic and end-diastolic volumes by the thermodilution technique. Br Heart J 30:690–695
Viquerat CE, Righetti A, Suter PM (1983) Biventricular volumes and function in patients with adult respiratory distress syndrome ventilated with PEEP. Chest 83:509–514
Dhainaut JF, Devaux JY, Monsallier JF, Brunet F, Villemant D, Huyghebaert MF (1986) Mechanisms of decreased left ventricular preload during continuous positive pressure ventilation in ARDS. Chest 90:74–80
Terai C, Uenishi M, Sugimoto H, Shimazu T, Yoshioka T, Sugimoto T (1985) Transesophageal echocardiographic dimensional analysis of four cardiac chambers during positive end-expiratory pressure. Anesthesiology 63:640–646
Jardin F, Brun-Ney D, Hardy A, Aegerter P, Beauchet A, Bourdarias JP (1991) Combined thermodilution and two-dimensional echocardiographic evaluation of right ventricular function during respiratory support with PEEP. Chest 99:162–168
Vieillard A, Schmitt JM, Beauchet A, Augarde R, Prin S, Page B, Jardin F (2001) Early preload adaptation in septic shock? A transesophageal echocardiographic study. Anesthesiology 94:400–406
Jellinek H, Krafft P, Hiesmayr M, Steltzer H (1997) Measurement of right ventricular performance during apnea in patients with acute lung injury. J Trauma 42:1062–1067
Diebel LN, Myers T, Dulchavsky S (1997) Effects of increasing airway pressure and PEEP on the assessment of cardiac preload. J Trauma 42:585–590–
Cheatham ML, Nelson LD, Chang MC, Safcsak K (1998) Right ventricular end-diastolic volume index as a predictor of preload status in patients on positive end-expiratory pressure. Crit Care Med 26:1801–186
Jansen JR, Schreuder JJ, Bogaard JM, van Rooyen W, Versprille A (1981) Thermodilution technique for measurement of cardiac output during artificial ventilation. J Appl Physiol 51:584–591
Stevens JH, Raffin TA, Mihm FG, Rosenthal MH, Stetz CW (1985) Thermodilution cardiac output measurement. Effects of the respiratory cycle on its reproducibility. JAMA 253:2240–2242
Okamoto K, Komatsu T, Kumar V, Sanchala V, Kubal K, Bhalodia R, Shibutani K (1986) Effects of intermittent positive-pressure ventilation on cardiac output measurements by thermodilution. Crit Care Med 14:977–980
Jansen JR, Schreuder JJ, Settels JJ, Kloek JJ, Versprille A (1990) An adequate strategy for the thermodilution technique in patients during mechanical ventilation. Intensive Care Med 16:422–425
Siniorakis EE, Nikolaou NI, Sarantopoulos CD, Sotirelos KT, Iliopoulos NE, Bonoris PE (1994) Volume loading in predominant right ventricular infarction: bedside haemodynamics using rapid response thermistors. Eur Heart J 15:1340–1347
Spinale FG, Mukherjee R, Tanaka R, Zile MR (1992) The effects of valvular regurgitation on thermodilution ejection fraction measurements. Chest 101:723–731
Yu M, Takiguchi S, Takanishi D, Myers S, McNamara JJ (1995) Evaluation of the clinical usefulness of thermodilution volumetric catheters. Crit Care Med 23:681–686
Jardin F, Farcot JC, Gueret P, Prost JF, Ozier Y, Bourdarias JP (1984) Echocardiographic evaluation of ventricles during continuous positive airway pressure breathing. J Appl Physiol 56:619–627
Huemer G, Kolev N, Kurz A, Zimpfer M (1994) Influence of positive end-expiratory pressure on right and left ventricular performance assessed by Doppler two-dimensional echocardiography. Chest 106:67–73
Jardin F, Dubourg O, Bourdarias JP (1997) Echocardiographic pattern of acute cor pulmonale. Chest 111:209–217
Mathru M, Kleinman B, Dries DJ, Rao T, Calandra D (1990) Effect of opening the pericardium on right ventricular hemodynamics during cardiac surgery. Chest 98:120–123
Schuster S, Erbel R, Weilemann LS, Lu WY, Henkel B, Wellek S, Schinzel H, Meyer J (1990) Hemodynamics during PEEP ventilation in patients with severe left ventricular failure studied by transesophageal echocardiography. Chest 97:1181–1189
Le Tulzo Y, Seguin P, Gacouin A, Camus C, Suprin E, Jouannic I, Thomas R (1997) Effects of epinephrine on right ventricular function in patients with severe septic shock and right ventricular failure: a preliminary descriptive study. Intensive Care Med 23:664–670
Vignon P, Mentec H, Terre S, Gastinne H, Gueret P, Lemaire F (1994) Diagnostic accuracy and therapeutic impact of transthoracic and transesophageal echocardiography in mechanically ventilated patients in the ICU. Chest 106:1829–1834
Jardin F, Brun-Ney D, Auvert B, Beauchet A, Bourdarias JP (1990) Sepsis-related cardiogenic shock. Crit Care Med 18:1055–1060
Jardin F, Fourme T, Page B, Loubieres Y, Vieillard-Baron A, Beauchet A, Bourdarias JP (1999) Persistent preload defect in severe sepsis despite fluid loading: a longitudinal echocardiographic study in patients with septic shock. Chest 116:1354–1359
Clements FM, Harpole DH, Quill T, Jones RH, McCann RL (1990) Estimation of left ventricular volume and ejection fraction by two-dimensional transoesophageal echocardiography: comparison of short axis imaging and simultaneous radionuclide angiography. Br J Anaesth 64:331–336
Urbanowicz JH, Shaaban MJ, Cohen NH, Cahalan MK, Botvinick EH, Chatterjee K, Schiller NB, Dae MW, Matthay MA (1990) Comparison of transesophageal echocardiographic and scintigraphic estimates of left ventricular end-diastolic volume index and ejection fraction in patients following coronary artery bypass grafting. Anesthesiology 72:607–612
van Daele ME, Trouwborst A, van Woerkens LC, Tenbrinck R, Fraser AG, Roelandt JR (1994) Transesophageal echocardiographic monitoring of preoperative acute hypervolemic hemodilution. Anesthesiology 81:602–609
Greim CA, Roewer N, Apfel C, Laux G, Schulte am Esch J (1997) Relation of echocardiographic preload indices to stroke volume in critically ill patients with normal and low cardiac index. Intensive Care Med 23:411–416
Feissel M, Michard F, Mangin I, Ruyer O, Faller JP, Teboul JL (2001) Respiratory changes in aortic blood velocity as an indicator of fluid responsiveness in ventilated patients with septic shock. Chest 119:867–873
Reuter DA, Felbinger TW, Schmidt C, Kilger E, Goedje O, Lamm P, Goetz AE (2002) Stroke volume variations for assessment of cardiac responsiveness to volume loading in mechanically ventilated patients after cardiac surgery. Intensive Care Med 28:392
Denault AY, Gasior TA, Gorcsan J, 3rd, Mandarino WA, Deneault LG, Pinsky MR (1999) Determinants of aortic pressure variation during positive-pressure ventilation in man. Chest 116:176–186
Morgan BC, Martin WE, Hornbein TF, Crawford EW, Guntheroth WG (1966) Hemodynamic effects of intermittent positive pressure respiration. Anesthesiology 27:584–590
Scharf SM, Brown R, Saunders N, Green LH (1980) Hemodynamic effects of positive-pressure inflation. J Appl Physiol 49:124–131
Brower R, Wise RA, Hassapoyannes C, Bromberger-Barnea B, Permutt S (1985) Effect of lung inflation on lung blood volume and pulmonary venous flow. J Appl Physiol 58:954–963
Abel JG, Salerno TA, Panos A, Greyson ND, Rice TW, Teoh K, Lichtenstein SV (1987) Cardiovascular effects of positive pressure ventilation in humans. Ann Thorac Surg 43:198–206
Fessler HE, Brower RG, Wise RA, Permutt S (1988) Mechanism of reduced LV afterload by systolic and diastolic positive pleural pressure. J Appl Physiol 65:1244–1250
Pinsky MR, Matuschak GM, Klain M (1985) Determinants of cardiac augmentation by elevations in intrathoracic pressure. J Appl Physiol 58:1189–1198
Taylor RR, Covell JW, Sonnenblick EH, Ross J (1967) Dependence of ventricular distensibility on filling of the opposite ventricle. Am J Physiol 213:711–718
Coyle JP, Teplick RS, Michael CL, Davison JK (1983) Respiratory variations in systemic arterial pressure as an indicator of volume status. Anesthesiology 59:A53
Perel A, Pizov R, Cotev S (1987) Systolic blood pressure variation is a sensitive indicator of hypovolemia in ventilated dogs subjected to graded hemorrhage. Anesthesiology 67:498–502
Coriat P, Vrillon M, Perel A, Baron JF, Le Bret F, Saada M, Viars P (1994) A comparison of systolic blood pressure variations and echocardiographic estimates of end-diastolic left ventricular size in patients after aortic surgery. Anesth Analg 78:46–53
Jardin F, Farcot JC, Gueret P, Prost JF, Ozier Y, Bourdarias JP (1983) Cyclic changes in arterial pulse during respiratory support. Circulation 68:266–274
Michard F, Teboul JL (2000) Using heart-lung interactions to assess fluid responsiveness during mechanical ventilation. Crit Care 4:282–289
Gunn SR, Pinsky MR (2001) Implications of arterial pressure variation in patients in the intensive care unit. Curr Opin Crit Care 7:212–217
Rooke GA, Schwid HA, Shapira Y (1995) The effect of graded hemorrhage and intravascular volume replacement on systolic pressure variation in humans during mechanical and spontaneous ventilation. Anesth Analg 80:925–932
Ornstein E, Eidelman LA, Drenger B, Elami A, Pizov R (1998) Systolic pressure variation predicts the response to acute blood loss. J Clin Anesth 10:137–140
Reuter DA, Felbinger TW, Kilger E, Schmidt C, Lamm P, Goetz AE (2002) Optimising fluid therapy in mechanically ventilated patients after cardiac surgery by on-line monitoring of left ventricular stroke volume variations. Comparison with aortic systolic pressure variations. Br J Anaesth 88:124–126
Acknowledgements
The authors thank Dr. M.R. Pinsky, University of Pittsburgh Medical Center, for his helpful advice in the preparation of this manuscript. The authors are also grateful for the translation support provided by Angela Frei.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bendjelid, K., Romand, JA. Fluid responsiveness in mechanically ventilated patients: a review of indices used in intensive care. Intensive Care Med 29, 352–360 (2003). https://doi.org/10.1007/s00134-002-1615-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-002-1615-9